Playlist
Show Playlist
Hide Playlist
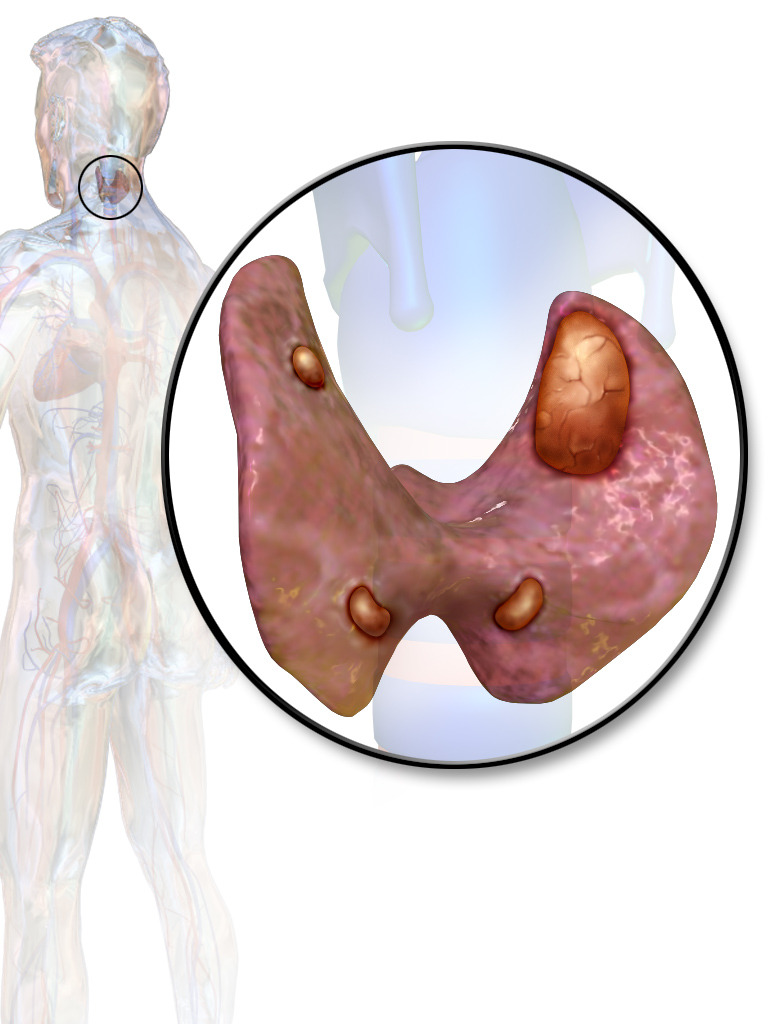
Primary Hyperparathyroidism
-
Slides Calcium Metabolis.pdf
-
Reference List Endocrinology.pdf
-
Reference List Metabolic Bone Disorders.pdf
-
Download Lecture Overview
00:01 Here are some of the radiologic features of primary hyperparathyroidism. 00:05 Subperiosteal bone resorption is the most consistent finding. 00:09 Most commonly, this involves the terminal tufts of the phalanges. 00:13 Osteitis fibrosa cystica is characterized by cystic bone spaces filled with brown fibrous tissues, otherwise known as brown tumors and are illustrated here in the image on the right. 00:27 Parathyroid hormone mediated hypercalcemia or primary hyperparathyroidism is the common cause. 00:33 It's diagnosed by a combination of elevated serum calcium and an inappropriately normal or elevated intact PTH level. 00:40 Peaks in the 7th decade and mostly affects women in 75% of cases. 00:46 Before the age of 45 years, similar rates occur in men and women. 00:51 Approximately 80% of patients will have elevated PTH levels with simultaneously elevated calcium levels. 01:00 Most commonly, it is due to a single parathyroid adenoma but rarely, it may be due to multi-gland hyperplasia. 01:08 This is typically seen in patients with end-stage kidney disease. 01:12 Also, multiple endocrine neoplasia syndrome should be thought of whenever a patient presents with primary hyperparathyroidism and we'll review this condition a little later in the lecture. 01:23 Parathyroid gland carcinomas typically present with calcium levels greater than 14 mg/dL and intact parathyroid hormone levels greater than 250 pg/mL. 01:36 Fortunately, this is a very rare manifestation. 01:39 Once primary hyperparathyroidism is diagnosed, measurement of serum phosphorus should always be done. 01:46 It's typically low or normal and helps to differentiate it from other causes of hypercalcemia. 01:52 A 24-hour urine calcium is elevated in 50% of the patients. 01:57 Serum 25-hydroxyvitamin D levels if low, the body converts more 25-hydroxyvitamin D to 1,25-hydroxyvitamin D and thus may have elevated levels of 1,25-hydroxy vitamin D on serum analysis. 02:14 Looking at the treatment of primary hyperparathyroidism, we divide this into symptomatic patients and asymptomatic patients. 02:22 In those patients who present manifesting symptoms of hypercalcemia, severe bone disease or fractures, overt neuromuscular dysfunction or kidney stones, they require parathyroidectomy. 02:36 When will we decide to do a parathyroidectomy in an asymptomatic patient? There are a number of guidelines for this including: patients who are younger than 50 years of age, those who are unlikely to follow up, those with a serum calcium that is greater than 1 mg/dL above normal range, those whose creatinine clearance are less than 60 mL/minute, those who have osteoporosis with a T-score that is less than -2.5, a 24-hour urinary calcium that is greater that 400 mg a day and those who have nephrolithiasis or nephrocalcinosis. 03:12 In terms of the surgical complications of parathyroidectomy, the first one to be aware of is post-operative hypoparathyroidism. 03:20 There also might be damage to the recurrent laryngeal nerve. 03:25 In terms of modern, surgical techniques with the increased use of sestamibi scans, high definition ultrasound and intraoperative measurements of PTH levels, minimally invasive techniques for removing the parathyroid glands are now preferred. 03:41 Minimally invasive surgery allows for a smaller incision and a shorter surgical duration. 03:48 For patients who do not meet criteria for surgery, surveillance usually consists of an annual measurement of serum calcium and monitoring of serum creatinine levels. 03:59 A 3-site dual-energy x-ray absorptiometry scan or DEXA scan should be performed every 1 to 2 years to evaluate the bone mineral density of the lumbar spine, the hip and the distal radius. 04:13 The frequency of DEXA scanning should increase to yearly when any treatment has been initiated for bone health or medications have been added that may affect the bones. 04:23 These could include anti-androgens, anti-estrogens, anti-seizure medications and especially glucocorticoids. 04:32 In treating patients with asymptomatic primary hyperparathyroidism, one must aim to maintain adequate vitamin D levels, 400 to 600 Units per day and to prevent further parathyroid hormone stimulation. 04:46 In patients with concomitant vitamin D deficiency, repletion is recommended to replete patients to whose levels are below 30 ng/dL, with careful attention to urine calcium excretion and serum calcium levels once the values are greater than 30 ng/dL. 05:05 Adequate physical activity must be performed to prevent bone resorption and adequate hydration should always be recommended to prevent kidney damage as imperative recommendations. 05:18 Parathyroid carcinomas fortunately are very rare. 05:21 Mutations of the HRPT2 gene are usually the culprits. 05:26 Inactivation of this gene can lead to familial hyperparathyroidism. 05:31 Associated with a total serum calcium level greater than 14 mg/dL and very high parathyroid hormone levels that are typically greater than 4 times the upper limit of normal. 05:43 Most patients present with a single gland involvement. 05:48 It may not be histologically different from benign adenomas and a local spread from the capsule distant metastases or lymph node involvement must be present for the carcinoma to be diagnosed. 06:01 Surgical resection is the treatment of choice and all patients should be screened for the HRPT2 gene. 06:08 And if positive, family members are screened as well.
About the Lecture
The lecture Primary Hyperparathyroidism by Michael Lazarus, MD is from the course Metabolic Bone Disorders. It contains the following chapters:
- Primary Hyperparathyroidism
- Treatment for PHPT
- Parathyroid Carcinoma
Included Quiz Questions
Which of the following is a common imaging finding in a patient with hyperparathyroidism?
- Subperiosteal bone resorption
- Subperiosteal hematoma
- Subperiosteal abscess
- Subperiosteal hemangioma
- Subperiosteal formation of new bone
What is the most common cause of primary hyperparathyroidism?
- Parathyroid adenoma
- Parathyroid gland carcinoma
- Multi-gland hyperplasia
- Pituitary adenoma
- Multiple endocrine neoplasia (MEN) syndrome
Which of the following is a major postoperative complication of parathyroidectomy? Select all that apply
- Recurrent laryngeal nerve damage
- Superior vena cava syndrome
- Asthma
- Cervical radiculopathy
- Postoperative hypoparathyroidism
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |