Playlist
Show Playlist
Hide Playlist
Pneumonia and Pulmonary Infections: Examination
-
Emergency Medicine Bord Pneumonia and Pulmonary Infections.pdf
-
Download Lecture Overview
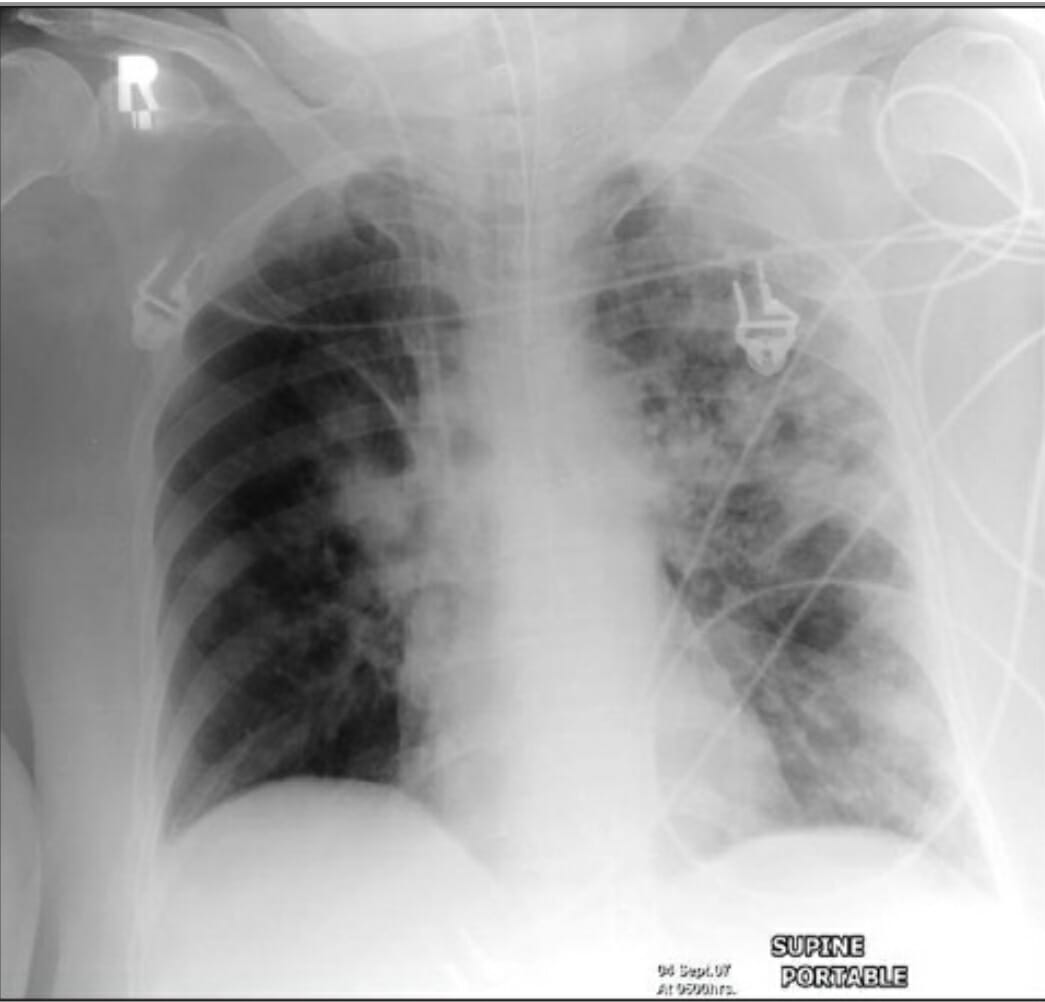
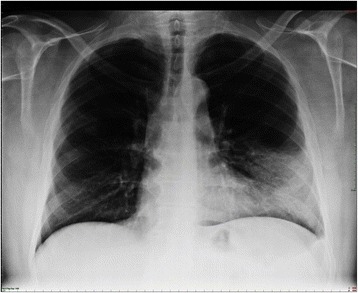
00:01 So when thinking about the examination for these patients, we wanna make sure we listen to the lungs. 00:06 You know, the lungs can have lots of different changes. 00:09 The classic thing we think about is that the lungs will have rhonchi which are kind of like a snoring sound. 00:14 I always say it's sort of what it sounds like. 00:17 The other things that can happen now or patients can have wheezing. 00:20 And this is due to the fact that when there's a pneumonia there or a possible other infection or a viral infection, the airways can become inflamed. 00:29 And that's basically what causes the wheezing. Some patients may also have wheezing on exam. 00:34 They can have tactile fremitus or egophony. 00:36 These are things that we do only occasionally in the emergency department. 00:40 We wanna go ahead cuz they can also help support or refute a possible diagnosis of pneumonia. 00:46 So you can go ahead and assess for the E to A changes as well as see if you feel any tactile fremitus. 00:52 In addition, there are more possible lung sounds. 00:55 Unilateral coarse crackles that could be heard in a localized lung zone are suggestive of an underlying consolidation. 01:03 Unilateral decreased air entry may suggest exudative pleural effusion, a common complication of pneumonia. 01:13 Other exam findings to think about. 01:15 You wanna look and see if your patient has a rash. 01:17 There are certain pneumonias or viral processes that can be associated with a rash. 01:22 Any patient who comes in with a cough or hemoptysis, it's a good idea to do an oropharyngeal exam. Take a look in their mouth. 01:29 Sometimes also if they're having upper respiratory symptoms, so look in their ears, possibly in their nose if you're worried that that could be a source of bleeding. 01:37 And then when thinking about the differential of consequence and potentially you're thinking about a pulmonary embolus. 01:42 Or is heart failure as a possible cause of the shortness of breath, you wanna take a look in their legs and see if they have any evidence of lower extremity swelling or edema. 01:51 You know, how are we gonna actually make the diagnosis? So, we're gonna definitely think about the patient and their presenting complaints and their physical exam. 01:59 And then we're gonna wanna move on to diagnostics. 02:02 You know, the chest x-ray is gonna be your most important test you're gonna get here. 02:06 And it's most important because it can be obtained easily, it can be obtained at the bedside and can give you a lot of information as to what's going on in the patient's lungs. 02:15 We'll look at a classic chest x-ray for lobar pneumonia in a moment. 02:18 Other testing that can be beneficial are basic blood tests. 02:23 So a CBC, a metabolic panel, an EKG which can look for any evidence of coronary syndrome, arrhythmias, can help you. 02:31 Potentially, this is something that can help if the patient is admitted to the hospital, a urinary strep or a Legionella antigen or a urine test that can be sent that look for possible strep infection or Legionella infection. 02:44 And strep is a common cause of pneumonia. Legionella, a little bit less common. 02:48 But important to know if that's what's going on. Influenza or other respiratory virus testing. 02:54 You know, depending on where you're practicing and what season it is, this test may have greater or less availability. 03:01 So in the winter months when influenza and viral illnesses are more common, this is gonna be much more readily available. 03:07 So in addition to influenza, other viruses that sometimes can cause these symptoms include RSV or rhinovirus and sometimes the testing for that can help. 03:17 Again, if your patient is admitted to the hospital, you wanna make sure if your patient does have influenza that they're not gonna go ahead and give influenza to their neighbor, to their roommate or to other people in the hospital. 03:29 So it has certain implications in those settings as well. 03:33 Also, a CT scan of the chest may be beneficial, especially if your chest x-ray doesn't show any evidence of pneumonia. 03:41 I've had lots of patients in whom the chest x-ray has been negative who they've gotten a CAT scan of their chest. 03:47 And that CAT scan has in fact shown pneumonia there that is present. 03:51 So while the chest x-ray is a good test, CT scan can sometimes give you additional information. 03:56 Additionally, thinking about that differential of consequence, if you're worried about a blood clot in the lungs, the CT scan, if you do it with IV contrast can also help take a look for that. 04:07 So, consider getting a CT scan if you're concerned about other processes that could be going on or potentially if your chest x-ray isn't revealing and you wanna get a closer look at the lung fields. 04:18 You know, we always wanna think about our risk-benefit ratio when we're thinking about whether or not to do our CAT scan cuz it does expose a patient to radiation. 04:25 So always keep that in mind when you're deciding whether or not to do this additional testing. 04:31 You know, other things to think about. So should you do blood cultures in pneumonia? You know, for sure if your patient is septic. 04:39 So, if they have evidence of sepsis by their vital signs or an elevated lactic acid or you're worried about it. 04:45 Blood cultures for sepsis are generally indicated and can be helpful. 04:49 However, for a majority of patients who present with pneumonia, blood cultures may not necessarily be a benefit. 04:55 And there are some studies that show that in a small -- very small proportion of patients who present with pneumonia, the blood cultures actually change course of management. 05:04 Now that's not to say they won't be positive. They very well might be positive. 05:07 But we know generally what bacteria will be causing a pneumonia. 05:12 So generally, we can check and do antibiotics that are gonna cover that specific pneumonia or cover kind of generally for pneumonia. 05:21 So blood cultures don't always necessarily make a difference in what we're doing for these patients. 05:27 How about sputum cultures? You know, sputum cultures are one thing that actually, potentially can change or make a difference in what you're doing. 05:34 The issue with sputum cultures is that you need to make sure that you're getting a sample from -- in the lungs. 05:39 What happens generally when you ask a patient to give up sputum culture is that they take the cup that you give them and they basically spit in the cup. 05:46 You don't want spit that's not gonna help you at all. 05:48 You want actually the gunk that's in their lungs to see what's in it. 05:53 So sometimes if you really want a sputum culture to kinda get additional information, you might have to have respiratory therapy come and help you get an induced sputum culture. 06:02 So the moral here is for septic patients, definitely go ahead and do blood cultures. 06:07 For other patients with pneumonia, it's a little bit more debatable and will depend on the culture of your institution. 06:13 Sputum cultures can potentially be of benefit, but you wanna make sure you're getting a good sample.
About the Lecture
The lecture Pneumonia and Pulmonary Infections: Examination by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
What is the cause of wheezing in patients with pulmonary infections?
- Inflammation of the airway
- Fluid accumulation within the alveoli
- Collapse of an alveoli
- Presence of consolidation
- Hyperinflation of the lungs
What is the most important diagnostic test for pulmonary infections?
- Chest x-ray
- Complete blood count
- EKG
- Chest CT scan
- Influenza testing
What is the indication for doing a blood culture in patients with pneumonia?
- Suspicion of sepsis
- Routine work-up for pneumonia
- Presence of hemoptysis
- Negative chest x-ray findings
- Non-productive cough
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |