Playlist
Show Playlist
Hide Playlist
Peripheral Neuropathy: Approach According to Its Location
-
Slides Introduction to Neuropathy Disorders.pdf
-
Download Lecture Overview
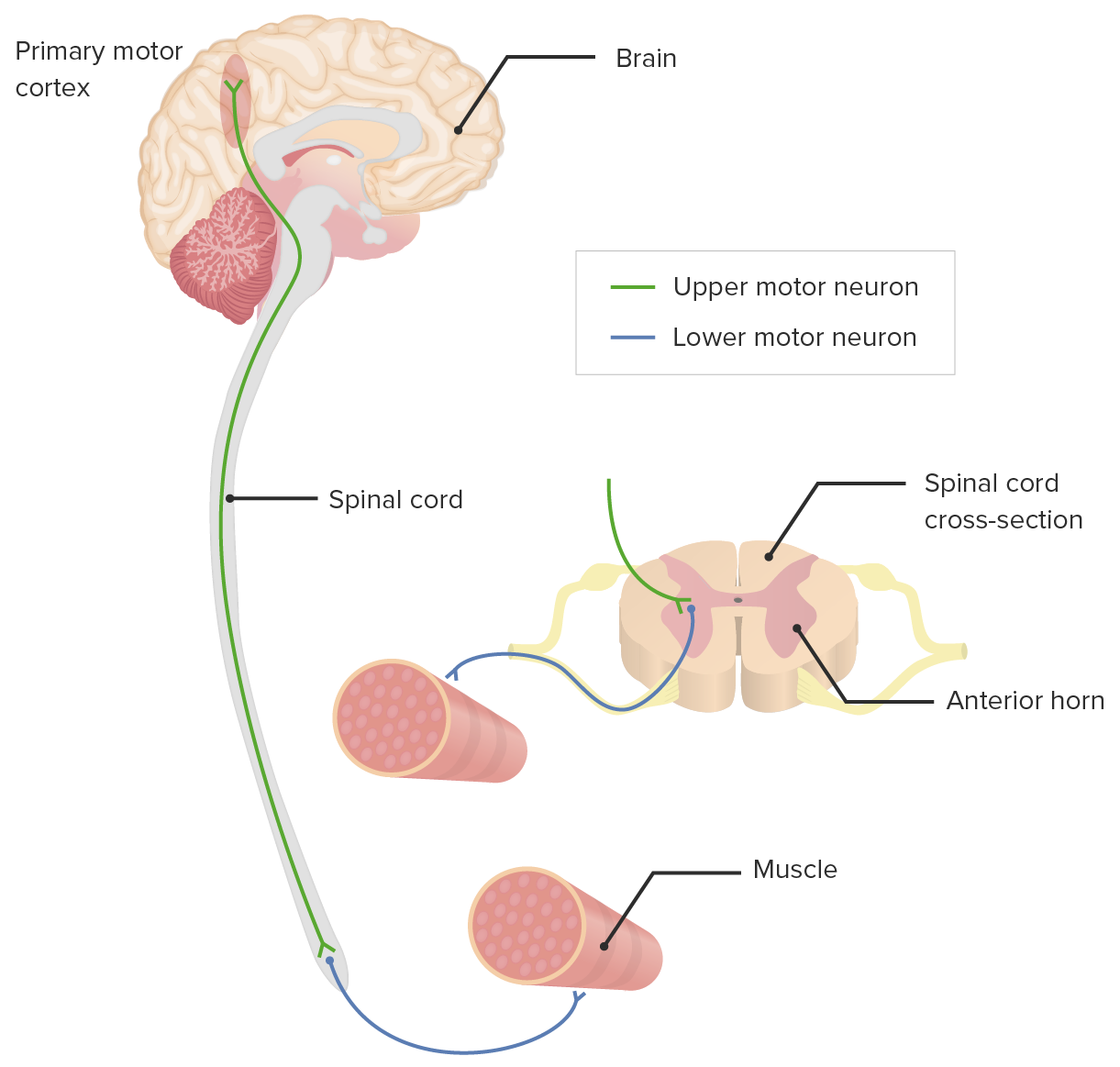
00:00 So, when we think about matching the patient presentation to the type of nerve that's involved, we can look at the symptoms and map that to our understanding of peripheral nerve anatomy. 00:11 When patients present with reduced vibration and proprioception, we think about large fiber involvement and disorders that affect the large fiber nerves. 00:19 When patients report pain, temperature, paresthesias, and neuropathic pain, we think about small fiber neuropathies in small fiber involvement. 00:27 And weakness points us squarely to motor involvement. 00:30 And so, this is how we use both the history and our physical exam to narrow our differential diagnosis to the type of neuropathy that we need to investigate. 00:39 So, how do we localize a neuropathy? Well, neuropathy is a peripheral nervous system disorder. 00:44 So, we're going to use all those things we know about peripheral nervous system localization to help with these patients. 00:51 We think about distribution, sensory changes in reflex findings, particularly to help localize a neuropathy. 00:58 In terms of distribution, we don't see a level. 01:00 We can see a distribution that affects multiple nerves or a single nerve, but importantly, symptoms should follow the course of the nerve. 01:08 A myotome should be affected if motor involvement is present, or a dermatome should be affected if sensory nerves are affected. 01:16 Motor weakness follows the peripheral nerve pattern. 01:19 Again, a myotomal pattern. Sensory dysfunction is common and may range from numbness to tingling paresthesias, to frank neuropathic pain. 01:28 And very, very importantly, reflexes are often reduced or can be absent. 01:33 Absence of reflexes should point strongly to a peripheral nerve neuropathic disorder. 01:40 We use sensory testing to evaluate the nerve involvement. 01:46 Sensory testing of vibration and proprioception interrogates function of the large fiber nerves and the dorsal column medial meniscus system in the central nervous system. 01:55 So, problems with vibration and proprioception should point us to large fiber neuropathies or problems affecting the dorsal column. 02:04 Similarly, sensory testing of pain and temperature interrogates function of the small fiber nerves and the anterolateral system of the spinal cord. 02:13 And so, patients reporting significant pain, neuropathic pain, paresthesias, or small fiber symptoms, those symptoms may be arising from a small fiber neuropathy or pathology affecting the anterolateral system. 02:27 When we think about strength testing, strength testing assesses motor function in addition to other areas of the nervous system, and deep tendon reflex testing assesses both the sensory nerve, afferent, and the motor nerve efferent part of that arc. 02:41 And so, reduced areflexia can be seen with our sensory neuropathies, motor neuropathies, or polyneuropathies. 02:49 The distribution of deep tendon reflex reduction or loss is very important. 02:53 Diffuse deep tendon reflex loss, particularly early in the course of a disease, suggests proximal nerve pathology like a polyradiculopathy, and distal deep tendon reflex loss suggest a distal disorder like a diabetic polyneuropathy, which is a distal symmetric length-dependent neuropathy affecting the distal deep tendon reflexes first, and approximately deep tendon reflexes over time. 03:20 So, let's look one more time at reflex testing and understand the type - the distribution of reflex abnormalities and how this can help us to narrow a differential. 03:29 When we tap on a reflex, that input is felt and sensed by peripheral sensory afferents. 03:36 The information is propagated up the sensory afferents and relays and terminates with a motor nerve in the ventral horn. 03:44 That motor information is carried out the interior rootlet to the peripheral motor nerve innervating the muscle and resulting in contraction. 03:53 So, there's two patterns of deep tendon reflex abnormalities. 03:58 The first we see with the distal symmetric polyneuropathy is like diabetes. 04:03 Their distal deep tendon reflexes are reduced and the proximal deep tendon reflexes are preserved. 04:09 That distal dying back that we see in the vast majority of distal symmetric links dependent polyneuropathies like diabetes, we find this pattern of reflex exam. 04:20 The other pattern is early proximal involvement or diffuse hypo or areflexia. 04:26 And a good example of a disorder where we see this is Guillain-Barre or acute inflammatory demyelinating polyneuropathy. 04:34 Here, diffuse areflexia is a sign of proximal involvement or a polyradiculopathy. 04:40 The immune system can affect any part of the nerve. 04:43 It can attack the distal nerve or the proximal nerve, and there's equal probability of affecting any aspect of the nerve. 04:51 So, we see early involvement, early loss of that sensory afferent distal efferent arc of the reflex exam, and early diffuse areflexia in those disorders. 05:03 So, now, let's put it all together. Let's talk about how we approach peripheral nerve pathology. 05:08 We're going to walk through the different localizations in the peripheral nervous system and talk about the motor, sensory, and reflex exams at each level. 05:17 Let's start with anterior horn cell disorders. 05:19 These are our motor neuron disorders. 05:22 On motor exam, patients have weakness and atrophy in the segment that is affected or in a focal pattern. And we commonly see fasciculations. Fasciculations are signs of peripheral motor nerve dysfunction. 05:34 Our sensory exam is intact, there's no sensory abnormalities, and reflexes are reduced to absent. 05:40 And examples of motor neuron diseases affecting the anterior horn cells are amyotrophic lateral sclerosis, or ALS, and poliomyelitis. 05:49 Moving out from the spinal cord, spinal nerve root disorders present differently. 05:55 Again, on our motor exam, we do see weakness and atrophy in a root innervated pattern. 06:01 A specific myotome is affected, or for the sensory exam, a specific dermatome. 06:06 Sometimes, we will see fasciculations in the area innervated by that nerve root, but that's uncommon. Our sensory exam corresponds to the nerve root that's involved. 06:17 So, we see a dermatomal pattern of sensory deficits. 06:20 And our reflexes may be reduced or absent in the pattern of the nerve root that's affected. 06:27 Examples include a herniated disc in the cervical or lumbar region. 06:31 Moving out even more distally, pathology at the peripheral nerve, and specifically the motor nerve or a motor neuronopathy. 06:39 This looks a lot like motor neuron diseases. 06:42 Motor neuronopathy is present with weakness and atrophy that fit a peripheral nerve distribution, and often or sometimes with fasciculations. 06:51 Sensory nerve loss is minimal in motor neuronopathies. 06:55 We should not see sensory findings and reflexes may be reduced or absent, and an example may be trauma. 07:03 Moving out more distally, we can talk about peripheral nerve disorders affecting a single nerve, the mononeuropathies. A motor exam shows weakness and atrophy, and a peripheral nerve distribution following the course of that single nerve. 07:16 We can see fasciculations, but that's not common. 07:19 Sensory loss may be seen but should be in the pattern of that nerve. 07:22 Reflexes may be reduced if there is a reflex innervated by that nerve, and examples include trauma, carpal tunnel syndrome, or fibular neuropathy. 07:33 Moving out more distally, pathology affecting the peripheral nerve, but multiple nerves, a polyneuropathy, present with weakness and atrophy, and that may be more distal than proximal, and sometimes cause fasciculations in that distribution. 07:47 Sensory deficits are common and may appear in a stocking glove distribution and deep tendon reflexes may be reduced or even absent, but they'll start distally and move their way proximally Some of the peripheral polyneuropathies, diabetic polyneuropathy, alcoholism-related polyneuropathy are common examples. 08:05 And this differs from pathology affecting the neuromuscular junction. 08:09 Junctional disorders can present with weakness. 08:11 This may be proximal, it may be with - be distal, but we commonly see bulbar dysfunction, and fatigability should raise suspicion for a junctional disorder. 08:20 Our sensory exam should be intact. 08:22 Reflexes are often normal, but may be reduced, and the classic disease is myasthenia gravis. 08:28 And then, finally, muscle disorders can present with a common chief complaint, but different distribution. 08:33 Here, a weakness is usually more proximal than distal. 08:37 Most of our neuropathies will present with distal neuro - distal weakness. 08:41 For muscle disorders, sensation exam should be intact. 08:44 Reflexes are normal to reduce, and the classic example are the inflammatory muscle diseases or inherited muscle disorders like muscular dystrophies.
About the Lecture
The lecture Peripheral Neuropathy: Approach According to Its Location by Roy Strowd, MD is from the course Introduction to Neuropathy Disorders.
Included Quiz Questions
What is the most likely location of a lesion in a patient with motor fatigability, intact sensation, and normal deep tendon reflexes?
- Neuromuscular junction
- Spinal root
- Anterior horn cell
- Muscle
- Peripheral nerve
What is the most likely location of a lesion in a patient with weakness, atrophy, fasciculations, intact sensation, and decreased deep tendon reflexes?
- Anterior horn cell
- Neuromuscular junction
- Muscle
- Spinal nerve root
- Peripheral nerve
Which of the following disorders will show early onset of diffuse areflexia in both proximal and distal deep tendon reflexes?
- Guillain-Barré syndrome
- Diabetic polyneuropathy
- Myasthenia gravis
- Muscular dystrophy
- Trauma to the fibular nerve
A patient that has diabetic neuropathy is likely to have which physical findings?
- Weakness and atrophy more distal than proximal, loss of sensation in a stocking-glove pattern bilaterally, and decreased distal deep tendon reflexes
- Weakness and atrophy in a specific nerve pattern, loss of sensation in a dermatomal pattern, and decreased deep tendon reflexes
- Weakness and atrophy in a segmental pattern, no loss of sensation, and decreased deep tendon reflexes
- Fatigability more than weakness, intact sensation, and normal deep tendon reflexes
- Weakness more proximal than distal, sensation intact, and normal or decreased distal deep tendon reflexes
Which of the following is TRUE regarding pain and temperature testing?
- They assess the function of the small peripheral nerve fibers and the anterolateral central nervous system tracts.
- They assess the function of the large peripheral nerve fibers and the anterolateral central nervous system tracts.
- They assess the function of the small peripheral nerve fibers and the dorsal column central nervous system tracts.
- They assess muscular contractile function.
- They are used to primarily assess reflexes.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |