Playlist
Show Playlist
Hide Playlist
Recurrent Laryngeal Nerves and Anomalies of Arterial Development
-
Slides 06-32 Aortic Arches and Large Arteries.pdf
-
Reference List Embryology.pdf
-
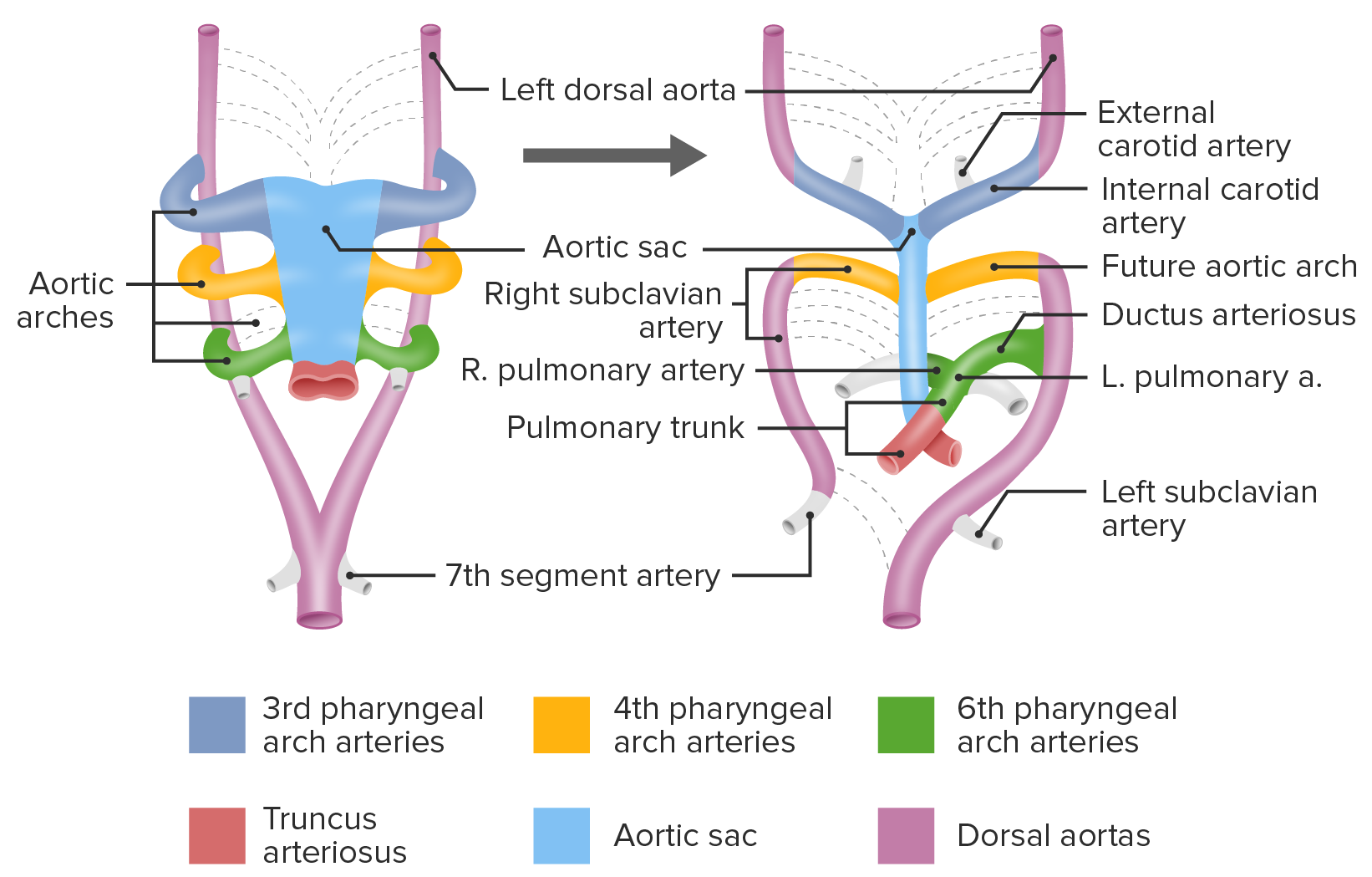
Download Lecture Overview
00:01 Now, why should we care? What does the practical significance of this have to do with anything? Essentially, you wanna remember that these blood vessels are not developing in isolation, we have nerves and bones and viscera, different organs all developing at the same time. 00:18 And one thing that this explains is why the recurrent laryngeal nerve takes such a bizarre course on both sides of the body? Initially, the recurrent laryngeal nerve, which innervates structures from the 6th pharyngeal arch is gonna be going from the vagus nerve into the developing muscles of the larynx and its looping underneath the 6th aortic arch in order to reach the 6th pharyngeal arch. 00:44 As the body elongates, that nerve gets stretched out and we're left with the vagus nerve coming down into the thorax giving off other branches, but having its recurrent branch looped back up to our larynx and have a very extended U as it does so; but on the right, we find it looping around our subclavian artery and on the left, looping around the aortic arch. 01:07 The reason for that is on the right side the 6th aortic arch losses its connection to the dorsal aorta and as the body grows, that nerve gets pulled further up and the next thing it hits is the 4th aortic arch and that remains as part of the subclavian artery, which is why we have a different course on the right than on the left for the recurrent laryngeal nerve, because on the left it winds up going around the arch of the aorta and gets tethered there, and in particular it's gonna be found just beside the ductus arteriosus which after birth becomes fibrous and is known as the ligamentum arteriosum. 01:44 So that's why we have two different courses for the same nerve on the right side versus the left side, it's reflecting the lack of symmetry between the right and left vascular development. 01:56 Now other things that can go wrong are gonna be called vascular slings where the vasculature actually constricts another organ. 02:04 In this case, we can have the esophagus and the trachea get compressed by the vessels. 02:10 The most common form of this is gonna be either a double aortic arch or a subclavian artery that wraps around the back of the esophagus to get to the right upper limb. 02:20 What happens in this case is we have the heart pumping blood to the aortic arches and we have the two dorsal aorta, in this picture, making a nicely memetic heart-shaped loop as they go to the dorsal aorta. 02:33 Normally, on the right side, the segment of the dorsal aorta between the 7th intersegmental artery and the fused dorsal aorta, would rescind in the subclavian artery on the right would detach, move up, and be connected to the upper limb only if that portion of the aorta fails to rescind, we wind up with a tether and that tether, as the body elongates, is gonna move up and constrict the esophagus and the trachea. 03:01 I'm gonna back-up just a moment, and you can see that if the esophagus and the trachea are passing posterior to the heart but anterior to the dorsal aorta, as that dorsal aorta shortens it's gonna wind up effectively zipping up and then constricting those organs causing difficulty swallowing and possibly difficulty breathing as those two organs get constricted. 03:26 Another form of this is called a subclavian sling and it's due to the right dorsal aorta rescinding but doing it in the wrong place. 03:37 Instead of rescinding between the 7th inter-segmental artery and the fused dorsal aorta, it will occasionally rescind above that point and we'll have that right dorsal aorta disappear but superior to the 7th inter-segmental artery. 03:51 Now, what I want you to remember is that the 7th inter-segmental artery is tethered to the upper limb. It can't just move around it, can't just detach and find another more efficient route to where it wants to go. 04:04 It's stuck right where it is. 04:05 So as the body elongates and that vasculature gets more and more tight we wind up with it passing posterior to the esophagus and the trachea. 04:15 So in this case we have our right subclavian artery coming off most distally from the arch of the aorta because it has no other choice, it came from much further down and had to take that posterior course simply to get where it was going. 04:30 Again, this can cause difficulty swallowing and even constriction of the airway if it's very pronounced. 04:37 Last and certainly not least are gonna be coarctations of the aorta. 04:41 As development happens, normally, the aorta should stretch, lengthen, and stay open along its entire length. 04:49 But occasionally there can be constrictions and these are called coarctations. 04:54 The most common one is called the post-ductal coarctation and that simply denotes that the ductus arteriosus leaves the pulmonary trunk for the aortic arch and the coarctation happens after that. 05:06 Now our coarctation is gonna narrow this massive artery meaning there's gonna be a lot of blood pressure above that constriction but much less blood pressure below, and our lower limbs, organs are gonna be deprived of blood if there's no way for the blood to reroute pass that blockage. 05:23 So in these cases, the ductus arteriosus is going to close because there's a lot of pressure in the aorta, there's a lot of oxygen that signals it to close and we wind up with the ductus arteriosus closing, yet we have impeded blood flow. 05:39 What happens in this case is that arteries that bypass the aorta will enlarge tremendously to get blood to the organs and lower limbs so blood will back up into the subclavian arteries go through the internal thoracic arteries on either side of our sternum and then back-fill the intercostal arteries into the thoracic aorta and those intercostal arteries will enlarge to the point that it actually leave pretty pronounced groves on the underside of the ribs and then the blood will fill into the aorta, move down to the organs in the lower limb. 06:14 One way to diagnose this at least early is to look for differences in the pulse in the upper limb and the lower limb. 06:21 A very strong bounding pulse in the two upper limbs but absent or very, very less pronounced pulses in the lower limb can be an early sign of coarctation of the aorta. 06:32 Now, sometimes these are subtle and aren't diagnosed until adulthood so I want you to note that it's not always gonna be obvious, these are not constrictions that are always so severe that they result in immediate distress but can be brought on by exercise and they're sometimes associated with the bicuspid aortic valve rather than the normal tricuspid set of semilunar valves leaving the aorta. 06:55 Now much less common, maybe between 2% to 5% of coarctations occur proximal to the ductus arteriosus and these, not surprisingly, are called pre- ductal coarctations of the aorta. 07:08 In this case, we've got a constriction of the aorta but distal to that we have the ductus arteriosus. 07:15 Because the pressure in that distal portion of the aorta is so low, the ductus arteriosus stays open and it's gonna take poorly oxygenated blood from the pulmonary circuit that's trying to get to the lungs and spill into the descending thoracic aorta. 07:33 Because of this there may be cyanosis or blue tinting of structures in the lower limb but not in the upper limb, that's going to be getting fresh blood from the aortic arch. 07:44 Patients with the pre-ductal coarctation of the aorta are gonna show cyanosis in any vessel that is distal to the coarctation and that's important because the coarctation doesn't always leave all the subclavian and carotid arteries unaffected. 08:00 If I have coarctation that occurs between my left common carotid and left subclavian artery, I'm gonna have good reddish perfusion of my head and neck, but I'll have cyanosis from my left arm but not my right. 08:14 If that coarctation happens between the right brachiocephalic trunk and the left common carotid artery, I may have one-sided cyanosis of the head and neck, cyanosis of the left upper limb but unaffected right upper limb and relatively decent reddish-pinking appearance of the mucus membranes on my right side. 08:34 So remember that the position of the coarctation can determine which vessels are getting cyanotic blood and which once are not, so it's typically evident right after birth if these are present, that cyanosis will be noted right away as opposed to a post-ductal coarctation which may only become notable as the patient gets older and becomes more active. 08:55 The previously mentioned congenital defects are usually related to impaired remodeling of the aortic arches. 09:03 The processes of remodeling of the aortic arches is responsible for the development of the mature arteries such as the carotid arteries and the differentiation between the left and right arterial circulation. 09:17 Again, this is usually related to a differential expression of the HOX gene family, particularly HOX3. 09:25 Mutations in this gene are implicated in the pathophysiology of impaired development of the carotid arteries from the 3rd aortic arch and the presence of a double-arched aorta. 09:38 Alright, thank you very much for your attention and I'll see you in our next talk.
About the Lecture
The lecture Recurrent Laryngeal Nerves and Anomalies of Arterial Development by Peter Ward, PhD is from the course Development of Thoracic Region and Vasculature.
Included Quiz Questions
What structure does the right recurrent laryngeal nerve loop under before ascending to innervate the larynx?
- Right subclavian artery
- Ligamentum arteriosum
- Esophagus
- Common carotid artery
- Brachiocephalic artery
Which structure does the left recurrent laryngeal nerve loop under?
- Aortic arch
- Ligamentum arteriosum
- Common carotic artery
- Subclavian artery
- Brachiocephalic artery
A subclavian sling occurs when the right subclavian artery originates from what mature structure?
- Distal aortic arch
- Proximal aortic arch
- Left subclavian artery
- Descending aorta
- Common carotid artery
Post-ductal coarctation of the aorta is the most common type of coarctation that occurs in what part of the aorta?
- After the ligamentum arteriosum
- After the subclavian artery
- After the brachiocephalic artery
- After the common carotid artery
- After the aortic valve
In coarctation of the aorta, what would be the expected quality of the pulses and blood pressure?
- Notably decreased in vessels distal to the coarctation
- Notably decreased in vessels proximal to the coarctation
- Notably increased in vessels distal to the coarctation
- Unaffected by the coarctation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |