Playlist
Show Playlist
Hide Playlist
Pyelonephritis (Kidney Infection) and Perinephric Abscess: Diagnosis & Management
-
Slides PyelonephritisPerinephricAbscess InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
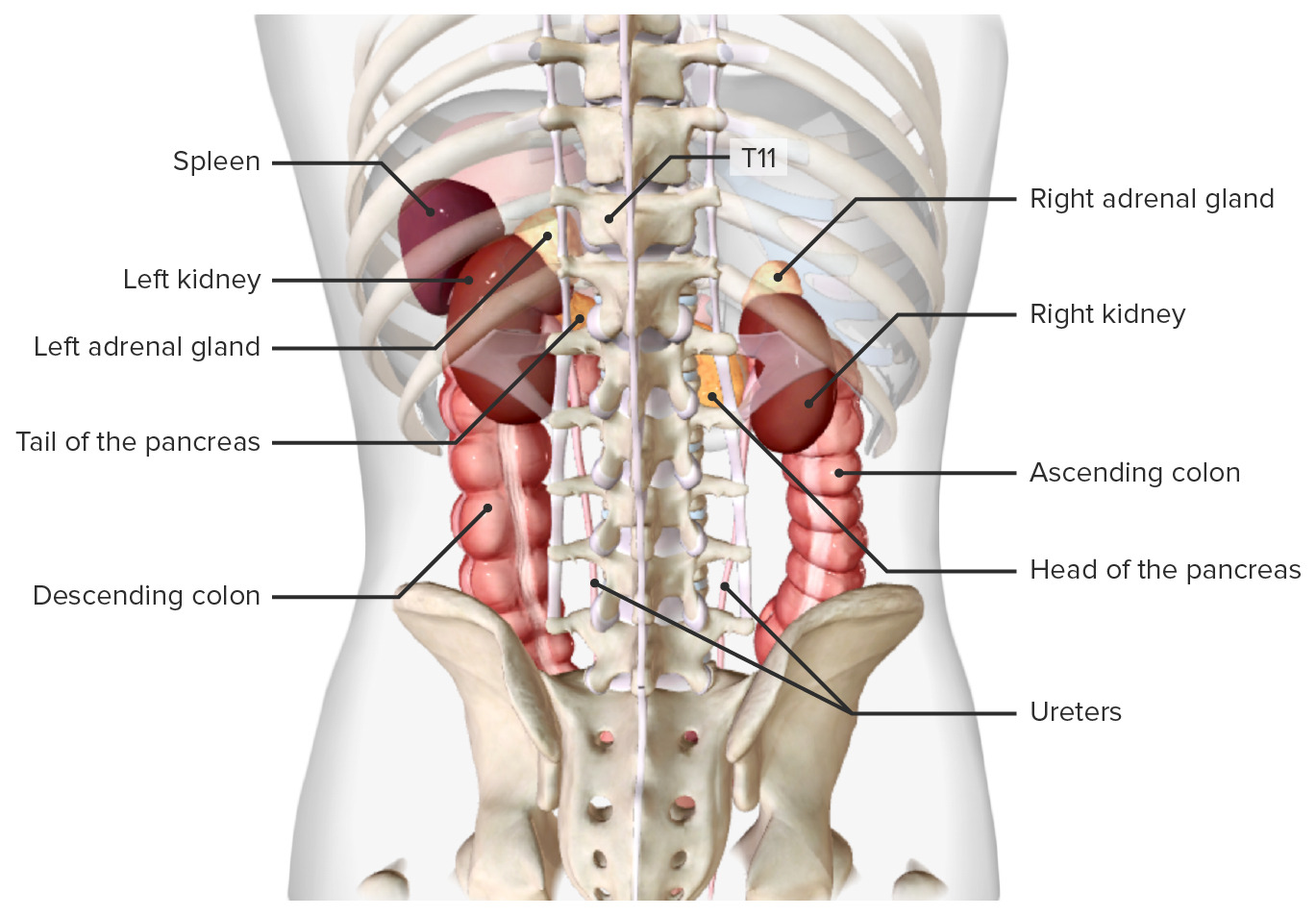
00:01 In the laboratory, we look for the presence of pyuria and 10 white cells per microliter of midstream urine in a ounting chamber is the gold standard. 00:15 However, a counting chamber's not available that often. 00:20 So we can use just centrifuge urine and look for 5 to 10 white cells per high power microscopic field. 00:30 We also have the dipstick, leukocyte esterase test Leukocyte esterase is present in the granules of neutrophils. 00:38 So if the leukocyte esterase is positive, then by inference, you can say there are white cells in the urine. 00:45 And the sensitivity and specificity are decent, 75 to 96% sensitive, 94 to 98% specific. 00:54 Once again, if a patient does not have microscopic hematuria, it's probably not coming from the urinary tract. 01:03 The source of the fever is somewhere else. 01:07 The urine culture in pyelonephritis certainly should have at least 10 to the fifth bacteria per ml. 01:14 And a poor man's culture is to look under the microscope looking for microorganisms. 01:21 You can do it by Gram stain. 01:23 If you see one organism per one oil immersion microscopic field, you can basically conclude that there are at least 10 to the fifth organisms per ml of that infected urine. 01:35 When do we need to image people? Well, for uncomplicated pyelonephritis, when the diagnosis is clear, and the patient's moderately ill, we don't need to image them. 01:47 We need to image them for complicated pyelonephritis when we suspect a structural urologic abnormality, when we're not sure what's going on, and urinary tract infection pyelonephritis is up high on the list. 02:03 If someone obviously is unusually severely ill with symptoms of a urinary tract infection and it would be prudent in an immunocompromised patient to get imaging because they may have not only urologic abnormalities, but they may have serious abscess in the kidney or other organs in the abdomen. 02:25 And then obviously patients who fail to improve from the choice of therapy we give them for pyelonephritis or for males who have suffered recurrent infections. 02:39 And what's the sequence of imaging? We start looking with a plain film and what we're looking for are calculi stones because that can be a reason for either the first time or recurrent pyelonephritis, and also we can detect some soft tissue masses. 02:57 Renal ultrasound is the next step. 03:00 And a renal ultrasound can tell you not only the presence of pyelonephritis, but perinephric abscess. 03:06 And if it's necessary, a CT scan can show you intrarenal or perinephric abscess and I think you can see the perinephric abscess on this particular projection For uncomplicated cases, empiric therapy of mild to moderate pyelonephritis can be done as an outpatient. 03:24 Patients will undergo a urine Gram stain, culture and antibiotic susceptibility testing. 03:30 There are some basic general guidelines for the initial antibiotic therapy. 03:33 The treatment choices can become complex in certain cases. 03:37 The patient's improvement must be followed very closely and there should be a low threshold to reevaluate or admit them should their condition worsen. 03:44 If there is no risk for multi drug resistant gram negative infections, for example, patients living in hospital or long term care facility, there are three possible treatment choices for non-pregnant women who are being treated as outpatients. 03:58 First, if the patient is not allergic to fluoroquinolones, they can be given a 5 to7 day course of Ciprofloxacin. 04:05 If there's more than a 10% community resistance of E. coli to fluoroquinolones, intramuscular IV Ceftriaxone is started and then followed by 5 to 7 days of Cipro. 04:16 And finally, if the patient has an allergy to fluoroquinolones, intramuscular IV ceftriaxone is given first and followed then with trimethoprim sulfamethoxazole for 5 to 7 days. 04:26 On the other hand, if it's determined that there are risk factors for a multidrug resistant gram negative infection, we have two different options. 04:34 First, if the patient has no allergies to fluoroquinolones, they should be started on intramuscular or IV ertapenem, followed by Cipro for 5 to 7 days. 04:43 If they are allergic to fluoroquinolones, on the other hand, they should be started on ertapenem daily until the cultures and susceptibility results allow for the transition to a more narrow coverage. 04:53 Empiric therapy for severe cases of pyelonephritis are generally taken care of as an inpatient to best allow for the treatment of sepsis or urinary tract obstruction should it occur. 05:03 The process still involves collecting urine Gram stain, culture and susceptibility testing. 05:08 But as we will see on the following slide, the treatment is a bit more complex. 05:11 Let's look at how we manage severe pyelonephritis involving sepsis or urinary tract obstruction. 05:17 Key first step: Get imaging. We need to identify any obstruction, abscess, or other complications that might need intervention beyond antibiotics. 05:28 Initial therapy needs broad coverage with two parts: Carbapenem (meropenem/imipenem) for serious gram-negatives including ESBL Plus vancomycin for resistant gram-positives. 05:42 Once they're improving, we can step down based on MDR risk: With MDR risk (recent healthcare exposure, resistant isolates, etc): Cefepime (if no ESBL concern) Piperacillin-tazobactam Or continue carbapenem if recent ESBL No MDR risk? We can go simpler: Ceftriaxone or Fluoroquinolone (cipro/levo) Remember, start broad, then narrow based on cultures. These are our sickest patients - we can't afford to miss with initial coverage. 06:14 Once the cultures and sensitivities are finalized, the antibiotic coverage can be narrowed. 06:19 All male urinary tract infections require more aggressive management than female UTIs. 06:25 Why? Two key reasons: The first is anatomical and clinical - we always have to worry about prostate involvement. The prostate can serve as a sanctuary site for infection, making treatment more challenging and requiring better tissue penetration of antibiotics. 06:43 The second reason is fascinating and was just discovered in 2024 - androgens actually impair neutrophil function and maturation in the infected kidney. 06:53 This biological mechanism helps explain why men often get more severe infections and are at higher risk for complications like renal abscesses. 07:03 So how do we treat? For standard cases, we use IV fluoroquinolones - either ciprofloxacin or levofloxacin - for 7-14 days. 07:15 Notice this is different from women where we can often use oral therapy for shorter durations. 07:20 However, if the patient has risk factors for multi-drug resistant organisms - like recent hospitalizations, healthcare exposure, or travel to areas with high resistance rates - we switch to broader coverage with either meropenem or ertapenem. 07:32 we switch to broader coverage with either meropenem or ertapenem. 07:37 Let's address the critical management considerations for severe pyelonephritis beyond antimicrobial therapy. 07:44 CT imaging is essential for three primary purposes: Determining the extent of infection Identifying complications requiring intervention Guiding surgical management when necessary Two scenarios require immediate intervention: First, perinephric abscess formation mandates drainage. 08:04 Antimicrobial therapy alone is insufficient in these cases. 08:08 Second, urinary tract obstruction requires prompt relief, whether through cystoscopy or alternative urologic measures. 08:16 The foundation of therapy remains appropriate antimicrobial selection. While broad-spectrum coverage is initially warranted, therapy must be carefully tailored based on culture and susceptibility results. 08:28 These interventions are not merely adjunctive - they are essential components of successful management in severe cases. 08:35 Proper imaging guides intervention, which in turn optimizes antimicrobial efficacy.
About the Lecture
The lecture Pyelonephritis (Kidney Infection) and Perinephric Abscess: Diagnosis & Management by John Fisher, MD is from the course Urinary Tract Infections. It contains the following chapters:
- Pyelonephritis and Perinephric Abscess – Diagnosis
- Uncomplicated Infection – Management
Included Quiz Questions
A positive leukocyte esterase test most strongly indicates which of the following?
- Presence of white blood cells in the urine
- Lower urinary tract infection
- Pyelonephritis
- Presence of urinary stones
- Glomerulonephritis
Which of the following is an indication for imaging in urinary tract infection?
- Failure to improve with antibiotic therapy
- Acute uncomplicated urinary tract infection
- Acute pyelonephritis
- Recurrent cystitis in a sexually active woman
- Pregnancy
According to the lecture, which of the following is the approximate sensitivity of the leukocyte esterase test for urinary tract infection?
- 75%
- 35%
- 50%
- 65%
- 20%
In a stable adult patient with suspected perirenal abscess, which of the following is the most appropriate initial imaging technique?
- Ultrasound
- Abdominal X-ray
- Computed tomography scan
- Magnetic resonance imaging
- Voiding cystourethrography
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
concise, really easy to listen to. Gave salient points very well. Loved the pause for thought on the red flag of having a staph aureus urinary tract infection.