Playlist
Show Playlist
Hide Playlist
Polyarteritis Nodosa, Antineutrophil Cytoplasmic Antibody (ANCA) and Microscopic Polyangiitis
-
Slides Vasculitis Mitchell.pdf
-
Reference List Pathology.pdf
-
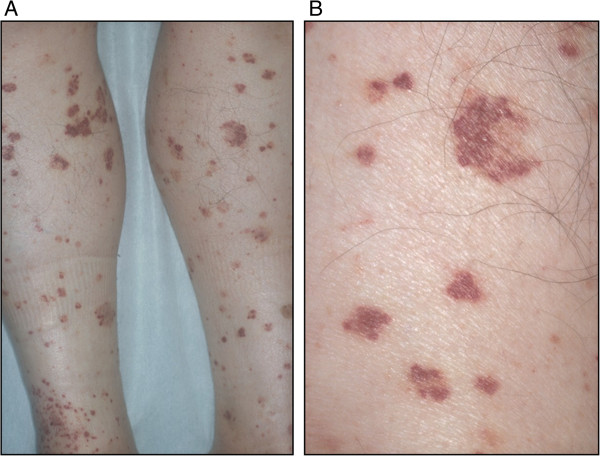
Download Lecture Overview
00:01 Okay, so now we're going to talk a little bit more about the immune complex vasculitis. 00:07 The the specific ones. 00:09 So, Polyarteritis Nodosa. 00:12 The epidemiology is that there's a peak incidence, kind of in the middle years of 45-65. 00:19 It's much more common in men than in women. 00:22 Again, the etiology is unknown, but it's due to immune complex deposition. 00:27 Typically, where you get deposition the immune complexes is that branch points of the vessel. 00:32 So that's where we have kind of turbulent flow so that kind of makes some sense. 00:36 And the inflammatory process weakens the arterial wall leading to thrombosis. 00:41 That then leads to ulcerations, infarcts, ischemic atrophy, and hemorrhage. 00:48 Signs and symptoms of polyarteritis nodosa include involvement of the renal artery in which case you will get hypertension because we are reducing flow through the renal artery or the renal arterioles. 01:02 The glomerulus senses that there's diminished flow, that diminished flow leads to elaboration of renin, which will then cleave angiotensinogen to angiotensin as we've learned previously, and we're often running in terms of driving hypertension. 01:17 Renal artery involvement in polyarteritis nodosa is very common. 01:21 So hypertension, acute onset hypertension is very common as well. 01:26 Coronary involvement occurs in about a third of cases. 01:29 And clearly the same mechanisms that are involving the renal artery and the injury and thrombosis can lead to an increased risk of myocardial infarction. 01:39 Skin involvement. 01:41 Occurs in just a little under half of patients with rash, ulcerations and nodules, and then you can have a number of gastrointestinal lesions. 01:49 Basically, wherever the immune complexes are depositing, that's where you're going to get symptomatology. 01:56 And because nerves are vascularized structures as well, you can have neuritis, you can have inflammation of the nerves, and you can have particularly of the motor nerves. 02:08 Okay, so that's polyarteritis nodosa, that's kind of a small and medium sized arteries of immune complex deposition. 02:15 Let's look at smaller vessel vasculitis. 02:19 So we're going to look at the microscopic polyangiitis, Wegener's Granulomatosis, and Churg-Strauss Syndrome. 02:27 These are going to be due to antineutrophil cytoplasmic antibodies. 02:30 Oh, remember those. 02:32 Okay, so if you think vasculitis overall is relatively rare, this is really really rare. 02:38 Still, it's a very interesting mechanism of disease. 02:41 And if we don't find clear cut immune complex deposition, we typically invoke antineutrophil cytoplasmic antibody. 02:49 This is also called Pauci-immune complex vasculitis, meaning that there really aren't immune complexes. 02:55 Okay so, the antibodies are directed against neutrophil primary granules that include the proteins proteinase 3 and myeloperoxidase. 03:05 It turns out similar structures are present on monocyte lysosomes. 03:10 So they can also be similarly activated. 03:13 And those granule contents, once they're extruded by neutrophils can settle onto endothelial cells. 03:20 You can have antibodies that are directed against endothelial cells that had been coated with proteinase 3 or myeloperoxidase. 03:30 We won't necessarily see antibodies present in the vascular lesions in the vasculitis. 03:36 But if we see elevated levels of antineutrophil cytoplasmic antibodies, those are considered very useful diagnostic markers. 03:45 So, depending on whether the antibodies are primarily against proteinase 3 or primarily against myeloperoxidase, we have different disease entities. 03:56 So if you have antibodies against proteinase 3 that disease entity is usually polyangiitis. 04:04 On the other hand, if you have anti-myeloperoxidase antibodies, that's usually associated with Churg-Strauss Syndrome but can also be with Microscopic Polyangiitis and Granulomatosis. 04:17 Let's look at some of the epidemiology of this disease. 04:20 So basically, we don't know what drives this. 04:22 We don't understand why people develop antibodies against neutrophil cytoplasmic antigens, but they do. 04:31 It's often present in older age groups, 6th and 7th decade. 04:36 It will affect men and women equally. 04:39 It's much more common in the white Anglo-Saxon population for reasons that are not yet known. 04:45 And unlike polyarteritis nodosa, in Microscopic Polyangiitis due to ANCAs, the lesions tend to all be of the same age in any given patient. 04:56 They're distributed much more broadly. 04:58 In polyarteritis nodosa, you can have lesions of various different ages, and they tend to crop up in one location and then in another location in another location. 05:11 So Microscopic Polyangiitis associated with antibodies to myeloperoxidase can be elicited not in all cases, but can be elicited by administration of certain drugs such as penicillin can also happen following infection. 05:27 It can also happen with the presentation of a variety of protein therapies. 05:36 When we see it in the kidney, and this is showing you a glomerulus from a patient with Microscopic Polyangiitis. 05:42 We can see what is a Crescentic glomerulonephritis. 05:46 So the glomerulus, what's left of it is that little shrunken hyper pink tuft in the middle and surrounding it is an epithelial cell proliferation. 05:55 So this is a very aggressive, glomerulosclerosis with Crescentic development. 06:07 Signs and symptoms very again, nonspecific, fever, malaise, fatigue, weight loss. 06:14 Patients because of the involvement of the pulmonary vascular bed can have hemoptysis not a common feature but can occur because of the involvement of the renal vascular bed can have hematuria. 06:26 There can also because of the glomerular damage be proteinuria.
About the Lecture
The lecture Polyarteritis Nodosa, Antineutrophil Cytoplasmic Antibody (ANCA) and Microscopic Polyangiitis by Richard Mitchell, MD, PhD is from the course Vasculitis.
Included Quiz Questions
Which artery is affected in 60% of patients with polyarteritis nodosa?
- Renal artery
- Pulmonary artery
- Hepatic artery
- Carotid artery
- Femoral artery
What is the peak age of incidence of polyarteritis nodosa?
- 45–65 years old
- 35–65 years old
- 45–75 years old
- 45–55 years old
- 35–55 years old
What is the most frequent neurologic complication of polyarteritis nodosa?
- Motor neuropathy
- Autonomic neuropathy
- Sensory neuropathy
- Cranial neuropathy
- Diabetic neuropathy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |