Playlist
Show Playlist
Hide Playlist
Renovascular Disease: Clinical Features and Treatment – Secondary Hypertension
-
Slides Secondary Hypertension.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
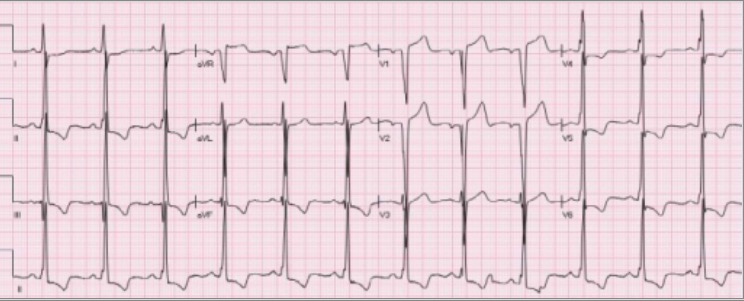
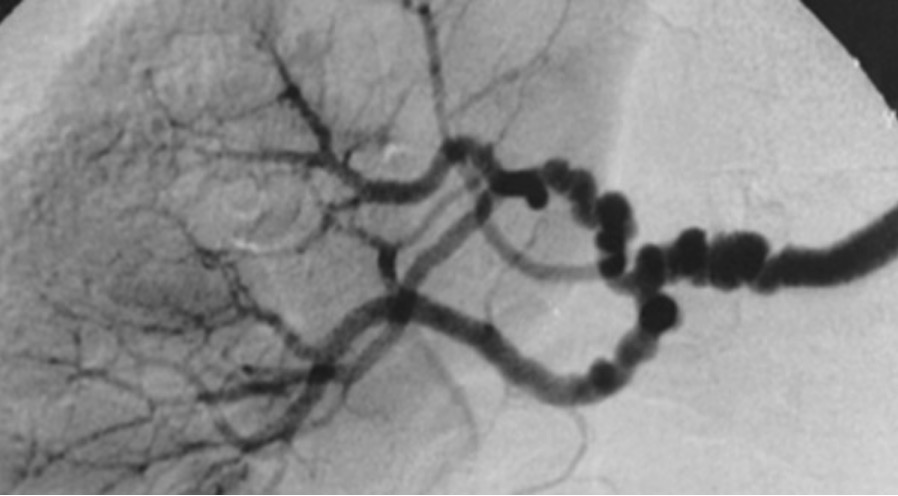
00:01 So, when we think about, kind of, how the clinical features present in our patients who have renovascular disease, for fibromuscular dysplasia, the onset of hypertension is typically much younger, between that 3rd and 5th decade, although there are some people who can present a little bit later. 00:18 In our patients with atherosclerotic disease, they're almost certainly of an older age, typically older than the age of 55. 00:26 Often times, our patients are going to present with sudden onset of uncontrolled hypertension, perhaps in a previously well-controlled patient, or they can present with accelerated or malignant hypertension. 00:39 That means that hypertension is in association with end-organ damage. 00:44 And occasionally, if you have something like bilateral renal artery stenosis, our patients can present with intermittent pulmonary edema despite a normal cardiac function. 00:55 So, if we suspect this and that patient is sitting in front of us, what kind of investigations can we do? We should be on the lookout for an epigastric bruit on physical exam. 01:05 It's not always present but sometimes helpful when it is. 01:08 If somebody has, perhaps, acute, unexplained rise in serum creatinine induced by ACE inhibitors or angiotensin receptor blockers, I just want to take a moment to explain why that happens. 01:18 Remember where ACE inhibitors and angiotensin receptor blockers work? They're actually working at the efferent arteriole causing vasodilation. 01:26 When you have vasodilation, that's gonna decrease the hydrostatic pressure. 01:30 If I already have a reduced efferent arteriole pressure coming in because of my renal artery stenosis or renovascular disease, I could really substantially drop GFR, therefore I have a rise in creatinine. 01:42 It's also helpful if you see an asymmetric renal size on imaging, particularly in atherosclerotic renal vascular disease. 01:51 So, often times, you might see a very small kidney in the affected arterial bed where there's atherosclerotic disease. 01:58 So, what about physical exam? As we mentioned before, our patients may have an abdominal bruit. 02:04 It's not always present and nonspecific but sometimes we can hear that. 02:09 In our patients who have fibromuscular dysplasia, remember we said multiple arterial beds are affected so it's not uncommon to hear it in epigastric bruit along with a carotid bruit just as our patient case had. 02:22 Laboratory investigations will show an elevated plasma renin activity. 02:27 That makes sense cuz we just talked about how renin is activated at that JGA and plasma aldosterone concentration will be elevated as well. 02:34 So, once we're suspect for somebody having renovascular disease, we really want to pursue imaging and the modality of choice is magnetic resonance angiography or MRA. 02:47 It's highly sensitive and specific, and it's noninvasive, really making this the test screening tool of choice in most centers. 02:55 If you look at the image on the right, this is an MRA of a patient who has left proximal renal artery stenosis. 03:03 And you can see how the contrast agent gadolinium, actually has delayed filling of that left kidney. 03:10 You can also notice that that left kidney is actually quite a bit smaller compared to the right. 03:14 Now, one thing to keep in mind about using MRAs, it's going to be contraindicated in patients with a GFR of less than 30 mL/min. 03:24 The reason being is that the contrast agent gadolinium has been, in the past, associated with nephrogenic systemic fibrosis. 03:32 So, NSF or nephrogenic systemic fibrosis is characterized by thickening and hardening of the skin overlining the extremities and trunk, and it really results in fibrosis and expansion of the dermis. 03:42 It's an extremely debilitating disease and something that used to almost exclusively affect our end-stage renal disease population or patients who are on dialysis. 03:53 Now, we actually have newer gadolinium agents and we haven't seen this happen most recently but most radiologist will not use this agent in patients who have a GFR of less than 30 mL/min. 04:05 So, another option for imaging modalities include a CT spiral angiography with contrast or a CTA. 04:14 This has a very high sensitivity and specificity but of course, we've got the risk of contrast-induced nephrotoxicity in patients who have an impaired GFR or who have chronic kidney disease. 04:27 Again, if I have a patient with renovascular disease due to atherosclerosis, they might already have some chronic kidney disease in association with that. 04:35 So, this may not be an appropriate modality for that particular patient. 04:40 If you look at the image on the top right, this is a CTA or CT angiography which shows an actual right renal artery stenosis right at the promixal takeoff. 04:50 And finally, there's duplex doppler ultrasonography or ultrasound and this has a moderate sensitivity and specificity. 04:59 It's time consuming and highly operator dependent but if you have a very good ultrasound technologist, then it's something that you could really rely on because the advantage is, there's no exposure to contrast agents. 05:11 So, this image at the bottom right shows a renal duplex ultrasound and this shows an increase in renal arterial resistive index, an increase in peak systolic velocity and turbulent flow in the poststenotic area which is something that our ultrasonographer will be looking for in renal artery stenosis. 05:28 Now, the gold standard for diagnostic imagining is really the conventional renal arteriography. 05:35 This is used specifically when we're really planning intervention. 05:40 So, that means my vascular surgeon might be coming in to potentially revise a renal artery and its anastomosis. 05:49 It might be that I'm going to be doing a percutaneous transluminal angioplasty, meaning that I'm gonna balloon the area of stenosis, or deploying a stent in that stenotic lesion. 05:59 Now, it's certainly risky. So, a couple of different things that I want you to think about. 06:05 Number one, these patients are getting contrast exposure. 06:09 Not only are they getting contrast exposure, it's going directly into the arterial circulation and into those renal arteries. 06:16 So, I do want you to think about that in terms of causing contrast-induced nephrotoxicity. 06:21 The other thing, remember we talked about cholesterol emboli, where now, doing angioplasty and deploying stents in an area where there may be atherosclerotic plaque, so it's very likely that those patients can develop renal atheroembolic disease. 06:37 And finally, any time you're doing any kind of invasive intervention like this, there could be damage to either the renal or femoral arteries. 06:45 So, the image on the right actually shows a renal arteriogram and this is somebody who's actually doing an intervention. 06:52 So, you can see there's a catheter in the area labeled B, so the top right image. 06:58 A catheter is actually deployed to that renal artery and they are performing percutaneous transluminal angioplasty and stent placement to one of the renal arterial beds. 07:11 The last image on the lower right actually shows the post-stent deployment image where you have filling of that renal artery. 07:20 So, when we think about the treatment of renovascular disease, all patients really should be on appropriate antihypertensives and lipid-lowering therapy. 07:33 Patients with fibromuscular dysplasia should initially trial ACE inhibitor or an angiotensin receptor blocker therapy, ARBs. 07:40 If they remain hypertensive despite that, then we think about revascularization with percutaneous transluminal angioplasty. 07:47 Again, that's kind of blowing up that stenotic area and that's something that your interventional radiologist, vascular surgeon, or interventional nephrologist can do. 07:56 Now, patients with atherosclerotic disease should be on an ACE inhibitor or ARB as well and I want you to think about why they should be on that medication. 08:06 Remember, the whole mechanism that causes the renal artery stenosis or renovascular disease is hyperreninemia. 08:13 Increased aldosterone, so it's important to have something like an ang-II receptor blocker or an ACE inhibitor to antagonize that. 08:21 It is essential for these patients to be in lipid-lowering medications. 08:25 Remember, they have a significant atherosclerotic plaque burden. 08:29 That's what's causing their disease so we've got to be able to treat their hyperlipidemia and they should be on antiplatelet therapy as well. 08:36 Now, in the past, we used to do much more interventions including PTA and stent deployment in our patients who had renovascular disease due to atherosclerosis. 08:47 But in the last several years, we've had a couple of different meta-analysis and randomized control trial that showed that there's really no benefit to intervention, that includes PTA and stent placement, to medical therapy. 09:01 So, we really only reserve revascularization with stent placement for those patients who have uncontrolled hypertension on multiagent therapy, a rapid rise in serum creatinine with parenchymal loss, or flash pulmonary edema. 09:16 And let me just make the point to distinguish between renal vascular disease due to atherosclerotic disease versus FMD, fibromuscular dysplasia. 09:25 In fibromuscular dysplasia, we do treat with ACE inhibitors and ARBs but if we can't treat to goal and our patient remains hypertensive, the treatment of choice in that population is to actually have percutaneous transluminal angioplasty.
About the Lecture
The lecture Renovascular Disease: Clinical Features and Treatment – Secondary Hypertension by Amy Sussman, MD is from the course Secondary Hypertension.
Included Quiz Questions
Which of the following is true regarding atherosclerotic renovascular disease?
- It is associated with intermittent pulmonary edema in patients with normal cardiac function.
- The onset of hypertension is typically before the age of 55 years.
- Renovascular hypertension is usually well controlled with lifestyle changes alone.
- A 50% decrease in serum creatinine level is expected after starting the patient on an ACE inhibitor.
- Conventional renal arteriography is the screening test of choice for renal artery stenosis.
What is the appropriate imaging modality to screen for renovascular disease in patients with a GFR of <30 mL/min?
- Duplex Doppler ultrasonography
- Magnetic resonance angiogram
- CT angiogram
- Conventional renal arteriography
- Abdominal X-ray
Which of the following is true regarding the management of atherosclerotic renovascular disease?
- Patients should be treated with antiplatelet therapy.
- Percutaneous transluminal angioplasty has a significant benefit over medical therapy.
- ACE inhibitors/ARBs should be discontinued if there is an acute rise in serum creatinine level.
- Lipid-lowering agents have no role in management.
Which of the following has a risk of causing atheroembolic renal disease?
- Conventional renal arteriography
- Magnetic resonance angiogram
- CT angiogram
- Duplex Doppler ultrasonography
- Abdominal X-ray
Which of the following pairings is correct?
- Malignant hypertension - End-organ damage
- CT angiogram - Invasive, time-consuming, and operator dependent
- Duplex Doppler ultrasonography - Nephrogenic systemic fibrosis
- Calcium-channel blocker - Antihypertensive of choice for renovascular disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |