Playlist
Show Playlist
Hide Playlist
Precocious and Delayed Puberty
-
Slides PrecociousPuberty PediatricGynecology.pdf
-
Download Lecture Overview
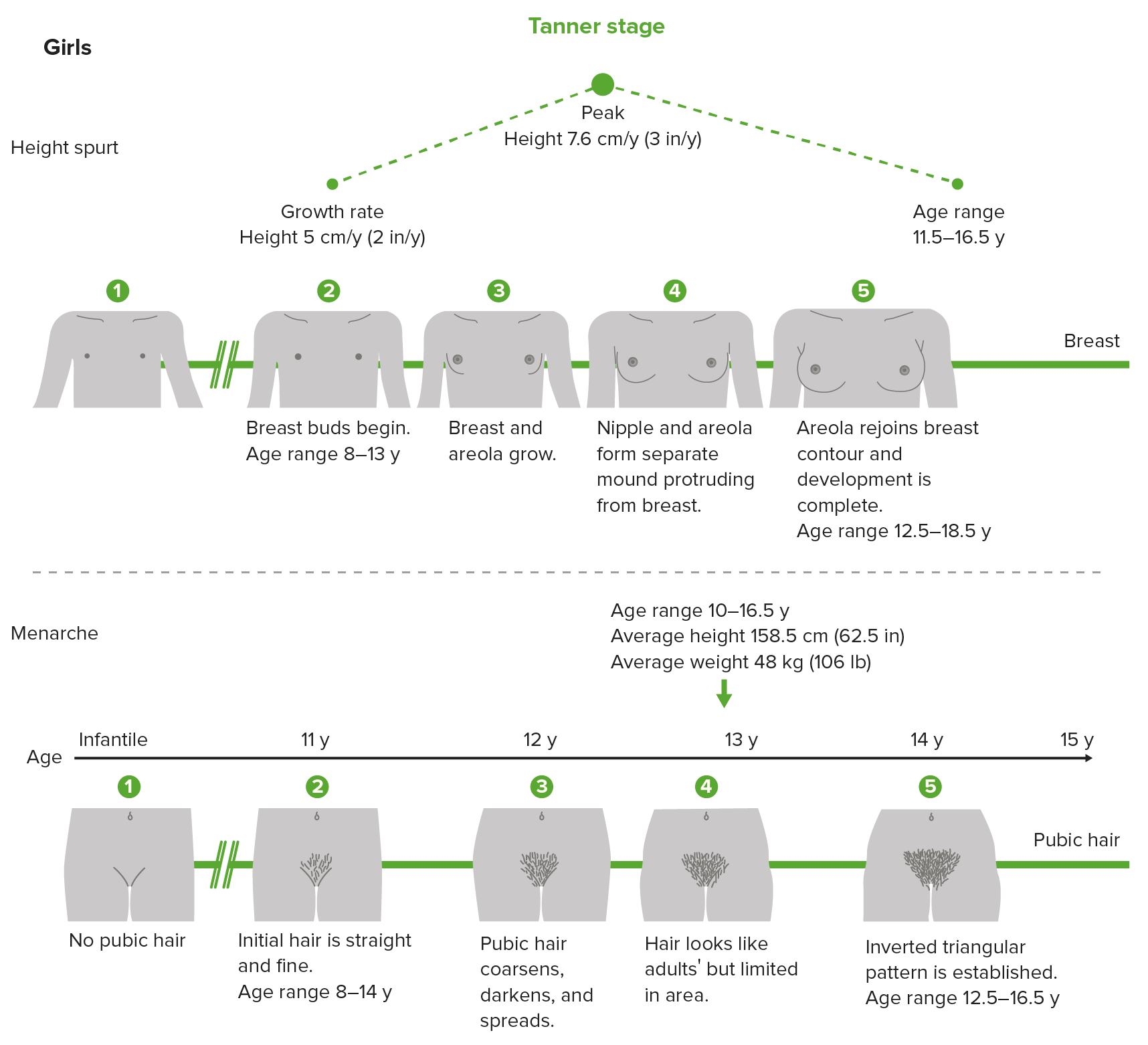
00:01 Hi. In this lecture we're gonna review pediatric gynecology, precocious puberty and evaluation and management. 00:08 Let's get started. 00:10 Precocious puberty is essentially pathologic. 00:15 All girls less than 6 years old who have either thelarche or puberche merit an evaluation. 00:21 Girls less than 8 with both actually merit an evaluation. 00:26 And girls with isolated premature thelarche or puberche merit at least an H and P or history and physical plus bone age with follow up. 00:35 There are some factors that is associated with intracranial pathology. 00:40 This usually happens when you have a patient who's less than 6 years old. 00:45 If you have rapid progression you should think there could be something happening at the level of the CNS. 00:51 If the patient has headaches this is also an indication. 00:54 She also may present with neurological deficits or seizures. 00:58 Let's now talk about the 2 types of precocious puberty. 01:04 Gonadotropin dependent or gonadotropin independent. 01:08 In gonadotropin dependent, you have early activation of the HPO axis and development is isosexual. 01:16 That means if you are a girl you're developing into a woman, or if you're a boy you're developing into a man. 01:23 90% of cases are idiopathic, we don't know why they are happening. 01:28 And can be associated with CNS lesions, irradiation, and trauma. 01:33 Again, gonadotropin independent, it is not reliant on FSH or LH. 01:38 Results from excess secretion of sex steroids from ovaries or maybe from exogenous sources. 01:45 This will be the case if maybe a young girl is ingesting oral contraceptive pills from her mom. 01:52 This also happens with autonomously functioning ovarian cysts and they are one of the most common causes. 01:59 Other ovarian tumors such as granulosa cell, intertola Leydig cell are rare causes. 02:06 Let's now talk about McCune Albright Syndrome. 02:10 This seems to be a favorite of the USMLE. 02:13 This is cause by an alpha subunit mutation of the G protein or GNAS1 gene. 02:20 This is a rare disorder so you probably won't see it on the wards but if you get lucky you might know about it already. 02:27 Again, this is a rare disorder whose clinical manifestation usually presents with precocious puberty. 02:34 They have this characteristic café-au-lait spots and also can polyosotic fibrous dysplasia of the bone. 02:42 Notice the irregular contour of this patient's café-au-lait spots. 02:47 Again with McCune Albright Syndrome, these patients can also suffer from gigantism, as well as Cushing Syndrome, thyrotoxicosis and adrenal hyperplasia, making the diagnosis quite difficult. 03:03 With McCune Albright Syndrome, the sequence of pubertal development may be abnormal, i.e. there is some bleeding before you even have thelarche. 03:14 In a typical pubertal development you should have breast development before menarche. 03:19 So again, this is abnormal in the McCune Albright Syndrome. 03:23 Let's go through a diagram of how to diagnose and work up precocious puberty. 03:30 With bone age you essentially have an x-ray of the left hand. 03:35 This is compared to x-rays of normal children at different ages. 03:39 If you have a bone age and you have breast and pubic hair development, you need to do a stimulation test. 03:46 If you have breast or pubic hair and accelerated growth, you still need to do a GnRH stimulation test. 03:54 If you have breast or pubic hair only, then likely you have incomplete precocious puberty. 04:01 This is typically gonadotropin independent. 04:05 Gonadotropin-dependent precocious puberty actually if you have a positive stimulation test should lead you to do an MRI and a TSH and free T4 to rule out clinical hypothyroidism. 04:20 In the gonadotropin-independent precocious puberty, you should do an estradiol and testosterone, an hCG, a DHEA-S and a p.m. Cortisol and 17OHP. 04:32 Essentially you're looking for in-organ problems that are causing this gonadotropin-independent precocious puberty. 04:39 In all of this patients, they should have an abdominal or pelvic ultrasound to rule out again an in-organ issue causing a precocious puberty. 04:49 Let's now talk about delayed puberty. 04:54 This is actually the inverse of what we've been talking about up until now. 04:57 Are you ready? By age 12 in the US, 95% of girls have some breast development. 05:03 However, not all girls go into puberty at the same time and since we don't know what causes puberty or starts puberty, then we can't really tell who's delayed sometimes and who's on time. 05:16 Refer to the slides at about normal puberty to learn more. 05:20 If you have an inactive hypothalamic pituitary ovarian axis, this is called hypogonadotropic hypogonadism or hypo-hypo just for short. 05:31 If you have ovarian insufficiency or ovarian failure such as with Turner syndrome, which is discuss in another lecture set. 05:39 You can have ovarian failure and this is called hypergonadotropic hypogonadism, so now hyper-hypo. 05:48 This can be the first sign of an occult metabolism problem such as IBS, irritable bowel syndrome or hypothyroidism. 05:57 Delayed puberty in terms of the most common cause is hypo-hypo. 06:02 That is hypogonadotropic hypogonadism, This is the case when you have GnRH deficiency. 06:09 One genetic cause for this will be Kallman Syndrome, recall that these patients have an anosmia. 06:16 Also, this can be cause by hypothalamic/pituitary tumors. 06:22 There are endocrinologic causes such as hypothyroidism and elevated prolactin and functional hypothalamic amenorrhea such as eating disorders, chronic stress and these can all lead to delayed puberty. 06:38 Again, if you have delayed puberty or delayed breast and pubic hair development get a bone age. 06:45 If they're way off in their chronological age that potentially can help you and assist you in the diagnosis. 06:51 You should also obtain an FSH, estradiol and an LH. 06:56 If you discover the patient has hypergonadotropic hypogonadism you should obtain a karyotype. 07:04 A Turner Mosaic would definitively have delayed puberty. 07:08 Also a Turner 45,XO would also have delayed puberty. 07:13 With hypogonadotropic hypogonadism you should obtain an MRI to rule out a CNS pathology. 07:21 Also, obtain a CBC, an ESR and LFTs. 07:27 Prolactin, TSH, and Free T4, and DHEA/S should also be obtained. 07:33 Thank you for listening and good luck on your exam.
About the Lecture
The lecture Precocious and Delayed Puberty by Lynae Brayboy, MD is from the course Pediatric Gynecology.
Included Quiz Questions
Which of the following statements is FALSE regarding precocious puberty?
- Girls who experience menarche at the age of 12 must be evaluated for precocious puberty.
- All girls less than 6 years old with either thelarche or pubarche require evaluation for precocious puberty.
- All girls less than 8 years old with both thelarche and pubarche require evaluation for precocious puberty.
- All girls less than 8 but older than 3 with isolated premature thelarche or pubarcheo should have at least a history and physical and bone age follow up.
Which of the following is associated with gonadotropin-dependent precocious puberty?
- Cranial irradiation
- Exogenous steroids
- Autonomously functioning ovarian cysts
- Granulosa cell tumor
- Leydig cell tumor
Which of the following is NOT associated with McCune Albright syndrome?
- Neurofibromas
- Gigantism
- Cafe-au-lait spots
- Polyostotic fibrous dysplasia
- Precocious puberty
Which of the following tests should be performed on patients with gonadotrophin dependent precocious puberty?
- Brain MRI
- Estradiol
- Testosterone levels
- Beta HCG leves
- DHEAS levels
Which of the following conditions can be the first sign of an occult metabolic problem such as irritable bowel syndrome or hypothyroidism?
- Delayed puberty
- Precocious puberty
- McCune Albright syndrome
- Granulosa cell tumors
- Leydig cell tumor
Which of the following factors does not suggest an intracranial cause of precocious puberty?
- Onset after 8 years
- Rapid progression
- Headaches
- Neurological deficits
- Seizures
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |