Playlist
Show Playlist
Hide Playlist
Reactive vs. Psoriatic Arthritis (PsA)
-
Rheumatology I 02 Seronegative Spondylarthropathies.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
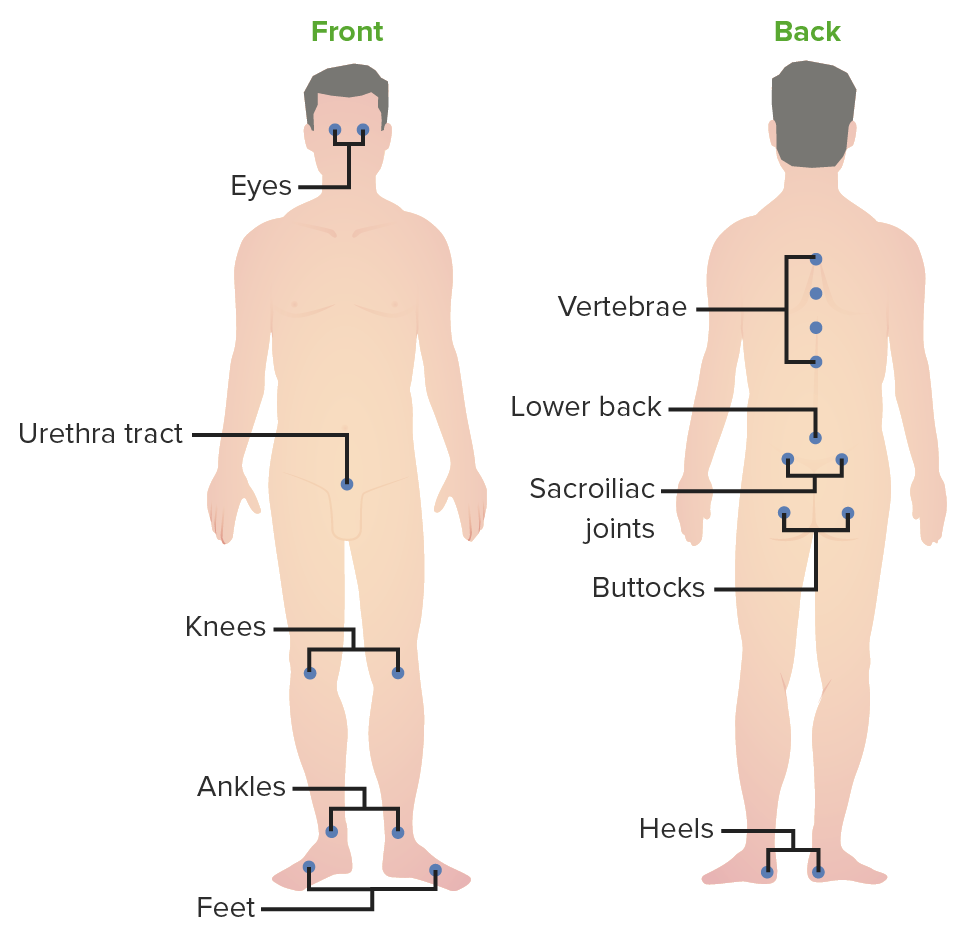
00:01 So seronegative. It’s the HLA-B27. 00:04 These are all the common features in all of them. 00:06 Next, predominantly, where is my issue in the back? Lower extremities. Inflammatory. Asymmetric arthritis. 00:15 One to three weeks after infection. 00:18 What infection? Now be careful here. 00:19 Let me remind you to go back and review septic arthritis. 00:23 We talked about septic arthritis, first we talked about adenitis In other words, there’s a patient who have diabetes, there’s a patient who had sickle-cell disease. 00:32 Once you get past those facts, and dealt with their history, and that is not been presented. 00:38 I told you to next take septic arthritis and divide it into gonococcal and non-gonococcal. 00:44 And under that category, I told you to please focus on non-gonococcal, because under non-gonococcal, a particular bacterial called Staph aureus, is so highly aggressive, that if you’re not aggressive with managing your patient, that patient’s knee is permanently gone. 01:01 Once you’re completely familiar with that discussion of septic arthritis, then you come back here and keep separate reactive arthritis, in which it’s HLA-B27 seronegative, is that understood? This has nothing, I repeat, and nothing to do with gonococcal. 01:17 Now what are my organisms? Oh, take a look, some of these includes salmonella, shigella, campylobacter, chlamydia. 01:25 So, it used to be called Reiter’s. 01:28 And here’s my triad. 01:29 And we have urethritis, or let’s go in order. 01:33 I like to use can’t see, can’t pee, can’t climb a tree. 01:36 The can’t see part obviously is going to refer to your conjunctivitis and uveitis. 01:43 If you cannot pee, and you’re thinking about the non-gonococcal urethritis. 01:46 And if you finally can't climb a tree, because my goodness! You have arthritis! There you have it, reactive. 01:53 Pathogenesis. Usually triggered by urethritis, cervicitis. 01:57 Some of the infection include the following: If it’s Chlamydia trachomatis, Remember, this is the urethritis part. 02:06 It has nothing to do with gonococcal, nothing. 02:09 The Chlamydia trachomatis, less likely pneumonia, shigella is one that you wanna keep in mind. 02:16 Particularly, the flexneri. 02:18 Then you have the salmonella, particularly typhimurium. 02:22 Yersinia enterocolitica, campylobacter jejuni, and ureaplasma. 02:28 You need to make sure that you know some of these organisms that are responsible for causing non-gonococcal urethritis in reactive arthritis. 02:38 The disease is more severe in patient with AIDS. 02:42 Not exactly sure as to why and B27 in most of your patients, In the reactive arthritis, let’s take a look at some extra-articular manifestation. 02:48 MSK stands for musculoskeletal lupus erythematosus polyarthritis. 02:54 Remember the insertion site of a tendon into the bone, may undergo inflammation. 02:58 We call that enthesopathy, dactylitis, sacroiliiatis. 03:02 Remember the urethritis will be non-gonococcal. 03:06 Organisms here could include, are shigella, could be salmonella, could be chlamydia, could be your campylobacter jejuni. 03:13 Ocular could have conjunctivitis. 03:15 Please picture the conjunctiva and uvea, specifically the anterior uveitis. 03:22 On the sole of the foot here, we’re seeing a particular derm issue with reactive arthritis that we then refer to as being blennorhagica. 03:33 And then, what I will show you is something called circinate balanitis around the penis. 03:39 In the cardiovascular system, they might have pericarditis, pericardial rubs, AV blocks. 03:47 Reactive arthritis, you could find aortitis. 03:50 Men are affected more so than woman were reactive arthritis. 03:54 Due to cervicitis typically less symptomatic and then urethritis. 04:00 Chronic symptoms after viral syndrome resolution is common with viral. 04:07 The signs that you are looking for as a clinician, the hands are inflamed, dactylitis. 04:14 Take a look at the conjunctiva here, the injected conjunctivitis. 04:19 On close examination, if by chance in the window of the cornea you’ll find a little bit of fluid accumulation, well, the uvea has been affected, uveitis. 04:31 The picture in the far right is your finger, and the finger here, circinate balanitis. 04:37 All part of the syndrome of reactive arthritis. 04:39 Diagnosis. 04:41 Look for temporal correlation between the infection and the onset of symptoms. 04:47 The differentials may include gonococcal. 04:50 With gonococcal we talked about how you get a purulent type of arthritis, or purulent type of synovial fluid with lots of WBCs. 05:00 In addition, we talked about the triad including tenosynovitis. 05:04 Also talked about pustular or derm issues, there may be polyarthralgia. 05:09 In lyme disease, you’re looking for patient coming in from maybe New England, particular Connecticut, and they went hunting, right? And the tick then introduced, unfortunately, a dangerous bacteria, what we call borrelia burgdorferi. 05:26 Rheumatoid arthritis, well with that, we may find rheumatoid factor to be positive, and rheumatoid arthritis will be more symmetrical and the patient has morning stiffness that may last greater than an hour. 05:39 Gout, and then pseudogout, technically called calcium pyrophosphate disease. 05:45 These are all differentials that you wanna keep in mind when dealing with the joints. 05:49 However, remember, keep to your roots in your foundation, Management. Include NSAIDs first. 05:54 And then followed by your drugs or disease modifying anti-rheumatologic agents or drugs called DMARDs. 06:02 Another type of seronegative spondyloarthropathy brings us to psoriatic arthritis. 06:10 Let me tell you, right off the bat, the psoriatic arthritis, that the patient, only 15% at a time that those patient’s that have the traditional salmon plaques of psoriasis. 06:23 May then have involvement of the joints or vertebrae. 06:26 Only about 15% maybe 30% at the max. 06:29 It’s a small percentage but still very important for you to know. 06:32 Seronegative spondyloarthropathy, HLA-B27. 06:36 Here the presentation oftentimes is going to be the skin rash. 06:41 And then issues with our bones. 06:45 I will show you pictures on x-ray of the hand for example. 06:49 Appears like rheumatoid arthritis, but what does that mean? That means that rheumatoid arthritis might have ulnar deviation. 06:57 You will also perhaps have issues with the metacarpophalangeal or maybe the PIP. 07:04 But joint involvement is quite different here. 07:06 As you shall see the patterns are important. 07:08 You’ve heard of maybe your pencil type of deformity. 07:12 I’ll show that coming up. 07:13 It can be symmetrical or asymmetrical but that doesn’t tell you too much. 07:18 Pathogenesis. 07:19 Psoriasis, really unknown as far as arthritis. 07:24 B27 positive seen with sacroiliitis. 07:27 Now, as I told you, these conditions of seronegative tend to be in the lower back so here is sacroiliitis. 07:35 If you take a look at the hand on close examination. 07:39 Proximally, you will find the salmon plaque color or salmon-colored plaque, referring to the psoriasis. 07:47 Parakeratosis will be expected to be seen on histology. 07:52 But most will develop skin lesion way before their arthritis. 07:56 And maybe, perhaps about 15-30% of your patients may then involvement of the bones. 08:03 Now, we're gonna take this hand here and then we're gonna do an x-ray. 08:07 Now when you do the xray you’ll see a few things The DIP joints are involved, which is a trait that is often seen in osteoarthritis. 08:14 And You may see the “pencil in cup” deformity, shown here with the white arrow. 08:18 This DIP involvement can be associated with onycholysis and nail pitting. 08:22 Another finding is that the arthritis is more asymmetric in the joints it effects. 08:26 Usually in severe OA, the dip joints are affected in a somewhat equal pattern, while in psoriatic patients, you may see a single DIP joint be involved, or a patient develops dactylitis as we saw in a previous slide. 08:39 Continue our discussion of five patterns of arthritis. 08:43 The third here, might be symmetrical polyarthritis. 08:46 Very similar to rheumatoid arthritis, keep that in mind but obviously here, rheumatoid arthritis might be Rf positive. 08:52 Here, we have Rf negative, seronegative. 08:54 Fourth, arthritis mutilans. 08:57 In other words, what may happen so badly, severe enough, is that with the erosion and destruction taking place. 09:03 Imagine looking at the stars at night with a telescope. 09:08 Now, with the telescope, you can either pull it out or you can push it back in. 09:14 Correct? And what may happen with such severe destruction of the finger is that, one part of the finger distally may then erode into the proximal literally telescoping of the digits. 09:25 That is not good. 09:27 And then, sacroiliitis. 09:31 Here are five patterns of arthritis that you might find with psoriatic arthritis. 09:35 Look for the skin lesion, please. 09:37 The salmon-colored plaques that I showed you earlier. 09:39 Management of psoriatic arthritis. 09:42 Remember we're trying to take care of the bone issues, of the joint issues. 09:47 NSAIDs and like many others, when we talked about DMARDs, that these modifying agents or anti-rheumatologic drugs, here once again will be pertinent. 09:59 And number two, anti-TNF therapy, the biologics that you wanna keep in mind. 10:02 Now, I’m just gonna mention our fourth and final type of seronegative spondyloarthropathy. 10:11 The details of our enteropathic arthropathy are inflammatory bowel diseases that we have discussed in great detail in gastroenterology obviously. 10:25 However, there’s a possibility of a patient, has ulcerative colitis or Crohn’s disease, in which the vertebrae could be affected or the bones could be affected, maybe lowered back pain. 10:38 When that happens, we then refer to it as being enteropathic type of arthropathy. 10:43 Now with this then, this then completes our four major types of seronegative spondyloarthropathies. 10:51 We went through the common features that you'd expect to find in all four. 10:55 Now, we have integrate detail in those in which you were able to differentiate ankylosing spondylitis, from reactive arthritis, from psoriatic arthritis, and then obviously here we have GI issues with our enteropathic including our two major inflammatory bowel diseases.
About the Lecture
The lecture Reactive vs. Psoriatic Arthritis (PsA) by Carlo Raj, MD is from the course Seronegative Spondylarthropathies. It contains the following chapters:
- Introduction to Reactive Arthritis
- Signs and Symptoms of Reactive Arthritis
- Psoriatic Arthritis
- Symptoms of Psoriatic Arthritis
Included Quiz Questions
Which of the following organisms is not typically associated with reactive arthritis?
- Neisseria gonorrhea
- Chlamydia trachomatis
- Shigella
- Campylobacter
- Yersinia
You find asymmetric oligoarthritis and conjunctivitis in a young man who had a urinary tract infection 2 weeks earlier. Serology and X-rays are unremarkable. Which of the following diagnoses is most likely?
- Reactive arthritis
- Rheumatoid arthritis
- Psoriatic arthritis
- Osteoarthritis
- Disseminated gonococcal infection
Which of the following statements regarding psoriatic arthritis is MOST accurate?
- Arthritis appears after the onset of skin lesions in the majority of patients.
- A bacterial etiology has been established.
- Negative HLA-B27 rules out the disease.
- Enthesitis suggests an alternative diagnosis.
- Peripheral polyarthritis is not seen.
Which of the following joint findings is NOT typically seen with psoriatic arthritis?
- Overhanging osteophytes
- Sacroilitis
- Symmetric polyarthritis
- Dactylitis
- Pencil-in-cup deformity
Pencil-in-cup deformity is primarily associated with a severe form of psoriatic arthritis (PsA) called arthritis mutilans. Which joints are typically involved in this condition?
- Distal interphalangeal joints
- Proximal interphalangeal joints
- First metatarsophalangeal joints
- Metacarpophalangeal joints
- First carpometacarpal joint
What GI condition is associated with enteropathic arthropathy?
- Crohn disease
- Irritable bowel disease
- Pancreatitis
- Gallstones
- Celiac sprue
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |