Playlist
Show Playlist
Hide Playlist
Proximal Convoluted Tubule (PCT): Type 2 (Proximal) RTA
-
Slides PCT ClinicalEffectsSyndromsandDiseases RenalPathology.pdf
-
Reference List Pathology.pdf
-
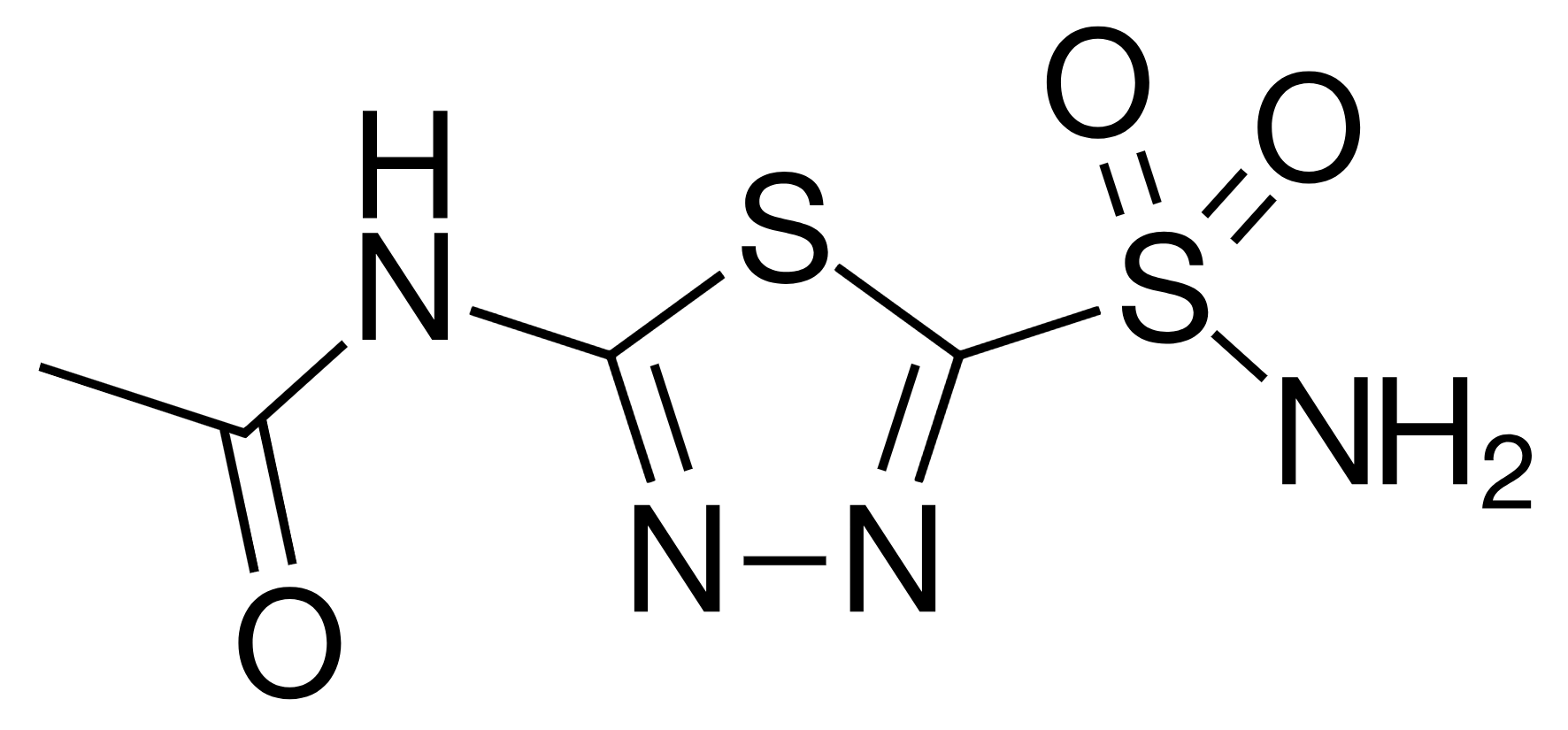
Download Lecture Overview
00:01 RTA type II, well where am I? Proximal convoluted tubule. Bottom line is inside of the picture, luminal membrane, what's in that lumen? Urine. Epithelial cell, what kind? PCT and there is my blood. Here you see the red X represents either a patient genetically was missing carbonic anhydrase, you can pharmceutically induce this by giving which drug? Something like acetazolamide to inhibit that carbonic anhydrase. Or what if you had a condition such as Fanconi syndrome that is causing complete destruction of the proximal convoluted tubule and in any of the cases that I just gave you in terms of numerous etiologies, what have you done to renal threshold for reclaiming bicarb? You have decreased it. When doing so, out goes the bicarb, you end up having a pH in your blood that is decreased. Welcome to RTA type II. Please do not miss this. What I wish to bring to your attention, once you diagnosed your patient metabolic acidosis, this next step that you have to take clinically every single time is called anion gap. Anion gap means what? Keep it simple. Cations minus the anions. 01:28 The only cation that you will be taking into consideration clinically is sodium, why? 135 to 145 is normal. Calcium is the other cation, but it's only 3.5 to 5, so let that go. Anions, there is two of them. 01:45 So from your cation, sodium, you will subtract your anions. Those include your chloride, which is between 95 to 105 and every bicarb between 22 to 26. This is something once again you have doubt with in acid-base physiology. Make sure you know about anion gap, when is the only time that you will be using this clinically? Metabolic acidosis, right? And here RTA type 2, there is a normal anion gap. All renal tubular acidosis, normal clinically is called nonanion gap metabolic acidosis. What is normal anion gap? Between 8 and 12. Don't worry. This is our first time in which we are dealing with anion gap. There is plenty of more places where we will do anion gaps. If you miss this, first time round, go back and repeat or bear with me here because we will see this over and over again. Type II, impaired reabsorption of bicarb, outer it goes. Welcome to RTA type II. Or with type 2, there might be impaired secretion of your hydrogen. Remember when you say renal tubular acidosis, be careful, what is that acidosis referring to? The acidosis is referring to the blood. Is that clear? That is your pathology. This is not aciduria. This is renal tubular acidosis so this would be of the blood. Or like we said, effective or deficiency of carbonic anhydrase. Large amounts of bicarb are gone and generalized PCT dysfunction may also result in large loss of bicarb such as Fanconi. Discussed this plenty. Inhibitors and other conditions causing damage to the PCT. Myeloma, we will head over and over again. Drugs that are nephrotoxic and cystinosis, which is rare, but could be an inherent cause of damage to the proximal convoluted tubule.
About the Lecture
The lecture Proximal Convoluted Tubule (PCT): Type 2 (Proximal) RTA by Carlo Raj, MD is from the course Diseases of the Nephron.
Included Quiz Questions
Which of the following amino acids is not affected in cystinosis?
- Tryptophan
- Cysteine
- Arginine
- Lysine
- Ornithine
Which of the following symptoms would you expect to find in a patient with cystinuria?
- Nephrolithiasis
- Cerebellar ataxia
- Depression
- Photosensitivity
- Megaloblastic anemia
Which of the following statements is incorrect regarding proximal renal tubular acidosis?
- It is due to defective bicarbonate secretion.
- It is due to a deficiency of carbonic anhydrase.
- It is due to impaired reabsorption of bicarbonate.
- The site of occurrence is the PCT.
Which of the following vitamins is deficient in Hartnup disease?
- Niacin
- Cobalamin
- Pantothenic acid
- Biotin
- Thiamine
Which of the following is a rare and inherited cause of type 2 renal tubular acidosis?
- Cystinosis
- Nephrotoxic drugs
- Acetazolamide
- Carbonic anhydrase inhibitor
- Myeloma
Which of the following changes would you expect to see in a patient with type 2 renal tubular acidosis?
- Increased urine pH early in the disease
- Metabolic alkalosis
- Increased plasma pH
- Anion-gap metabolic acidosis
- Aciduria
Which of the following anion gap values would likely indicate type 2 renal tubular acidosis?
- 10
- 14
- 16
- 19
- 21
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |