Playlist
Show Playlist
Hide Playlist
Polymyositis
-
Slides Inflammatory Myopathies.pdf
-
Download Lecture Overview
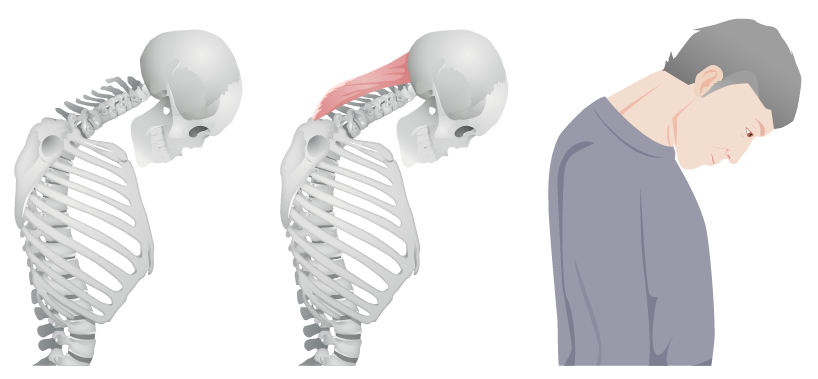
00:00 So, let's walk through each of the major categories of inflammatory myopathies and understand how they present, how they are similar, and how they are different. And we're going to start with polymyositis. Polymyositis begins subacutely. Patients present with several weeks or sometimes several months of progressive weakness that is getting worse and worse over the course of days and often weeks. The distribution is symmetric. There's just as much weakness on the right side as the left side and typically there's not prominent asymmetry in the patient symptoms or signs. This is a painless condition. There's not myalgias; there's myopathy or weakness. This is often proximal more than distal and so we see patients describe difficulty with getting up out of chairs. They are now having to use their hands. Or walking upstairs, they are using the rail. They have difficulty getting to the top cabinets, so everything is low in their house. And that's the typical symptoms that we would see from a patient suggesting a proximal distribution. There are no sensory changes and reflexes are normal to decreased indicating that this is localizing to the muscle. And you can see here a typical pattern for a patient presenting with polymyositis with proximal, limb and shoulder girdle weakness that's present in the proximal muscles, the biceps, the triceps, the hip flexors. Those are the common muscles that we see and test for that would indicate a polymyositis distribution. What do we do for work-up? Well, the first thing we have to do is prove that the subacute onset proximal weakness condition is coming from inflammation in the muscle and we test the CK, and typically we see moderate elevations in the thousands or so. We can also test aldolase and AST more than ALT, and elevations on those are more nonspecific markers of muscle inflammation. The EMG and sometimes nerve conduction test can be helpful. We see a myopathic EMG, meaning short duration, low amplitude muscle firing. 01:58 There's not as much muscle to activate and not as much muscle is being activated. So, the duration of muscle activation is small in amplitude, the amount of muscle activation is small as well. We can also see spontaneous activity. This is times where the muscle fires on its own and this is suggestive of inflammation in the muscle or around the neuromuscular junction. 02:20 Muscle biopsy can be helpful in certain cases but is not required to make this diagnosis. And most importantly for polymyositis is we have to exclude other causes of myopathy. There can't be a rash to suggest dermatomyositis, or exposure to a myotoxic drug to suggest a toxic process like a statin drug or some other type of medication. The treatment for polymyositis is prednisone. This is an immune mediated condition and we calm the immune system down with corticosteroids and prednisone is the steroid of choice for this condition. 02:54 So let's look a little bit at the pathophysiology. What's going on in polymyositis and what do we see when we do that muscle biopsy in selected cases? Well, here we're looking at the vessel lumen, the interstitium, and the muscle, a single muscle fiber. And in polymyositis, we see that one of the drivers is the T-cell. T-cells become activated in the circulating system. 03:18 They traffic into that interstitial space and we see cytokine release. Cytokine release drives further inflammation and we see that CD8 cytotoxic T-cells are localized to the muscle membrane. Those CD8 cells expressed MHC1 and recognize individual muscle fibers through the MHC class 1 complex and this leads to necrosis or damage of the muscle. This is critical because on muscle biopsy for polymyositis, we're going to look for those CD8 T-cells expressing MHC1 and binding to a necrotic muscle fiber. In addition, we also see that there is other inflammation that's involved in polymyositis and increasingly we see an interplay between macrophages which are activated in the circulating system and may cross talk with B-cells which also become activated and serve an antigen presentation role contributing to this inflammation around the muscle. So, what do we see on muscle biopsy? Well, here are some of the characteristic findings. The light pink that you're seeing is the muscle. The white with the purple dots is the endomysial tissue around each muscle fiber. And what we see is too many purple dots, too many lymphocytes surrounding each of those muscle fibers. We see endomysial inflammation. Recall the makeup of the muscle. There is the big muscle body with the epimysium surrounding it, the endomysium and then individual muscle fibers with the cell membrane being the sarcolemma. And the critical finding that we see in polymyositis is endomysial inflammation, the CD8 T-cells binding to muscle fibers and resulting in necrosis and inflammation.
About the Lecture
The lecture Polymyositis by Roy Strowd, MD is from the course Acquired Neuromuscular Diseases.
Included Quiz Questions
What will a muscle biopsy show from a patient suffering from polymyositis?
- Endomysial inflammation
- Perimysial and perivascular inflammation
- Intramuscular vacuoles
- Fatty replacement
- Normal findings
Which of the following cell types would be seen in a muscle biopsy from polymyositis?
- CD8+ T cells
- CD4+ T cells
- Eosinophils
- Neutrophils
- B lymphocytes
What is the most important part of diagnosing polymyositis?
- Excluding other causes of myopathy
- Muscle biopsy
- Measuring CK
- Obtaining an EMG
- Examination of reflexes
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Miophaties is a very complicated matter, this exposition is really simple in this complicated disease. thank you Dr Strowd.