Playlist
Show Playlist
Hide Playlist
Peripheral Chemoreceptors – Control & Regulation of Breathing
-
Slides 05 PulmonaryControlRegulation RespiratorySystem.pdf
-
Download Lecture Overview
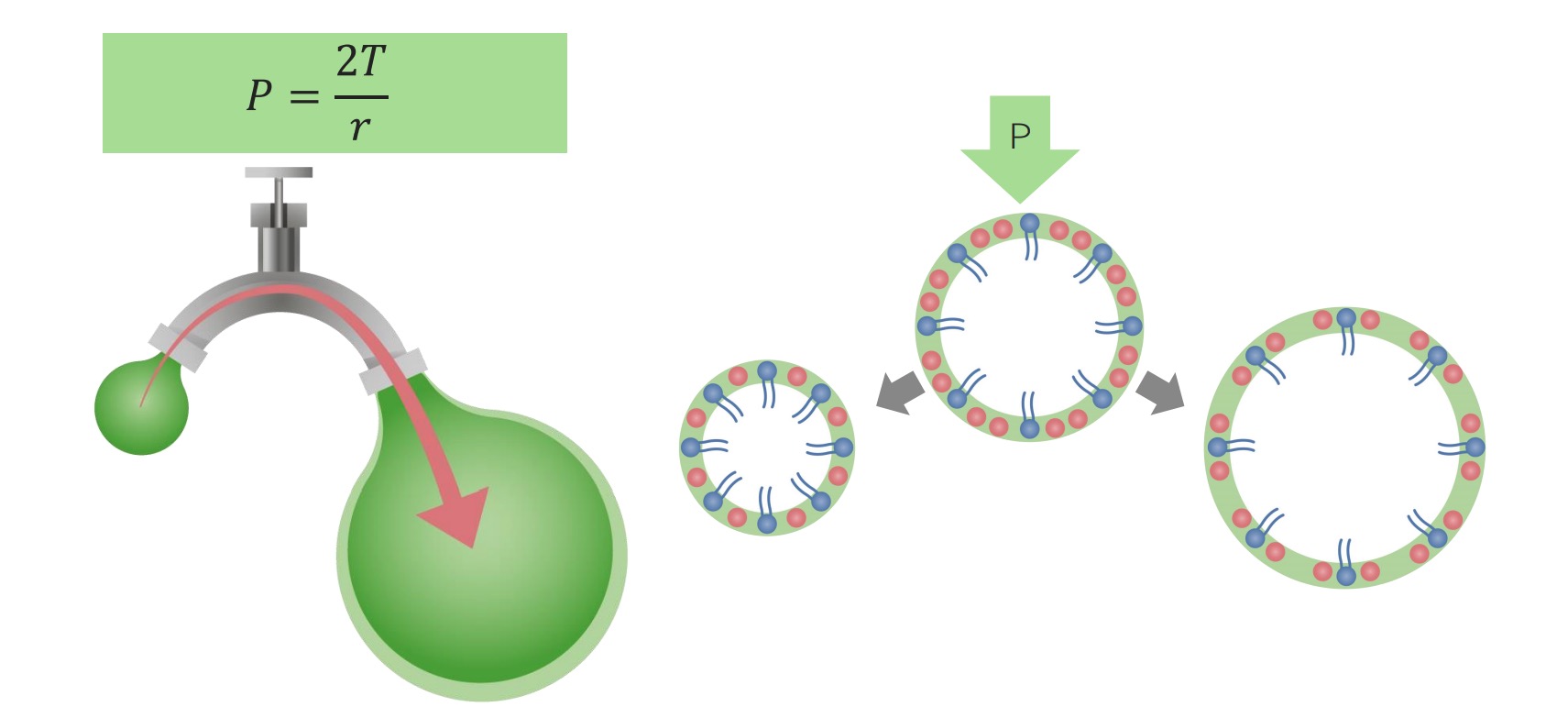
00:01 Now peripheral chemoreceptors, we talked about before they’re responsive to more blood gasses than the central chemoreceptors. 00:08 Where are they located? Well, they are primarily located in the carotid bodies and the aortic bodies. 00:18 This will help because the carotid bodies will send their information via cranial nerve IX, which is the glossopharyngeal, or cranial nerve X, which is the vagus nerve. 00:28 This is the overall anatomical process for how these particular bodies are sensed and where they send their signal to. 00:38 But now, let’s go in a little bit more detail to what these particular bodies look like and how they operate. 00:45 We can see a blowup here of a peripheral chemoreceptor. 00:50 The most important aspect of these particular chemoreceptors are these type I or glomus cells. 00:56 The glomus cells are the sensors for the various carbon dioxide oxygen and so forth. 01:04 The blood is in these little sinusoids which can be seen as the red components of circles, and in the blood vessels that go into these particular carotid bodies. 01:15 There are also other nervous system information that is both sensed as an afferent and efferent. 01:24 For example, the sympathetic nervous system has efferent signals that will send both to the glomus cells and the various components around it. 01:32 And what this can do is alter the gain of what a glomus cells would be able to signal. 01:39 What I mean by gain is a certain amount of carbon dioxide in a sympathetically stimulated environment will cause a greater response than if you had that same signal with CO2 without sympathetic stimulation. 01:55 The afferent information is again for the carotid body sensed by cranial nerve IX or the glossopharyngeal and then that’s sent up to the brain. 02:07 So peripheral chemoreceptors, these are the ones again in the carotid bodies. 02:11 They are going to be sensing particular signals in a little different manner than the central chemoreceptors. 02:18 So let’s go through that process. 02:20 You’ll notice here that there are blood vessels right next to the glomus cells. 02:26 What's very important on these type I glomus cells, there is oxygen-dependent potassium channels. 02:33 And when PO2 in those blood vessels are high, these potassium channels remain open and what this means is potassium is allowed to leak out of the glomus cell. 02:45 And if this occurs, there’s no change in membrane potential and the glomus cell is quiet. 02:53 And this can be seen in this diagram where we put all the pieces together. 02:57 Again, this oxygen-dependent potassium channel is open. 03:03 Calcium channels are closed. PO2 is high in this case. 03:11 Now when PO2 falls, those potassium channels close. 03:16 And as the potassium channel closes, the potassium which would be leaving the cell builds up within the cytosol. 03:23 That creates a positive charge and can eventually depolarize that glomus cell. 03:29 As that depolarization happens, that opens L-type calcium channels. 03:33 And calcium is allowed to rush in to the glomus cell. 03:38 What this causes is a docking and fusing of a neurotransmitter to signal sensory afferents and sending that signal up to the brain. 03:49 This whole process works in response to a fall in O2. 03:57 Now showing you how this works in terms of a diagram where we have membrane potential on the Y-axis and then we have time on the X-axis. 04:07 We have a normal resting membrane potential here. 04:10 This is time in which we have reduced the amount of O2 and you can see a dramatic increase in the firing frequency. 04:18 And what does that increase in firing frequency tell us? These spikes are all releasing neurotransmitter and sending signals back to the brain. 04:30 Now let’s talk through a little bit about how O2 and CO2 govern your drive to breathe. 04:36 And I like this kind of flow chart because it tells you a little bit more about what kind of decisions the brain stem needs to make to determine if you should breathe or not. 04:47 So if the arterial partial pressure of carbon dioxide goes up, central chemoreceptors are engaged. 04:56 The decision then will be to increase ventilation. 05:00 If arterial partial pressure of oxygen decreases, peripheral chemoreceptors will be engaged and then there needs to be another question asked. 05:12 And that is this decrease of O2 occurring at the same time that CO2 is increasing? If that’s the case, the decision will be to increase ventilation. 05:24 If the answer is no, we need to ask another question and that is is the partial pressure of oxgen less than 60 millimeters of mercury? If that answer is yes, you have to increase ventilation. 05:38 If the answer is no, it cycles back to a process in which now we’re going to govern if O2 or CO2 will change. 05:47 This kind of flow chart is very nice when thinking about when you get numbers from an arterial blood gas, trying to decide what the body is going to do with that information.
About the Lecture
The lecture Peripheral Chemoreceptors – Control & Regulation of Breathing by Thad Wilson, PhD is from the course Respiratory Physiology.
Included Quiz Questions
Which of the following types of channels are present on type-I glomus cells?
- Oxygen-dependent potassium channels
- Oxygen-dependent calcium channels
- Oxygen-dependent sodium channels
- Oxygen-dependent chloride channels
- Oxygen-dependent magnesium channels
Which of the following types of channels open after depolarization of glomus cells at low partial pressures of O2?
- L-type calcium channels
- L-type sodium channels
- L-type potassium channels
- L-type chloride channels
- T-type calcium channels
Which of the following changes will occur in the body in response to PO2 < 60 mmHg?
- Increase in ventilation
- Decrease in ventilation
- Normal breathing rate
- Relaxation of diaphragm
- Decrease in carbon-dioxide
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |