Playlist
Show Playlist
Hide Playlist
Scarlet Fever and Rheumatic Fever in Children
-
Slides SFandRF Pediatrics.pdf
-
Download Lecture Overview
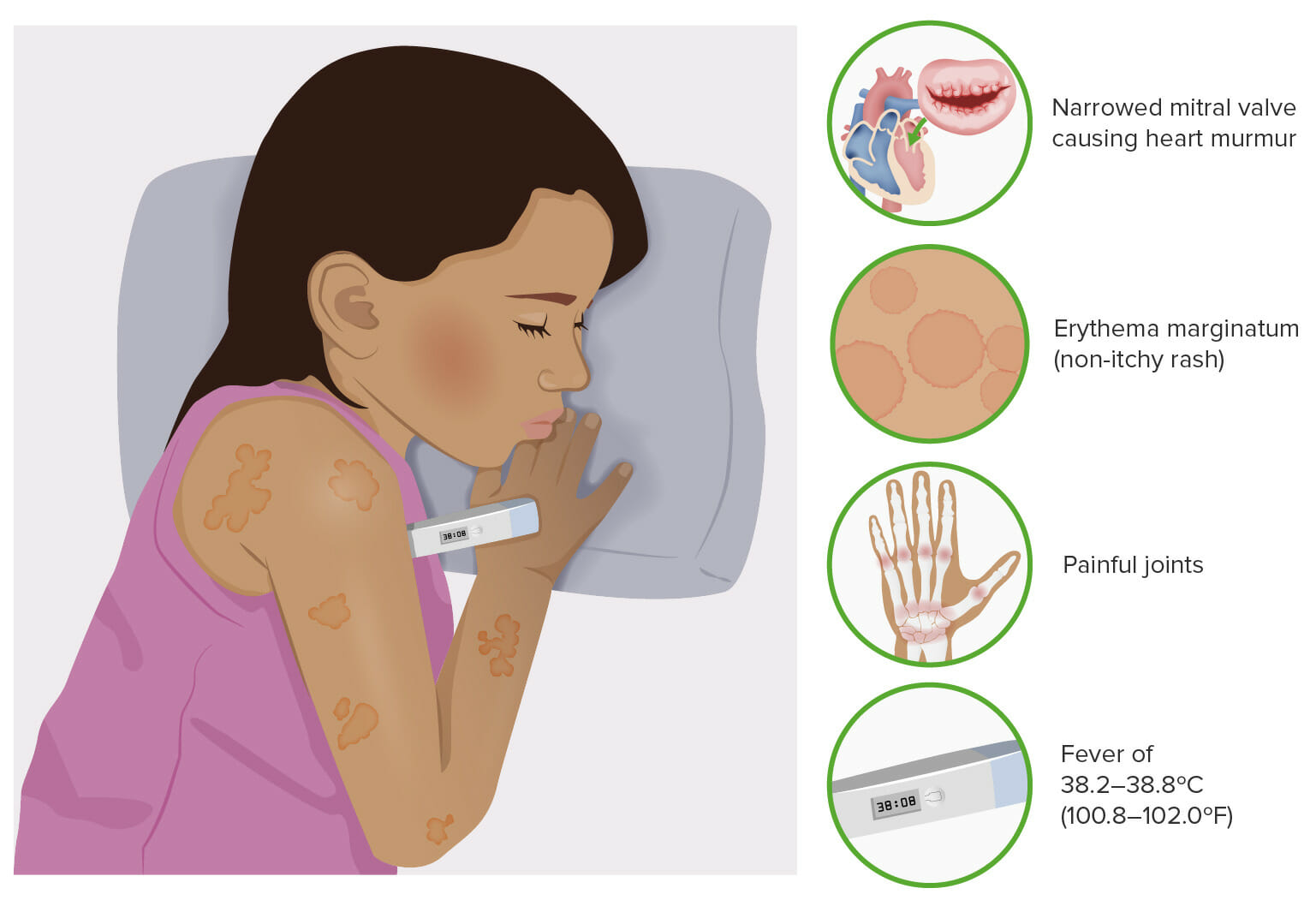
00:00 In this lecture, we’re going to discuss sequelae of group A Strep. In one case, it’s a toxin and in the other case it’s an autoimmune response. We’re going to talk about scarlet fever and rheumatic fever. So let’s start with scarlet fever. Scarlet fever is associated with a group A Strep pharyngitis. It’s a toxin-mediated rash and the rash may appear either before or up to 7 days after the infection but usually 1 or 2 days after the sore throat symptoms begin. Here is an example of a patient with a typical scarlet fever rash. It’s a red confluent what we call sandpaper-like rash. It’s rough to the touch. Patients may have hyperemic lines in their axillae and their groin which we call Pastia lines. These may show up in this case. Patients may also have a strawberry tongue or a very bright red tongue with little bumps. Afterwards, patient often have peeling of their fingers and toes. So you might want to warn them about that as a sequelae a little bit later on. Scarlet fever is usually a clinical diagnosis. Although a rapid Strep test is usually positive, blood testing is generally unhelpful. To treat scarlet fever, we simply treat the Strep throat. We give patients generally amoxicillin or penicillin for a 10-day course. 01:28 Older children can definitely take oral penicillin but younger children we typically give the amoxicillin because the liquid penicillin generally tastes pretty bad. Now, that simple disease is to be distinguished from this autoimmune disease which happens after the infection. So this is rheumatic fever. In this case, symptoms begin after usually an untreated case of Strep throat. Usually this happens in children between the ages of 5 and 18 and certainly not in children under 2. So under 2, we really don’t have to worry about rheumatic fever. This disease is extremely rare in the United States. It is a post-streptococcal consequence to an untreated group A Strep pharyngitis. So treatment prevents this consequence and it’s an autoimmune disease, it’s antibody-mediated. So, to remember this disease, we classically have gone through the major criteria, let’s go through what they are. They’re called the Jones criteria and we can remember the Jones criteria because each letter in the word Jones counts as one of the major criteria but you have to make the O a little heart instead. Watch with me. The J stands for joints. These patients have arthritis. The O which is drawn as a heart stands for cardiac. Any part of the heart can be involved. It can be endocarditis, myocarditis, or pericarditis. N is for nodules. These are firm subcutaneous nodules. E is for erythema marginatum which is a rash that these patients will have and S is Sydenham’s chorea which all by itself with evidence of having had a group A Strep infection is diagnostic for the condition. 03:16 So, let’s go through this major criteria carefully, joints. This is typically a polyarticular, migratory arthritis that usually affects the large joints like the knees, ankles and elbows. 03:31 Typically, these joints like in this drawing are red, tender and swollen and you should know an effusion on your exam. If it’s just pain but no effusion, this technically isn’t an arthritis but it’s rather an arthralgia which is actually one of the minor criteria but is not a major criteria. Also, the pain tends to respond well to NSAIDS. The carditis, 80% of patients with rheumatic fever will have a carditis, most commonly an endocarditis. The endocarditis is an attack on the valves of the heart and it generally causes valvular insufficiency and stenosis as you can see in this picture. Pathologist might describe this as a fish mouth appearance. Generally, the mitral valve is the most common valve affected followed by the tricuspid, followed by the other valves. 04:27 Alternatively, patients may develop a myocarditis which is an inflammation like you can see here on the muscle fibers of the heart. This can result in conduction arrhythmias and can result in congestive heart failure from an ineffective pumping of the heart. Lastly, patients may develop a pericarditis which is typically presented as a pericardial effusion. When you listen to these patients, this is when you can hear that famous friction rub which is such a distinctive sound it’s fairly hard to miss. Subcutaneous nodules are relatively rare. They only happen in about 2% of cases. These are, as you can see in this picture, little pea-sized nodules that are usually over small joints in extremity surfaces of joints. They are firm, they are non-tender, often around the wrists, ankles, or over the knee joints or sometimes rarely over the spine. So you should inspect the spine of any patient where you’re concerned about rheumatic fever. The rash is called erythema marginatum and you can see it pictured here. It’s generally around or annular rash with a clear center and usually overlapping circles in small bunches. This is classic for this disease, erythema marginatum. The S is Sydenham’s chorea. If present, you don’t need any other criteria to make the diagnosis as long as they have evidence for a Strep infection such as an ASO titer. For any child who has choreiform activity and history of recent Strep infection, that’s likely what’s going on. It may be a subtle choreiform activity such as worsening handwriting but usually it’s not, usually it’s fairly obvious and it usually presents later than other major criteria so the evidence of Strep infection would be a little bit more distant. The minor criteria are others and they’re fairly nonspecific things like fever, arthralgia, elevated sed rate or CRP, or, and this is one to remember, a prolonged PR interval or AV block. So for these patients, we may get an EKG as well to make the diagnosis. So how do we diagnose rheumatic fever? Well, first they need evidence of a recent Strep infection that can be a rapid Strep, an ASO titer, or the anti-DNAse B. Second, they need either 2 major criteria or 1 minor criteria, or 1 major criteria or 2 minor criteria, or Sydenham’s chorea alone and if they have these things plus the evidence of the Strep infection, you’ve made your diagnosis of rheumatic fever. So there’s no test we can do. The rheumatoid titer does not help at all. How do we treat? We treat immediately for a 10-day course to prevent any more ongoing antibody production from occurring. So we’re going to treat these patients with amoxicillin or penicillin. In patients with heart disease, this may require prophylaxis with daily amox or monthly penicillin for decades. Nobody is really sure how long we have to prophylax but the concern is this that if they get another Strep throat infection, there are risks for remounting their antibody response and exacerbating their more significant concerns such as endocarditis. In general for the heart disease, we will give them supportive care such as digoxin or antiarrhythmics and in severe cases they may require a transplant. 08:17 So that’s my summary of group A Strep-induced diseases specifically scarlet fever and rheumatic fever. Thanks for your attention.
About the Lecture
The lecture Scarlet Fever and Rheumatic Fever in Children by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Scarlet Fever
- Pathology of Rheumatic Fever
- Clinical Presentation of Rheumatic Fever
- Diagnosis and Management of Rheumatic Fever
Included Quiz Questions
Which of the following is the treatment of scarlet fever?
- Amoxicillin for 10 days
- Ciprofloxacin for 10 days
- Amoxicillin for 5 days
- Ciprofloxacin for 5 days
- Azithromycin for 10 days
Which of the following is a major criteria used to diagnose rheumatic fever?
- Pericarditis
- Erythema multiforme
- Sjogren’s syndrome
- Sore throat
- Hepatitis
Which of the following is NOT a feature of scarlet fever?
- Conjunctivitis
- Sandpaper rash
- Strawberry tongue
- Pastia's lines
- Peeling of fingers and toes
Which of the following is enough to diagnose rheumatic fever when there is evidence of a recent streptococcal infection?
- Sydenham's chorea
- Fever
- Erythema multiforme
- Migratory monoarthritis
- Increased ESR
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly liked the remarks concerning the taste of penicillin and the clear explanation concerning the Jones criteria.
Concise, Succinct, and "digestible" I now know about scarlet & rheumatic fever in children.