Playlist
Show Playlist
Hide Playlist
Physical Exam Findings in Cirrhosis
-
Reference List Physical Examination.pdf
-
Download Lecture Overview
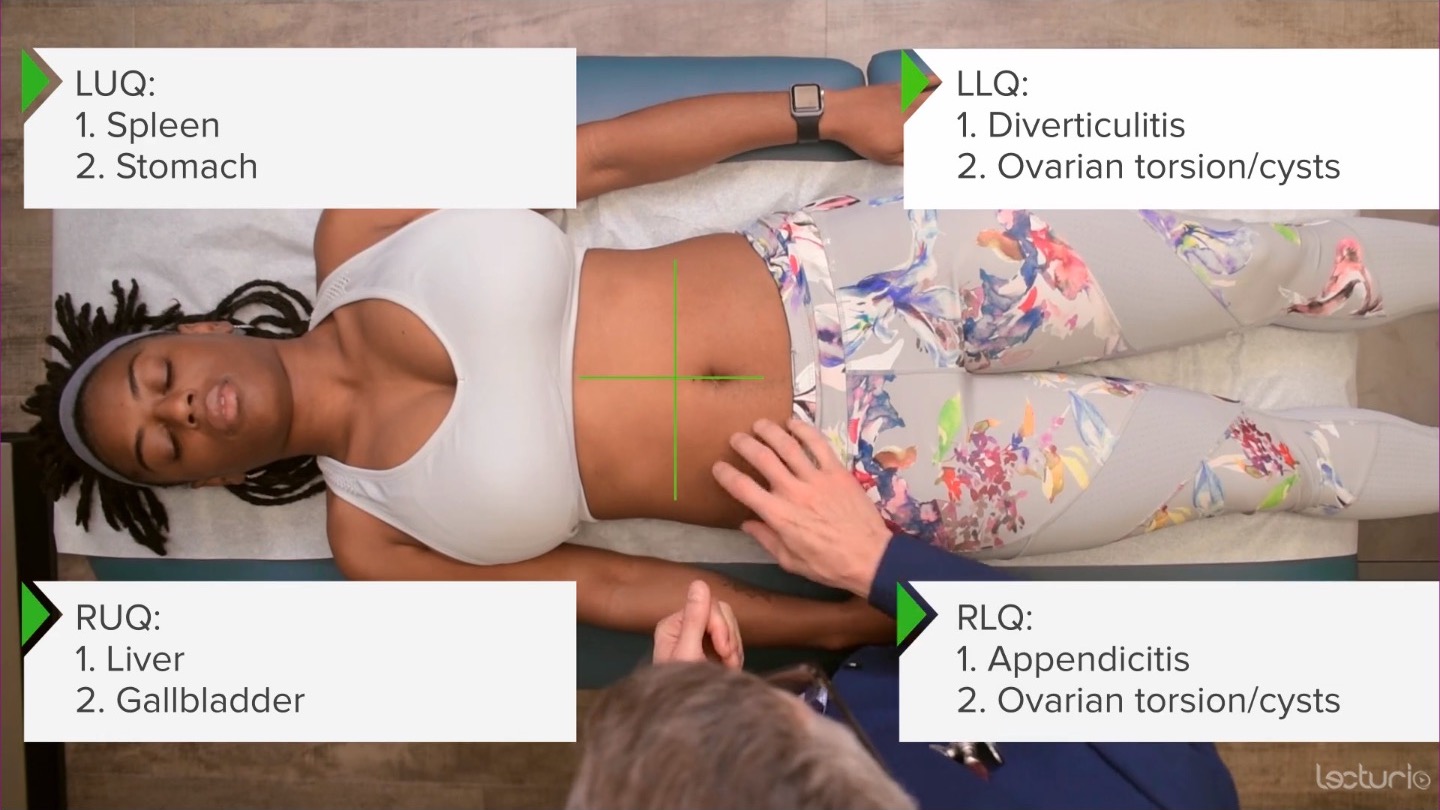
00:00 Now, let's talk about ascites. 00:01 It's really important to be able to identify ascites especially in folks who have chronic liver disease because the presence of ascites in a person who has chronic liver disease and has a little bit of abdominal pain may be concerning for SBP, Spontaneous Bacterial Peritonitis, which can be a potentially devastating condition if not detected and if you don't do an abdominal paracentesis to look for it. 00:25 So very important for us to be able to assess this at the bedside, because you can't always get an ultrasound up there quickly to do that. 00:32 So we're going to review a couple of tests for ascites. 00:35 First off, again, the person should have chronic liver disease, you're not really worried about spontaneous bacterial peritonitis and somebody without that, though, ascites can be caused by a variety of other things other than liver disease, for example, patients with metastatic ovarian cancer could have ascites as well. 00:52 In general, folks with ascites from liver disease are going to have peripheral edema. 00:56 So that can be an important marker that would suggest the presence of ascites, if there is distension, in the belly, again, those bulging flanks we were talking about earlier. 01:04 in the absence of peripheral edema, it's somewhat less likely to be ascites in the abdomen. 01:10 But now let's look at some specific findings in the belly. 01:14 So first off, we talked before about how as you move towards the back, you're going to have dullness because the retroperitoneal organs are all dull. So down here, -can you just slide your arm over; thanks- it's going to be more dullness back here compared with up here, right? In patients who have a lot of fluid in the belly from ascites the water is heavier than the intestines, so, it basically forms a pool of water all the way across the abdomen, with the intestines rising to the top. 01:48 So you'd have only tympany in this upper area, this upper circle and a line of dullness heading towards the flanks. 01:58 As opposed to in this case, you've got some tympany here, a little bit dullness there, some tympany there, there's not like a clear line, distinguishing between air and liquid. 02:09 Instead, there's just this kind of vague line where the intestines and the retroperitoneal organs begin. 02:17 So, flank dullness, when we talk about flank dullness as a sign of ascites, we're talking about a line of dullness. 02:26 Next up, we want to see if that line moves when you move the body because if it is actually like a balloon filled with water, as we rotate the balloon, the line of water should stay in the same place even as the balloon itself is rotating. 02:40 So, if I may just make a little mark. 02:44 Let's say that she did have a line of dullness here. 02:50 She doesn't, but I'm going to make a mark. 02:51 She has a line of dullness right there. 02:54 As I rotate her on to your left hip, please. 02:58 You could rotate on to your left hip. 03:00 - Okay. This way? - Yes. 03:05 After a minute or so of that fluid settling, it'll now be settled down to the left side of her abdomen. 03:13 And that line of dullness is very simple gravity working on water will now rise up, because now we have that lake of fluid is on the lower half of the dependent position that she's in. 03:25 So, I would instead find that if I started percussing, I would find dullness down here, I would put a new mark, let's say here. 03:38 Now, you can roll back over towards me. 03:41 When you have so-called shifting dullness, that is that line moved medially, that is a strong likelihood of having ascites. 03:52 And the last test we would look for ascites is called the fluid wave. 03:55 This oftentimes requires another person to come and help you do the test. 03:59 But it's based on the idea that if there's a leak of fluid in there and I push on one side, I should feel a wave of fluid hit my fingers on the other side. 04:06 So it's simply applying pressure from here, I've got my right hand here as a detector. 04:12 And I'm pushing like that. 04:14 And I'm not looking for just soft tissue kind of moving over, I'm looking for really that feeling of water having a wave that comes into your hand. 04:23 So that's called the fluid wave. 04:25 And folks who have a lot of adiposity, it's useful to have a third person sort of put their hand on the top here to prevent the soft tissue from confusing things. 04:33 But in a thin patient, it's easy enough to just do that. 04:36 And in this case, I'm not feeling any evidence of any fluid wave coming against my fingers. 04:40 So, those are all useful tests at the bedside to look for ascites. 04:45 Now, let's move on to talk about cirrhosis itself. 04:48 There are dozens of different interesting findings that can come along with cirrhosis, so called the stigmata of cirrhosis. 04:57 There's some that are diagnostically useful and some that are just historical interesting. 05:00 We're going to focus on the first group now. 05:04 We've already talked about the presence of Ascites. 05:06 That would of course support the diagnosis of cirrhosis as would Peripheral edema. 05:10 Other potential findings, we'll start head to toe. 05:13 So patients with cirrhosis oftentimes have Spider angiomata. 05:17 These are a little spider shaped, dilated capillaries that are oftentimes on the chest, sometimes on the cheeks, and certainly the upper arms. 05:27 You tend to not see them much farther down. 05:28 I mean characteristic feature is that if you push on one, and release your finger, you'll see it fill from the inside out. 05:35 So, it'll blanch and then it'll fill from the inside out, and there'll be scattered on the chest. 05:40 So the next finding would be Gynecomastia. 05:42 Now, in a woman that's going to be impossible to distinguish between actually just breasts that are present versus gynecomastia. 05:48 Whereas in men, men who have cirrhosis have excess estrogen levels, which contribute to a lot of these findings. 05:58 There's also a diminished clearance of progesterone, or metabolism of progesterone and all these things contribute to some of these manifestations. 06:06 And in men, you'll have what's called gynecomastia, which is the production of glandular breast tissue around the nipples around the areola. 06:14 And you can distinguish that from obesity. 06:16 Patients who are obese may have enlarged breasts, but there won't actually be any glandular tissue, any that indurated thick and firm tissue around the areola. 06:26 Whereas, in gynecomastia from cirrhosis, there's actual breast tissue there. 06:30 There are glands, glandular tissue around the areola, so that's a distinguishing characteristic. 06:38 Next up is the so-called Caput medusae sign. 06:41 Folks who have portal hypertension specifically in the setting of progressed or advanced cirrhosis, are going to have dilated umbilical veins, and it's called caput medusae because of this sort of looks like little spiders, or a little snakes coming off of the head of Medusa, due to this engorgement of these umbilical vessels. 07:01 It's normal to have umbilical vessels, of course. 07:04 Those are the veins that are draining your abdominal wall, but in the setting of cirrhosis with portal hypertension, fluid can't go forward pass the liver into the IVC. 07:14 So it finds other ways to end up getting back towards the heart. 07:18 So, you'd see this dilation of the umbilical vessels. 07:21 Next up, let's head towards the extremities. 07:24 Patients with cirrhosis, oftentimes will have what's called Terry's nails, where 80% of the nail plate is has turned white or leukonychia is present. 07:35 And the distal nail bed is kind of a reddish brown. 07:40 So, it's 80% white versus 20% are reddish brown in coloration. 07:46 And that's present in a number of folks with cirrhosis. 07:50 And while this is not exactly a marker of cirrhosis itself, it's a diagnosis of one of the complications of cirrhosis portosystemic encephalopathy, and that's asterixis, which is something we look for all the time and folks when we're concerned about uremic encephalopathy or portosystemic encephalopathy. 08:06 So what I'm going to have you do now, Shayla is just put your hands up in front of you, like this, like you're stopping traffic. 08:13 Patients with asterixis will develop what's called a liver flap. 08:16 We're just have your hand kind of floppy that for me. 08:19 That's a classic picture of asterixis. 08:21 You can put your hands down now. 08:23 You can actually do that in any muscle group in the body, where the patient has to maintain muscular contraction. 08:29 In some ways, it's the opposite of myoclonus. 08:31 Myoclonus is a patient at rest with spontaneous muscle contractions. 08:35 Asterixis is a patient actively contracting muscles and spontaneously losing tone in those muscle groups. 08:42 And you can even have a person stick out their tongue and look for asterixis. 08:45 It's any muscle group will work. 08:50 In addition on the hands, patients with cirrhosis may have Palmer erythema. 08:54 This is again has to do with the estrogenization and folks with cirrhosis where in particular on the thenar and hypothenar eminence you may see some blanching erythema on those areas. 09:06 Patients with cirrhosis may have Scleral icterus depending upon what's going on with their liver at the time. 09:12 Some with certainly alcohol induced hepatitis could have an acutely elevated bilirubin that would be manifest in their sclera, if they have a bilirubin of at least 3 or 4 milligrams per deciliter. 09:28 You may also see icterus even under the tongue in patients with jaundice.
About the Lecture
The lecture Physical Exam Findings in Cirrhosis by Stephen Holt, MD, MS is from the course Examination of the Abdominal Region.
Included Quiz Questions
Which physical examination findings are consistent with ascites?
- Shifting dullness and fluid wave
- Tenderness in the right lower quadrant
- Obesity
- Sister Mary Joseph node
- Purple striae
Why is shifting dullness on exam consistent with ascitic fluid in the abdomen?
- Fluid is heavier than air and thus shifts with gravity when the patient changes position.
- The liver is dull to percussion and moves with position change.
- Air is heavier than fluid, so dullness is found in the anterior abdomen.
- Fluid is dull to percussion and shifts to the top of the abdomen with ascites.
- Ascitic fluid is not able to be assessed by percussion of the abdomen.
Cirrhosis of the liver can produce which of the following physical exam findings?
- Ascites, gynecomastia, and spider angiomas
- Ascites, Sister Mary Joseph node, and Beau's lines in the nails
- Gynecomastia, conjunctivitis, and intention tremor
- Asterixis, facial erythema, and wheezing
- Spider angiomas, dermatitis, and deep vein thrombosis
Why is gynecomastia seen in men with cirrhosis?
- Glandular breast tissue is produced due to excess estrogen.
- Glandular breast tissue is produced due to increased testosterone levels.
- Cirrhosis causes obesity and patients have breast enlargement.
- Cirrhosis causes shifting in body fat.
- Cirrhosis causes fluid retention and the breasts appear larger.
On which areas of the body would you find spider angiomas in a patient with cirrhosis?
- Chest, cheeks, and arms
- Lower back and legs
- Hands and feet
- Genitalia
- Abdomen and legs
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text