Playlist
Show Playlist
Hide Playlist
Cell-mediated Immunity: Regulatory T-Cells, Cytotoxic T-Cells, Macrophages, and Intraepithelial Lymphocytes
-
Slides Cell-Mediated Immunity.pdf
-
Reference List Immune System.pdf
-
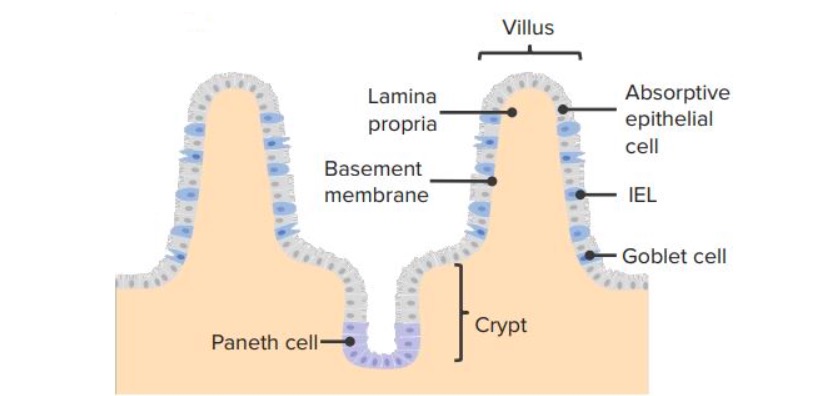
Download Lecture Overview
00:01 So those are different types of helper T-cells. 00:03 What about the regulatory T-cells? Well these suppress immune responses. 00:07 In fact, they’d probably be better called suppressor T-cells rather than regulatory T-cells. 00:13 And they act in a number of different ways. 00:16 One of the ways in which they function is by releasing immunosuppressive cytokines such as interleukin-10 and transforming growth factor beta (β). 00:25 And these cytokines can down-regulate the activity of eosinophils, basophils, mast cells, helper T-cells and cytotoxic T-cells. 00:39 So really, suppressing a very broad range of immune responses. 00:44 There is a second way in which regulatory T-cells can suppress immune responses, and that’s a cell contact-dependant mechanism whereby molecules on the surface of the regulatory T-cell interact with molecules on the surface of the cell that is going to be suppressed. 01:00 And cell surface CTLA-4 and LAG-3, are functional in down-regulating the activity of dendritic cells. 01:11 What about cytotoxic T-cells? Well, as their name suggests, they can kill; cytotoxic cell killing. 01:19 They can kill infected cells and also tumor cells. 01:24 They can also secrete cytokines; in fact virtually all cells in the body can secrete cytokines. 01:29 And cytotoxic T-cells have been divided into different subpopulations, just like the helper T-cells have. 01:36 So, we can identify Tc1 cells that secrete gamma interferon, just like Th1 cells secrete gamma interferon, Tc2 cells that secrete IL-4 and so forth just like Th2 cells do. 01:48 So there are also subpopulations of cyctoxic T-cells. 01:55 The killing of an infected cell by cytotoxic T-cell depends upon peptides from the pathogen being presented by MHC Class I to the T-cell receptor on the surface of the cytotoxic T-cell. 02:12 This will lead to the activation of the cytotoxic T-cell. 02:17 And there are two ways in which the killing process can function. 02:23 First of all, infected cells have on their cell surface, the molecule Fas, and this can interact with the molecule Fas ligand or FasL on the surface of the cytotoxic T-cell. 02:37 So when Fas is engaged by Fas ligand, a signal is sent into the infected cell which activates caspases. 02:48 And these are enzymes that are involved in inducing apoptotic cell death in the infected cell. 02:56 There is a second pathway by which cytotoxic T-cells can kill infected cells. 03:01 And this relies on the release of enzymes called granzymes from the cytotoxic T-cell, and also molecules called perforin which as their name suggests, cause pores to be formed in the membrane of the infected cell. 03:21 Again, just like Fas-Fas ligand interaction, the granzyme-perforin pathway leads to caspase activation and apoptotic cell death of the infected cell. 03:34 This killing of infected cells may seem like a rather brutal strategy. 03:39 I mean the cytotoxic T-cell is killing our own cells. 03:44 But the problem is, as we’ve already heard, that antibody and complement can’t get at pathogens once they’re inside a cell. 03:50 So, this strategy of killing our own cells removes the ability of viruses and other pathogens to replicate within our cells. 04:00 And as long as that happens very early on in the immune response, it’s not a problem. 04:03 We can regenerate a few of our own cells, and the infected cells can be got rid of. 04:09 And the way in which the killed cells are removed is by using macrophages to recognize the fact that these cells have been killed and to take them up and then destroy them. 04:21 So here we can see a cytotoxic T-cell that has interacted with a virus infected cell. 04:26 And when those apoptotic signals are sent into the cell, either via the Fas-Fas ligand pathway or the perforin-granzyme pathway; one of the things that happens is that there is a flipping of the membrane on the outside of the apoptotic cell. 04:43 So bits of the membrane that… surface membrane of the cell that were on the inside of the cell now become on the outside of the cell. 04:50 And molecules associated with the inside layer of the cell membrane, now become exposed to the outside. 04:56 Previously they weren’t on the outside but now they are. 04:59 An example of such a molecule is phosphatidylserine. 05:03 And this is normally not present on the outside of the cell but following apoptotic cell death, the phosphatidylserine appears on the outside of the cell. 05:14 And macrophages have on their cell surface, receptors for phosphatidylserine. 05:22 And that means that they can recognise the fact that this is a dead or dying cell, and they will engulf it and destroy it. 05:31 I’m sure you’re fairly clear that infections often enter the body via mucosal surfaces. 05:36 So you won’t be surprised to hear that there are many immune system cells associated with mucosal surfaces. 05:43 And one group of lymphocytes that has been identified as being important in protection of mucosal surfaces, are the intra-epithelial lymphocytes. 05:53 And on this diagram you can see them highlighted by the red boxes. 05:58 So they are resident within the intestinal epithelium, and they are one of the first lines of defence of the immune system. These intra-epithelial lymphocytes are a mixed population of antigen-experienced cells. So they’re not naïve cells, they’ve already encountered antigen previously. And they comprise both, gamma-delta T-cells and alpha-beta T-cells. 06:24 Some of them are CD4+, but others are CD8+. 06:29 And very unusually, many of the CD8+ cells, have a… not the normal form if you like, of the CD8, which is an alpha-beta heterodimer. 06:41 But they have a alpha-alpha homodimer version of CD8.
About the Lecture
The lecture Cell-mediated Immunity: Regulatory T-Cells, Cytotoxic T-Cells, Macrophages, and Intraepithelial Lymphocytes by Peter Delves, PhD is from the course Humoral Immunity and Cell-mediated Immunity. It contains the following chapters:
- Regulatory T-Cells
- Cytotoxic T-Cells
- Removal of Killed Cells by Macrophages
- Intraepithelial Lymphocytes
Included Quiz Questions
Which of the following surface molecules are characterisitc of intraepithelial lymphocytes?
- Cluster of differentiation 8 alpha alpha
- Cluster of differentiation 28
- Human leukocyte antigens (HLA) A
- Major histocompatibility complex (MHC) class II
- Fas
When regulatory T cells secrete interleukin 10, and TGFβ, they suppress the actions of all EXCEPT which of the following?
- Keratinocytes
- Mast cells
- Eosinophils
- Basophils
- Helper T cells
Which of the following is the main function of Fas-Fas ligand binding?
- Apoptosis
- Cell differentiation
- Cell proliferation
- Cytokine release
- Immune suppression
Externalization of which of the following molecules in an apoptotic cell is required for effective phagocytosis by macrophages?
- Phosphatidylserine
- Major histocompatibility complex (MHC) class II
- Cluster of differentiation 8 alpha alpha
- Pathogen associated molecular patterns
- Pattern recognition receptor
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |