Playlist
Show Playlist
Hide Playlist
Pheochromocytoma
-
Slides 01-02-02 Adrenal Pituitary.pdf
-
Reference List Endocrinology.pdf
-
Reference List Adrenal Gland Disorders.pdf
-
Download Lecture Overview
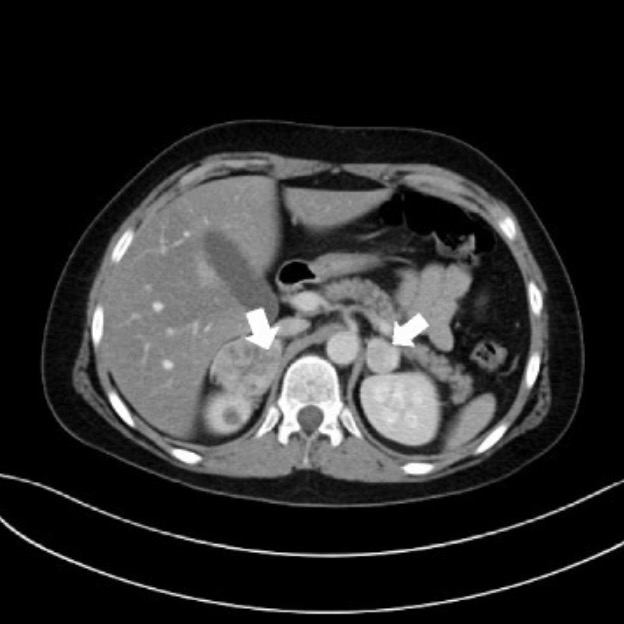
00:00 Paragangliomas are tumors composed of chromaffin cells. 00:05 80% of Intra-adrenal pheochromocytomas are paragangliomas. 00:10 Pheochromocytoma and extra-adrenal sympathetic paragangliomas almost always secrete catecholamines. 00:17 These include norepinephrine, epinephrine, and dopamine. 00:22 Although catecholamine-secreting tumors are rare overall, they are found in 0.5% of patients with hypertension. 00:31 Pheochromocytomas account for 5% of adrenal incidentalomas. 00:37 An incidentaloma is a radiographic term for a mass incidentally found on imaging. 00:43 Most pheochromocytomas secrete norepinephrine resulting in episodic or sustained hypertension as was present in our case. 00:52 Orthostatic hypotension can also be seen and likely reflects low plasma volume. 00:57 Symptoms as described include palpitations, tremor, pallor, and anxiety. 01:03 Less commonly, these patients can present with papilledema, diabetes mellitus, and cardiomyopathy. 01:09 Most of these manifestations are from elevated levels of blood pressure. 01:13 Approximately, 10% of pheochromocytomas and 20 to 50% of paragangliomas are malignant. 01:21 Pheochromocytomas are seen with multiple endocrine neoplasia syndromes. 01:27 Type 2A and 2B MEN syndromes include neurofibromatosis type 1 and Von Hippel-Lindau syndrome. 01:35 Let’s review some of the multiple endocrine neoplasia syndromes. 01:40 MEN 1 is caused by the inheritance of one mutated allele with a somatic mutation in other allele and leads to neoplasias. 01:48 The most common presentation is with a parathyroid adenoma, often multiple. 01:53 To confirm the diagnosis of MEN 1, this must be associated with pancreatic islet cell tumors or enteric tumors like a gastrinoma or an insulinoma. 02:04 Pituitary adenomas may also occur. 02:07 Other associations include carcinoid tumors and adrenocortical adenomas. 02:12 MEN 2A most commonly manifests with medullary thyroid carcinoma in association with a pheochromocytoma which is often multifocal as well as parathyroid hyperplasia. 02:24 MEN 2B manifests with medullary thyroid carcinoma. 02:29 But here, although also associated with pheochromocytomas is also accompanied by mucosal neuromas, gastrointestinal ganglioneuromas, and patients may have a Marfanoid body habitus. 02:42 Returning now to confirming the diagnosis of pheochromocytoma, the excessive secretion of catecholamines or their metabolites as measured in the plasma or urine will help. 02:53 Evaluation is recommended for all incidentally noted adrenal masses or in the setting of hereditary pheochromocytoma or paraganglioma syndromes. 03:04 The sensitivity of plasma free metanephrines is the highest of any screening test in endocrinology at 96-100%. 03:12 However, the specificity is relatively low at 85-89%. 03:17 Bear in mind that the pretest probability based on the patient’s presentation in terms of signs and symptoms can improve this. 03:26 Plasma free metanephrines will reliably exclude a pheochromocytoma when negative. 03:32 But further testing is needed to confirm the diagnosis unless the result is markedly abnormal, often in the range of four times the upper limits of normal. 03:43 Imaging follows the biochemical diagnosis for radiographic localization. 03:49 Because most catecholamine-secreting tumors are located in the abdomen, a CT or MRI of the abdomen is the best place to start. 03:58 If negative, an Iodine-123 MIBG scan can be performed. 04:04 Adjunctive diagnostic tests are MRI of the chest and the neck region if you have not identified the tumors within the abdomen. 04:17 Laparoscopic adrenalectomy is the preferred treatment for pheochromocytoma except in the case of a large or malignant tumor where an open adrenalectomy is required. 04:28 Long-term follow up is needed for pheochromocytoma and paragangliomas due to difficulty distinguishing benign from malignant tumors. 04:37 Metastases have been reported after 20 years of the diagnosis. 04:42 In addition to routine clinical surveillance, annual measurements of plasma or urine metanephrines is indicated to assess for a current or metastatic disease. 04:53 Metastatic disease is managed with additional surgery and MIBG therapy as well as chemotherapy and/or radiotherapy.
About the Lecture
The lecture Pheochromocytoma by Michael Lazarus, MD is from the course Adrenal Gland Disorders. It contains the following chapters:
- Pheochromocytoma
- Review of MEN
Included Quiz Questions
Which of the following is a common presenting symptom of pheochromocytoma?
- Tremor
- Bradycardia
- Skin flushing
- Papilledema
- Episodic hypotension
Which of the following syndromes is NOT associated with pheochromocytoma?
- MEN 1
- MEN 2B
- Von Hippel–Lindau syndrome
- Neurofibromatosis type 1
- MEN 2A
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |