Playlist
Show Playlist
Hide Playlist
Psoriasis
-
Slides Dermatology Inflammatory Skin Diseases.pdf
-
Reference List Pathology.pdf
-
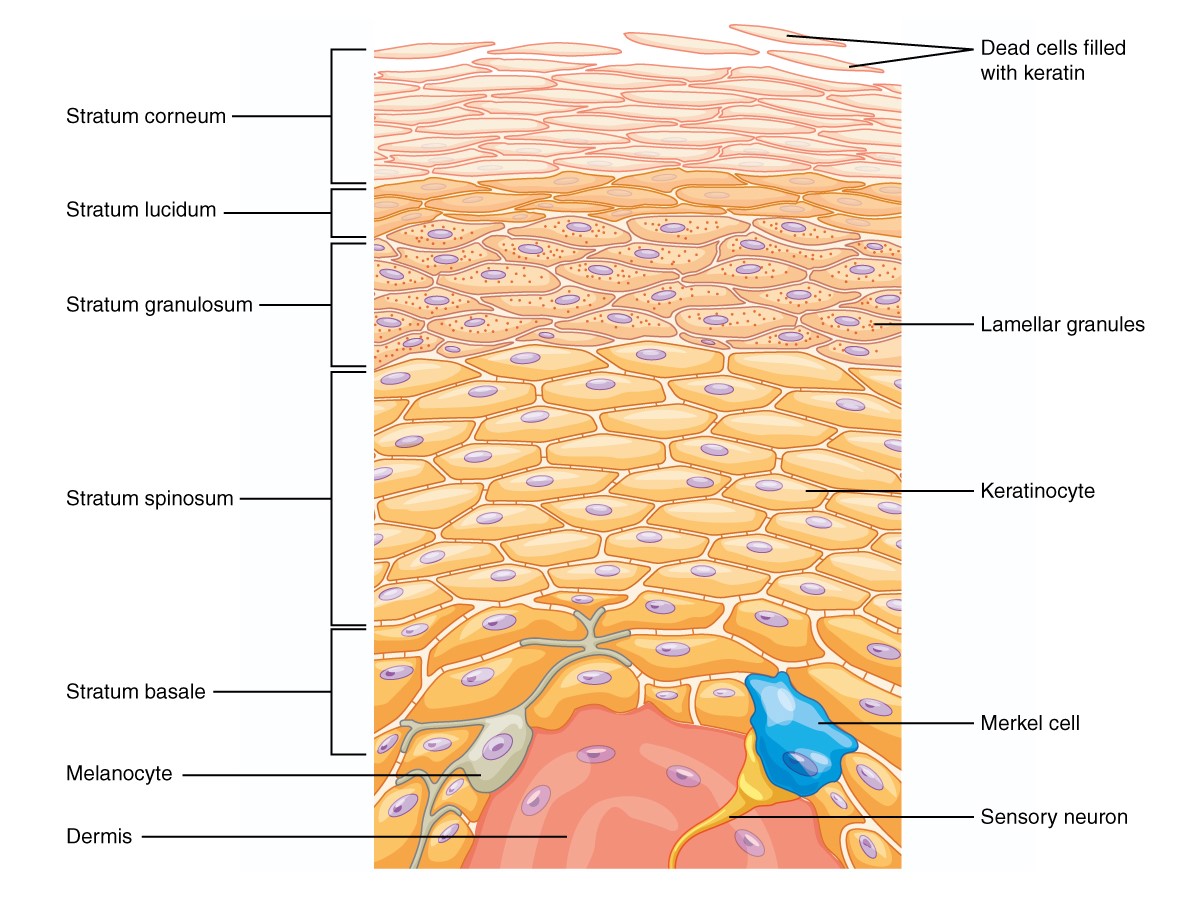
Download Lecture Overview
00:01 Our topic is a big one here, high-yield, definitely, for both the wards and your boards. 00:07 Demographics of psoriasis is my topic. 00:11 Look at this, a whopping 1% to 3% of Americans. 00:14 That’s a large population. 00:16 Do you understand that? The one-third of your psoriatic patients are going to report a family history though. 00:22 Now, for the most part, we’re unsure about what causes it, but as far as you’re concerned, you must look for trigger such as genetic and also environmental, which I’ll expand upon in a moment. 00:34 The morphology here includes, well, this is psoriasis. 00:37 As soon as you hear psoriasis, you should be thinking salmon, salmon, salmon-colored. 00:42 What does that even mean? If you have no idea what salmon is, well, that could be problematic. 00:46 But salmon might be pinkish and scaly. 00:49 Okay, so if you want, Google it, whatever, but salmon-colored erythematous plaque with thick silver scale, salmon-colored plaques. 00:59 Where would these be located? We’ll talk about distribution. 01:02 And obviously, by the time we come to the end of our discussion of psoriasis, we’ll take a look at differentials. 01:08 This is important. 01:10 You pay attention to the distribution of psoriasis. 01:12 Crucial: Elbows, knees. 01:15 Stop. 01:17 Elbows, knees. 01:20 Next, scalp and the gluteal clefts are typical. 01:27 The pruritus is a chief complaint in one-third of your patients. 01:30 In fact, unfortunately, the patients here who are genetically prone, perhaps, to psoriasis in which the itching might actually then trigger the psoriasis is called Koebnerization. 01:41 What did I say? Not to worry, I’ll repeat it again. 01:44 It’s called Koebnerization. 01:47 Nail changes include pits. 01:50 Stop there for one second. 01:52 Nails are important as a diagnostic feature. 01:57 In the nails, pits, what happens here is the fact that you’re going to start having dryness of the nail in which it looks like it’s flaking off. 02:07 So, this is not referring to spooning of the nails. 02:11 It’s not clubbing, okay? It’s not koilonychia, nor is this clubbing or hypertrophic osteoarthropathy, but this is the pits. 02:20 And so therefore, this is something that you want to keep in mind. 02:23 Nails are a big deal for psoriasis. 02:25 Diagnostic feature, keep that in mind. 02:28 And oil spots and nail loss. 02:33 Psoriasis, what else may possibly cause it apart from genetic environmental? Lithium and beta blockers can exacerbate psoriasis. 02:41 Look for a patient that maybe perhaps taken lithium to manage bipolarism or beta blockers. 02:48 Strep respiratory infection may perhaps trigger what’s known as a guttate type of psoriasis or lesions. 02:55 Remember, really unknown, that could be many, many triggers. 02:58 Apart from environmental and genetic, these are some common clinical ones. 03:02 And understand that psoriasis for the most part at this juncture, we’re referring to our dermatology, aren’t we? And we talked about these salmon-colored plaques that appear then as being silvery. 03:17 At some point in time, maybe your patient has a hard time bending over. 03:22 Down by the lumbar region, they lose their normal curvature. 03:26 They lose their normal curvature. 03:29 And so therefore, if you have vertebral involvement in psoriasis, now, at this point, you must categorize it as being psoriatic arthritis, and my goodness, it is debilitating. 03:41 That is no joke. 03:42 Is that clear? At this juncture, I need you to clearly pick out psoriatic arthritis as being debilitating. 03:52 With psoriatic arthritis then comes in that interesting description and discussion of HLA-B27 seronegative spondyloarthropathies. 04:05 Let’s take a look at the pictures here of psoriasis. 04:08 The one is beautiful here on your left, which then shows you the salmon-colored silver plaque, these flat elevations that you see on the left. 04:17 Look at the distribution, please. 04:18 We’re down by the lower back and there is the crevice of your buttocks, the gluteal region. 04:28 Maybe you have involvement of the head, and maybe perhaps, you have involvement of the hands, and take a look at the fingers and the nails. 04:34 It’s difficult to see the nails, but rest assured that if you were to then flip your hand over, the nails here will be pitted. 04:45 Pathology: So what’s happening to the skin, the keratinocytes? Is it undergoing thickening or is it undergoing thinning? It’s a plaque. 04:55 Well, I’m thinking that you are using common sense, and you know there’s thickening that’s taking place of the epidermis. 05:02 This thickening, clinically, is then referred to as being acanthosis versus acantholysis, right? Acanthosis, as the name implies, means thickened epidermis, referring to that plaque. 05:18 Can you picture that plaque for me that I just showed you? And you have elongated rete ridges. 05:26 This part is important, be careful. 05:29 So overall, you’ll have thickening of your keratinocytes or epidermis, but you’ll have thinning. 05:36 It’s very important for you to think about the layers of the epidermis; the corneum, granulosum, lucidum and so on and so forth, spinosum and basale. 05:45 But the granular layer is going to be either thin or absent. 05:50 Extremely important that you pay attention to that pathologic feature. 05:55 But overall, what happens with epidermis? Good, thickened. 06:00 Here’s a description. 06:02 Parakeratosis, and what that basically means is that you have the nucleus within the keratinocyte, which is then in the stratum corneum. 06:11 So, it’s going to be retained in the stratum corneum And with neutrophil microabscesses. 06:17 That is a very important description for psoriasis. 06:20 P as in psoriasis, P as in parakeratosis, which literally means there would be retention of the nuclei by the time you come in to the stratum corneum. 06:30 Remember the granulosum or the granular layer is either thin, or perhaps, even absent. 06:35 Quite characteristic of psoriasis. 06:38 Each one of these bullet points are very important pathologic features. 06:44 Here, we’ll take a look at actual histology of your psoriasis. 06:48 You’ll notice here that you have this rete. 06:50 These rete ridges are then thickened, and they are then literally invading down towards your dermis. 06:58 This thickening of your stratum spinosum, which is basically the thickest layer that you see here, is then referred to as been your acanthosis. 07:08 Management: Remember with psoriasis, it can be quite dangerous. 07:12 Every patient is going to present a little bit different with severity. 07:16 You can have certain patients in which you might find a little bit of dryness and a little bit of plaque, perhaps, on their skin. 07:22 Whereas, other patients, my goodness gracious, they have one patient in which she had to remove -- well, she has psoriasis, and when she was taking off her panties, literally, the skin was coming off with the panties itself. 07:33 So, this could be debilitating in terms of self-esteem in psychology. 07:37 So, be very, very careful as to how you discuss matters of psoriasis with your patient. 07:42 Topical. 07:43 In other words, your vitamin D type of derivative. 07:46 Oral retinoids, vitamin A, perhaps, derivative. 07:49 Methotrexate, cyclosporine, biologics including your TNF-inhibitors and we have light treatment, if at all available. 07:57 Basically, looking at what can you possibly do so that you can improve the quality of the skin, and also, improve the quality of your life of your patient. 08:06 We have vitamin A, vitamin D derivative steroids, and we have immunomodulators or suppressants such as methotrexate and biologics. 08:15 I’ll spend a second here to make sure that you’re quite familiar with the management of psoriasis. 08:21 Differential diagnoses: Here, we have eczema or dermatitis. 08:26 There are a couple of times when we have seen dermatitis or eczema. 08:30 We talked about a condition called atopic dermatitis. 08:33 And at this point, whenever you hear the term atopy, you automatically should be thinking about the triad. 08:38 The triad includes your asthma and then you have your rhinitis, and also, atopic dermatitis. 08:43 Extremely common in our society, industrialized nations, and may present with eczema, right? And remember, with the eczema, if it’s atopic dermatitis, then you’re thinking about a child in which maybe the cheeks might be involved, and maybe the extensors. 08:59 As a patient gets older, then now the eczema might be located where? Good. 09:04 Maybe on the flexors. 09:05 Usually involves your flexors rather than extensor areas if the patient is older. 09:10 Eczema has a more exudative weeping type of appearance versus psoriasis which has what? A plaque-like issue. 09:17 And lacks the distinctive dry silver scale that you’d find with psoriasis. 09:23 A couple of clinical pearls here that you want to identify eczema with immediately. 09:26 Weeping type of appearance of your vesicles, have you? And the fact that you might be exposed to some kind of antigen. 09:37 As a differential, a secondary syphilis. 09:40 Why? Well, with secondary syphilis, generally, smaller plaques. 09:45 I’ll walk you through syphilis soon enough. 09:47 And plasma cells and possibly even spirochetes by biopsy. 09:51 So, it would be very clear to you as a differential that secondary syphilis is present versus it being psoriasis. 09:57 Tinea corporis. 09:58 This time, where are we? Corporis means body, okay? Not usually in such characteristic locations. 10:05 So for example, psoriasis, remember, I told you to memorize your elbows and knees, and also, your scalp and gluteal cleft, and I even showed you a picture of the gluteal cleft with psoriasis. 10:18 With tinea, which is then an organism, and affecting the body, an active scaling border with central clearing. 10:25 Oftentimes referred to as being your -- well, unfortunately, as a differential, we’ll talk about this later, at times, this has been called the ringworm, and it’s actually not at all a worm. 10:37 Take a look at the second bullet point here. 10:39 And we have an active scaling border. 10:42 In other words, an erythematous border with the central clearing. 10:45 So therefore, in layman’s terms, has been described as being ringworm but it has nothing to do with a worm. 10:52 We’ll talk about this again, but this is very distinctive for tinea corporis versus in psoriasis, what are you going to find? Your silvery salmon-colored plaque.
About the Lecture
The lecture Psoriasis by Carlo Raj, MD is from the course Inflammatory Skin Diseases.
Included Quiz Questions
A 45-year-old man with coronary artery disease presents with a worsening chronic rash of salmon-colored erythematous plaques with a thick silvery scale appearance. What medication might he be taking that can exacerbate his condition?
- Beta-blockers
- Calcium channel blockers
- Diuretics
- Nitrates
- Warfarin
Which of the following pathologic features is characteristic of psoriasis?
- Parakeratosis with neutrophilic microabscesses
- Acantholysis
- Thickened granular layer
- Epidermal thinning
- Shortened rete ridges
Which of the following vitamins is used as a topical treatment in psoriasis?
- Vitamin D derivatives
- Vitamin E derivatives
- Vitamin K derivatives
- Vitamin C analogs
- Vitamin B1 analogs
How is psoriatic arthritis described in the context of psoriasis management?
- As a debilitating condition that needs to be clearly identified
- As a mild and easily treatable condition
- As a skin condition that does not affect the joints
- As a rare complication affecting only elderly patients
- As a condition best managed with light treatment only
What other common skin condition is in the differential diagnosis of psoriasis?
- Eczema
- Actinic keratosis
- Squamous cell carcinoma of the skin
- Cutaneous T cell lymphoma
- Scabies
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The derm lectures have been surprisingly helpful and as always Dr Raj keeps it clear, funny, and to the point.
HE HAS TAKEN THE BEST EFFORT IN EXPLAINING THE TOPIC AND HAS PRESENTED IT WELL AND IN A STUDENT FRIENDLY MANNER.
Love this guy! Easy to listen to. Puts emphasis on important points. And occasionally says something surprisingly funny. "Rubber Baby Bumper Buggies" lol