Playlist
Show Playlist
Hide Playlist
Pheochromocytoma – Secondary Hypertension
-
Slides Secondary Hypertension.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
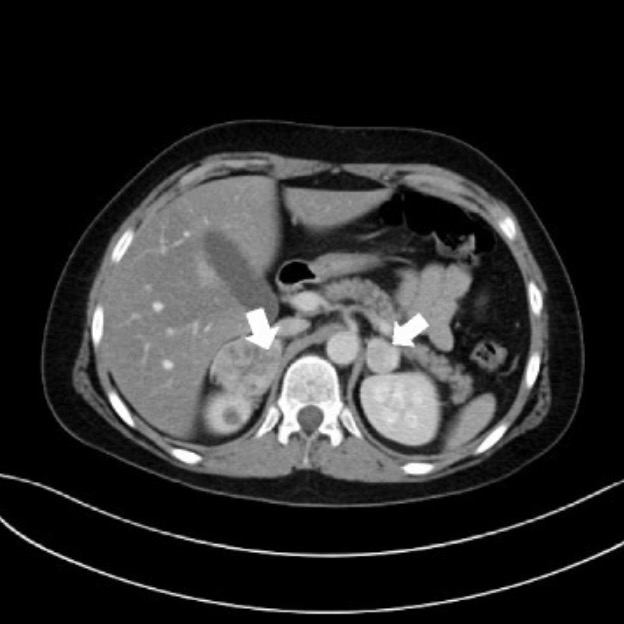
00:01 So, we're talking about pheochromocytoma. 00:03 I think this is probably something that we've all learned about but hardly any of us see but it's exciting, nevertheless, when you do see it clinically and you should be aware of what it looks like so you can urgently treat these patients as they need this. 00:16 Pheochromocytoma are catecholamine-secreting tumors that arise from the chromaffin cells of the adrenal medulla and sympathetic ganglia. 00:24 Patients clinically typically will present with this classical triad in addition to hypertension. 00:31 They have episodic headache, diaphoresis or sweating, tachycardia, sometimes they explain this impending sense of doom. 00:38 Now, I want you to keep in mind that 40% of the population or 40% of tumors are going to be part of a familial disorder including multiple endocrine neoplasia type 2 or MEN2, von Hippel-Lindau syndrome, and neurofibromatosis type 1. 00:54 So, getting a family history is going to be critical in that patient population. 00:58 So, once we suspect pheochromocytoma, our next step in diagnosis is to do a 24-hour fractionated urinary metanephrines and catecholamines. 01:09 What we're looking for is norepinephrine, epinephrine, dopamine, and normetanephrines. 01:13 Now, this has a very high sensitivity and specificity, about 98% respectively. 01:19 We can also do something like a fractionated plasma metanephrines. 01:23 It has a very high sensitivity between 96 and 100% but specificity is quite a bit lower because there's a lot of false positives here. 01:33 It's much more attractive to patients because it doesn't require a 24-hour urine. 01:37 It's something that you can just get a plasma level from. 01:40 But really, you should only use this first-line when your pre-test probability is high. 01:44 So, I might reserve this for somebody who has classical symptoms and a familial history like MEN2. 01:51 Alright, once we've got biochemical confirmation, remember, we have to locate where this tumor is so we want to do either a CT or MRI of the abdomen and pelvis. 02:03 This allows us to detect almost all sporadic tumors cuz most are about 3 cm or larger in diameter. 02:09 The sensitivity is quite high at 98-100% but only 70% specific, again, this is because of that prevalence of adrenal incidentalomas. 02:20 That means there's an adrenal tumor there that's nonfunctional. 02:23 We've talked about those before in our other cases. 02:26 Now, if for some reason, we don't have any luck with our CT or MRI imaging, we can go to our radionuclear testing with an MIBG scintigraphy. 02:36 This is performed, again, if we have a CT that's negative and/or an MRI that's negative but we have biochemical confirmations so we know that a pheochromocytoma is there. 02:46 This particular test can also detect multiple tumors so if a patient has multiple tumors up the sympathetic ganglia, we can see that. 02:54 And the radioisotope is essentially of norepinephrine so it's a norepinephrine analog. 02:59 Okay, so once our patient manifest, we have biochemical confirmation, we now have location of where the tumor is. What do we want to do? Before we do anything, we've got to control that blood pressure. 03:14 These patients have some of the highest blood pressures and they really can succumb to that and have complications. 03:19 So, we want to get an alpha antagonist on board and before we even think about surgical resection, that blood pressure needs to be controlled as best as we can do that. 03:28 So, we're gonna use something like phenoxybenzamine which is a long-acting nonspecific alpha-blocking agent. 03:34 We typically start that about 7-10 days prior to surgical resection. 03:38 We can also use phentolamine which is a shorter-acting nonspecific alpha-blocking agent as well. 03:44 Now, we can use beta blockers because remember, these patients are extraordinarily tachycardic but we only want to use these after adequate alpha blockade is achieved. Okay? If we start beta blockers before we have alpha blockade, we have unopposed alpha stimulation and those patients can get extraordinarily hypertensive. 04:05 So, please remember, long-acting alpha antagonist first followed by beta blockade. 04:11 Now, if additional agents are needed, the use of dihydropyridine calcium channel blockers can be used. 04:18 Things like nifedipine or amlodipine. 04:20 Now, we now -- once our blood pressure is fairly well-controlled, we wanna get our endocrine surgeon or surgical colleague to come in and remove the tumor. 04:31 One thing that I do want you to be aware of is that patients can undergo acute hypertensive crisis when you are in the process of surgically resecting this tumor. 04:40 This can occur because of endotracheal intubation with anesthesia induction or just manipulating that adrenal gland. 04:46 So, during the operative procedure, it's important to control that blood pressure, those patients should be treated with parenteral nitroprusside, phentolamine, or nicardipine.
About the Lecture
The lecture Pheochromocytoma – Secondary Hypertension by Amy Sussman, MD is from the course Secondary Hypertension.
Included Quiz Questions
Which of the following familial syndromes is associated with pheochromocytoma?
- Multiple endocrine neoplasia type 2 (MEN2)
- Neurofibromatosis type 2
- Multiple endocrine neoplasia type 1 (MEN1)
- Tuberous sclerosis
Which of the following statements is true regarding pheochromocytoma?
- Starting a beta-blocker before adequate alpha blockade can lead to a further elevation in blood pressure.
- Nitroprusside is the preferred drug for preoperative blood pressure control in patients with pheochromocytoma.
- MIBG scintigraphy should be performed when CT or MRI findings are negative after a negative biochemical test result.
- A fractionated plasma metanephrine test has the highest sensitivity and specificity among the biochemical tests used in pheochromocytoma.
Which of the following best describes a pheochromocytoma?
- A catecholamine-secreting tumor arising from chromaffin cells from the adrenal medulla and the sympathetic ganglia.
- A neuroendocrine tumor arising from primitive cells of the gut and lung.
- A vasoactive intestinal peptide-secreting tumor that typically arises from pancreatic islet cells.
- An insulin-secreting tumor arising from the ductular/acinar system of the pancreas.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |