Playlist
Show Playlist
Hide Playlist
Pulmonary Function Testing (PFT) – Laboratory Diagnostics
-
Slides Diagnostics PulmonaryFunctionTest RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
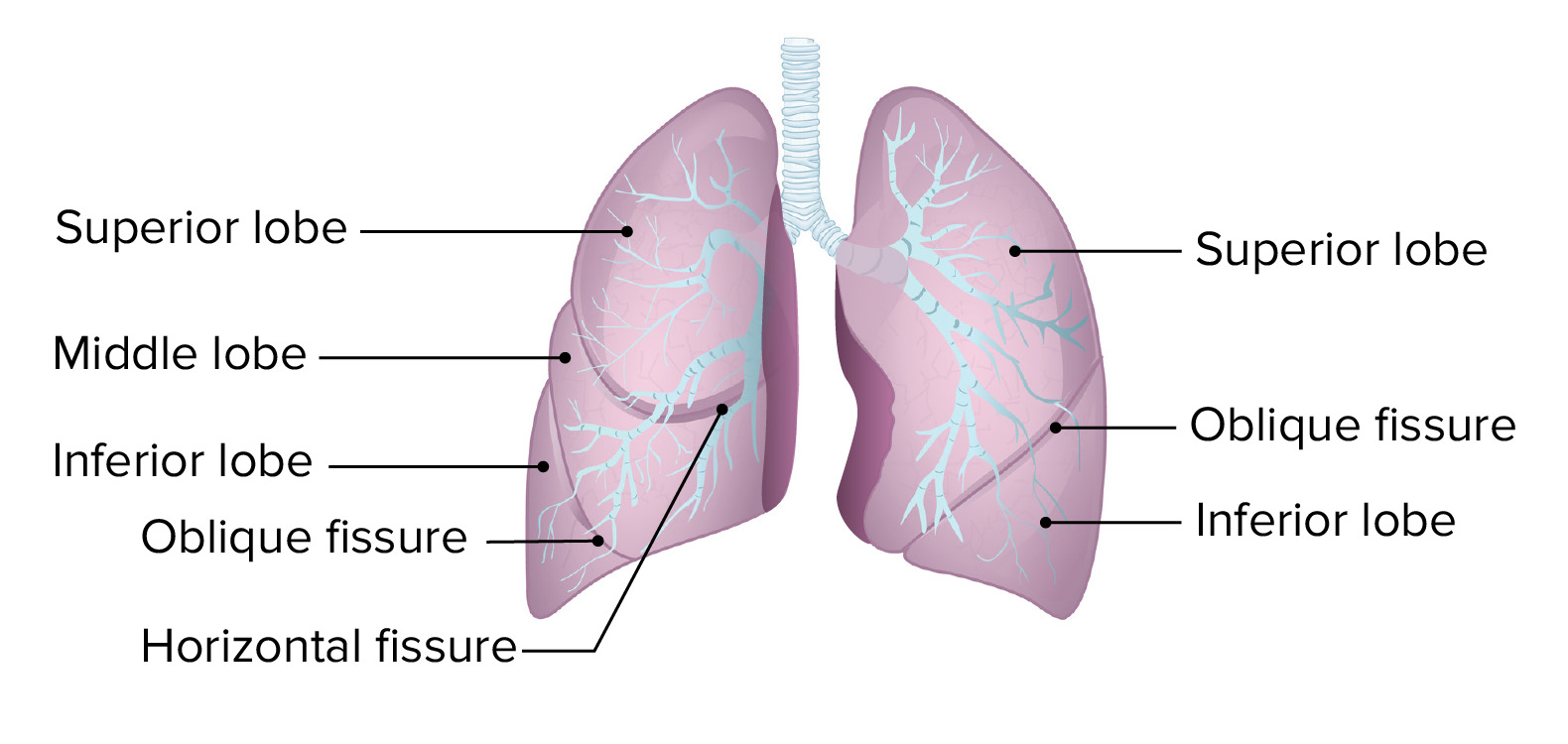
00:03 We have been dealing with the laboratory techniques quite a bit. And what we are doing here is making sure that we know as to who is coming in and how to properly assess the information that’s going to come at you. At this point, you should be extremely adept at being able to delineate as to when test is used when and for what reason. So, on that note, let’s begin by looking at pulmonary function tests. 00:28 Conventionally speaking, pulmonary function tests are used so that you can divide your obstructive versus restrictive lung diseases. With your pulmonary function tests and the type of graphs that we are going to create, you will see that you can get a heck of a lot more information out of it and what is expected of you at this junction in your medical education because of the evolution of the boards themselves. You will enjoy this because it’s building upon things that you already know. 00:53 Now, the three main categories of the testing include the following. We’ll take a look at spirometry, of course, which is probably the most famous of them all. And with this, it’s the ratio of FEV1 over FEC that we will take a look at. What does it actually mean? It means the amount of air that you are able to get out in one second, forced expiratory volume, one second, over the total amount of air that you physiologically are able to get out which is only limited by, what volume please? Good. Residual volume. You cannot exhale your residual volume completely. 01:32 Now, if it is obstruction, what does that even mean to you? It means that you cannot properly get your air out. You are obstructed. When that occurs, well, what kind of changes are we going to see? We will take a look. Must have a decrease in vital capacity and a decrease in total lung capacity for diagnosis of restriction. That is important and we will focus upon that. The obstructive part is quite simple. The obstructive means that, for the most part, I cannot significantly exhale. So, FEV1 is going to drop dramatically and you find that, well, for VC and TLC that for the most part, that will be a little bit different. 02:15 In restrictive, both VC and TLC must be decreased in order for you to diagnose restrictive. 02:21 You will see why. What kind of lung volumes become important for us, clinically? Total lung capacity and residual volume. 02:30 As I told you earlier, there is no way that you can possibly measure residual volume. 02:35 You must have a little bit of your air inside my lungs so that it does'nt collapse. Remember, it is always going to be at negative pressure. And that has to be kind of balanced by the fact that the chest wants to recoil, right? And so, therefore, that negative pressure has to remain and if you lose your air completely, well, that ends up being a problem and obviously, we will talk about that later. And blood or body plethysmography, in other words the "body box”, is really the gold standard for measuring the lung volumes. Plethysmography. 03:09 The other tests that we will take a look at is the diffusion capacity for carbon monoxide, and we will call this DLCO. Now, please understand, carbon monoxide is used for different reasons in pathology. Carbon monoxide, here, clinically, will be used to see as to how quickly, this is by proxy, by proxy, you will utilize carbon monoxide to see as to how quickly it then diffuses across that membrane into pulmonary capillary. So, therefore, it is a good measurement of gas exchange. This does not mean you take a patient’s mouth and put it over a car exhaust. That is not very nice. Nor are you going to do that. This is just a little bit of carbon monoxide for diagnostic purposes. Now, if by chance there was a patient who got exposed to carbon monoxide from a car exhaust in a closed environment, granted garage, but more importantly, as to what occurs on a regular basis. We will talk about this later, especially during the winter, where there might be fumes and gases coming out of in the basement heater, what not. Or maybe those of you that enjoy the sport of hockey. And sometimes, you know, it gets cold in there and so, people that work in those ice rinks accidently leave their car on in a closed environment and anyhow, that is carbon monoxide poisoning. You see the difference now? This is only for diagnostic purposes. 04:36 Both have heavy relevance for you and when the time is right, we will look at both. 04:42 Let’s take a look at an overview of your lung volumes and capacities. I will only focus upon the ones that you need on this graph. Clinically, this is obviously from physiology. So, begin by looking at tidal volume. Right there in the middle there, looks like a waves that are really tiny and that’s your tidal volume. See labelled as such, at the end of the graph there. The tidal volume does not require any effort. 05:07 It’s a fact that it’s quiet inspiration, quiet exhalation, that’s it. It’s approximately about 500, keep that in mind. As as we go through this, like we have been doing, there is going to be a lot of physiology involved only because we need to have this for clinical reasons. And then, well, that should go into breathing with inspired or great effort is then known as your inspiratory reserve volume. And once you go below your tidal volume with expiration, that is then known as your expiratory reserve volume. And so, some of these volumes that are important for us, however, include the following. 05:48 Residual volume. That is the last bit of air that we have in the lung that you cannot properly void. There is no way that you can do that on spirometry, but some of those volumes that we talked about with the body box and such might help you figure out your residual volume. 06:05 Next, the type of volume is the tidal volume, we looked at it. And then the capacities. 06:09 The capacities that are important for us include vital capacity. Take a look at vital capacity, Includes everything except our residual volume. Vital capacity is important for us because it then explains forced vital capacity. That is part of our pulmonary function test. And it is not really timed in terms of exhalation. The other big capacity that we need to take a look at is function residual capacity. 06:37 Functional residual capacity is more or less your control point. So, for example, when you have done your graphs. Your graphs, known as the-the graphs for inspiration-expiration, and the functional residual capacity be the control point, a ground zero in which, for example, if it is obstructed lung disease, then FRC is increased. If it is restrictive lung disease, FRC is decreased. We will talk more about that later. Total lung capacity is important for us. For example, here, a large lung, say that you see a huge lung on your AP diameter and also on your chest x-ray from anterior posterior, you find that there is a huge black areas of the lung where the diaphragm has then been pushed downward. That’s emphysema that I am referring to bilaterally. And there you can expect your total lung capacity to be increased. Okay, so those are some important volumes and capacitities that you want to keep in mind and that will be good enough for you to at least know what is going on clinically. Let's continue.
About the Lecture
The lecture Pulmonary Function Testing (PFT) – Laboratory Diagnostics by Carlo Raj, MD is from the course Pulmonary Diagnostics.
Included Quiz Questions
What does spirometry measure?
- FEV1/FVC
- TLC and RC
- Diffusion capacity of CO
- VC and TLC
- FEV1/TLC
Why can residual volume only be estimated?
- It cannot be expelled because prevents the lungs from collapsing.
- It is the amount of air that is fully diluted by N2 or He.
- It is responsible for the recoil of the chest wall.
- It represents limitations on airflow.
- It represents the surface area available for gas exchange.
Which of the following is the gold standard for measuring lung volumes?
- Body plethysmography
- Spirometry
- DLCO
- FEV1/FVC
- Gas dilution
What does vital capacity equal?
- Inspiratory capacity + expiratory reserve volume
- Inspiratory capacity + tidal volume
- Inspiratory reserve volume + tidal volume
- Inspiratory reserve volume + expiratory reserve volume
- Tidal volume + expiratory reserve volume
What is functional residual capacity?
- Expiratory reserve volume + residual volume
- Expiratory reserve volume + tidal volume
- Tidal volume + residual volume
- Vital capacity + residual volume
- Expiratory reserve volume + inspiratory capacity
Which of the following would you expect to find in emphysema?
- Increased TLC
- Decreased residual volume
- Increased tidal volume
- Decreased functional residual capacity
- Decreased total lung capacity
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |