Playlist
Show Playlist
Hide Playlist
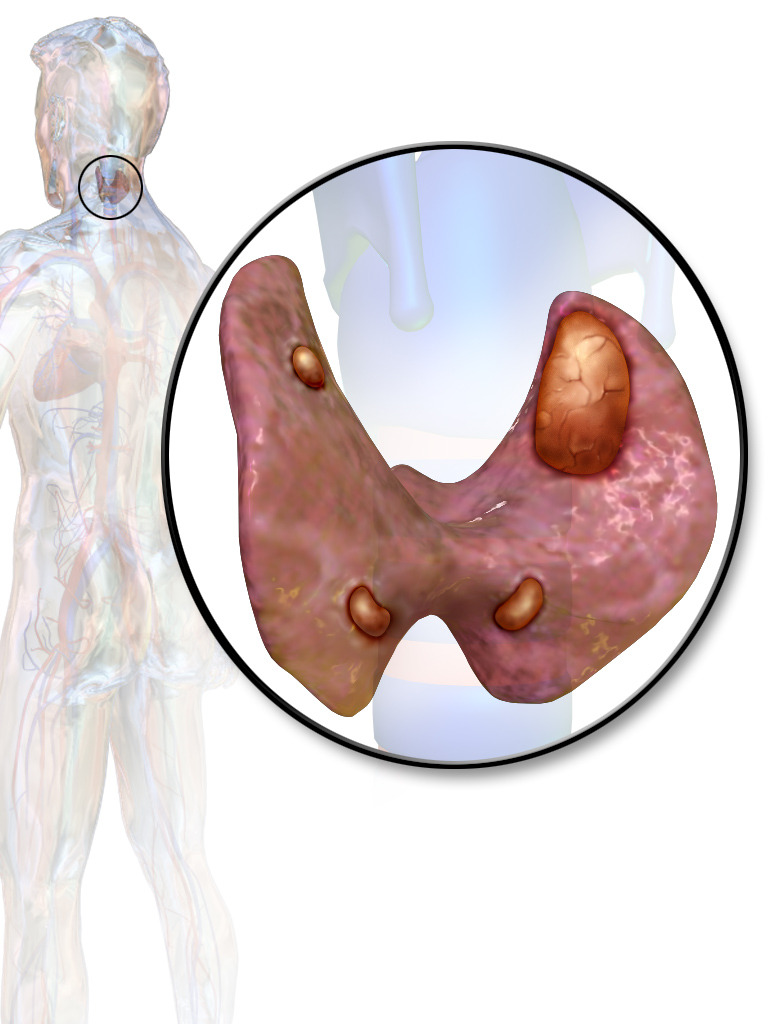
Management of Primary Hyperparathyroidism
-
Slides Hypercalcemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:01 The management of primary hyperparathyroidism, what you do here is you, pre-operatively, you try to localizing getting baseline of your PTH. 00:10 Do a Sestamibi Scan. 00:11 I showed you a picture of a Sestamibi Scan where there was a solitary adenoma of the parathyroid. 00:17 If you’ve forgotten, please take a look at the previous discussion where I very much showed you that, that’s important. 00:22 Ultrasound could also help with establishing your baseline. 00:26 Indication of parathyroidectomy, so if you actually need to remove the parathyroid because of this excess calcium, what are the indications? Symptomatic hypercalcemia; calcium at least 1 milligram per decilitre greater than normal; age under the age of 50, 24 urine calcium of being greater than 400 milligrams. 00:44 The bone density here, unfortunate well, not show enough bone because of increased osteoclastic activity and the calcium stones are found in the kidney. 00:54 All of these to you represent hypercalcemia. 01:00 Whenever your patient starts becoming symptomatic with hypercalcemia and you know for a fact that it’s being caused by primary hyperparathyroidism, it’s time for you to start thinking about moving the parathyroid now. 01:12 What you find to be interesting is anytime that you start doing surgery upon an organ, what is the possibility always? There is every possibility that you might take out too many parathyroids; you might take out too much of that organ is my point. 01:26 If you take out too much of the organ or you might have collateral damage, say there’s a nerve passing through there, but in this case, if you take out too much parathyroid, then your patient is rendered hypoparathyroid. 01:36 And if the patient is suffering from hypoparathyroidism, obviously, hypocalcemia maybe tetany. 01:43 During a surgical excision you can do a stat PTH 10 minutes after excising what you think to be the adenoma PTH has a half life of only 3-5 minutes So a subsequent drop in the PTH levels will confirm the tumor removal. 01:58 And if you’re drop below 50 percent, stop please; if not, then you keep cutting, cutting, cutting; if by chance you cut too much, we just said, may result in hypo… hypoparathyroidism. 02:11 Medical therapy, bisphosphonates to decrease fracture risk and something called Cinacalcet which lowers PTH secretion. 02:19 So, it’s a calcimimetic. 02:22 Imagine we give a calcimimetic, the body gets fooled and so, may... 02:26 Now, this is interesting, right? How many times have we dealt with management in which, for example, polycystic ovarian syndrome, when you know your patient has too much estrogen and you’re giving the patient perhaps low dose of or contraceptive pill with estrogen, why? Because the body actually may respond to this mimetic, even though within the body itself there might be too much of that very substance that you’re giving in vivo. 02:54 Clear? Be careful. 02:56 So, calcimimetic might actually respond, the patient might actually respond to it and therefore, may lower the PTH. 03:02 Obviously, this is not cure; this is for management.
About the Lecture
The lecture Management of Primary Hyperparathyroidism by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
What is NOT an indication for removal of the parathyroid gland?
- A patient over the age of 50
- Symptomatic hypercalcemia
- Calcium at least 1 mg/dL greater than normal
- 24 hour urine calcium > 400mg
- Estimated glomerular filtration rate (eGFR) < 60 mL/min
Why are serum PTH levels helpful during the excision of parathyroid adenoma?
- PTH half-life is only 3-5 minutes.
- PTH can increase drastically when glands are disturbed during surgery.
- Indicates if the thyroid is affected by surgery
- Serves as a marker for post-surgical prognosis
- Predictably increases by 50% before dropping to normal levels
What is the mechanism of action of cinacalcet?
- It is a calcimimetic that produces negative feedback, lowering PTH.
- It is an inactive analog of PTH, leading to increased calcium excretion.
- It directly promotes bone mineralization and decreases fractures.
- It is a calcimimetic that tricks the body into releasing more PTH in order to identify the diseased parathyroid gland.
- It causes positive feedback on calcium absorption in the gut.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |