Playlist
Show Playlist
Hide Playlist
Pancreatitis in Children: Pathology
-
Slides PancreatitisCholecystitis Pediatrics.pdf
-
Download Lecture Overview
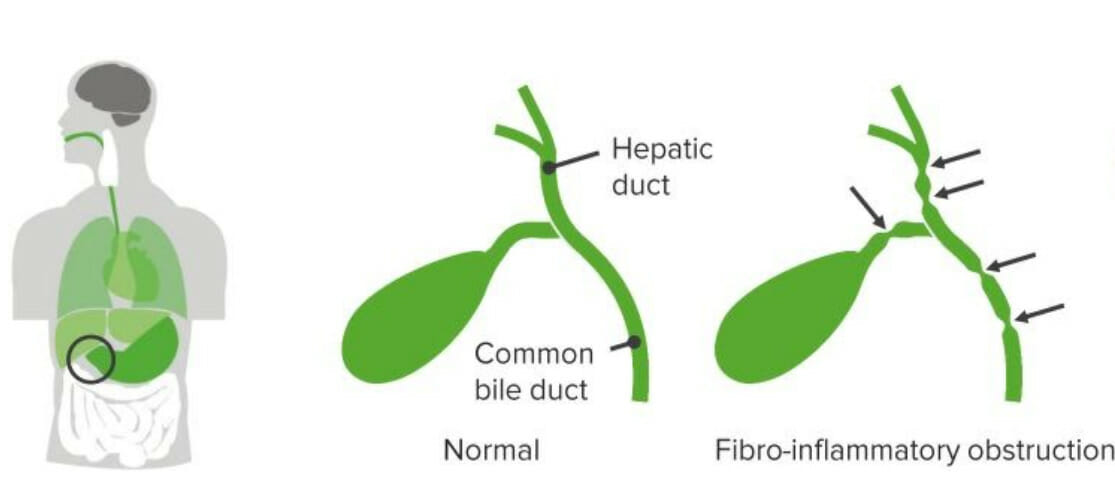
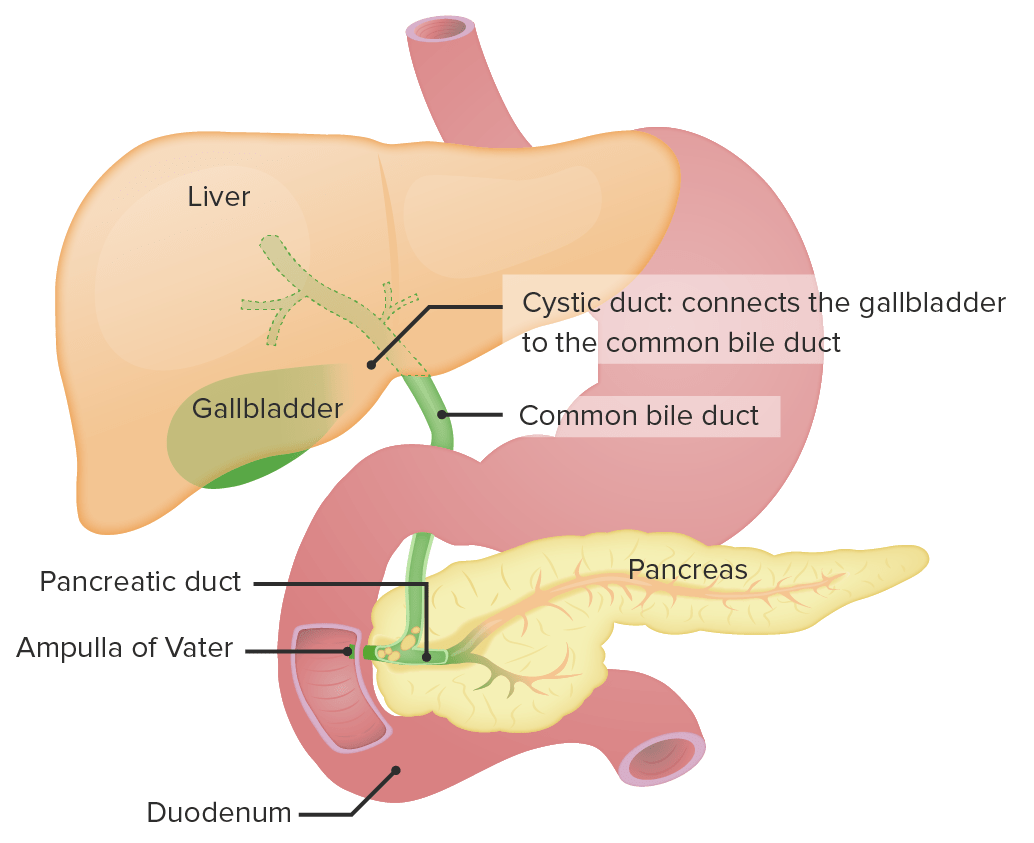
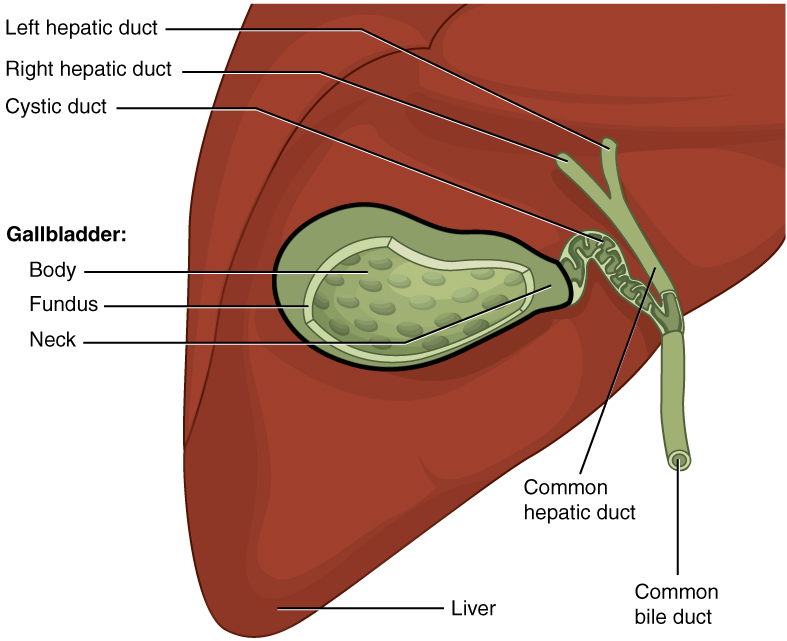
00:02 In this lecture, we’ll be discussing acute pancreatitis and cholecystitis in children. 00:09 Let’s start with pancreatitis. 00:12 So here, you have a 17-year-old male who’s coming in with abdominal pain and vomiting. 00:18 He admits to drinking alcohol with his friends after school and has been feeling nauseous and vomiting a lot, but was attributing these symptoms to his alcohol use. 00:28 On physical exam, he has abdominal tenderness, fever, and decreased bowel sounds. 00:32 You notice he has an upper abdominal pain that radiates up to his back. 00:37 He’s feeling worse after eating, maybe a half hour to an hour after eating. 00:42 And then you notice the lab work shows an elevated lipase level. 00:47 This is a classic case of pancreatitis. 00:51 Let’s look at what pathologic processes might have led to this problem. 00:57 So, pancreatitis is an acute or chronic inflammatory process of the pancreas. 01:02 Generally, in acute disease, it’s a reversible injury associated with inflammation. 01:08 In chronic disease, there is irreversible destruction from prolonged inflammation. 01:14 Keep in mind, pancreatitis is much more common in adults and children. 01:20 But likewise, children are more likely to have acute rather than chronic pancreatitis with the exception of those children with underlying significant systemic disease such as say cystic fibrosis. 01:35 Metabolic disorders and anatomic or mechanical problems can increase your risk of problems in the pancreas in children. 01:44 Examples are pancreas divisum, which is a congenital divided pancreas where there might be impairment of drainage of the pancreatic fluid. 01:56 Choledochal cyst are common in children, and we’ve talked about them in our GI lectures. 02:03 This choledochal cyst can cause a backup in some cases and a pancreatitis. 02:10 Or in some cases, patients may have a dysfunction of the Sphincter of Oddi. 02:15 Remember, that’s the sphincter that might constrict and prevent release of pancreatic juices into the intestinal vault. 02:23 So, let’s drill down into the pathophysiologic mechanisms of acute pancreatitis. 02:31 First, a patient may have duct obstruction, a gallstone, for example, that could stack in the common bile duct and prevents exocrine function of that pancreas causing a backup of pancreatic enzymes. 02:46 Or a patient may ingest a substance such as alcohol, which could cause a direct acinar cell injury so the cells of the pancreas themselves are actually being directly damaged. 02:59 Or a patient may have some defective intracellular transport of enzymes within the cell that then escape and cause damage. 03:09 All of these things will lead to an acinar cell injury, and that will result in activated enzymes, which autodigest the pancreas. 03:21 This is acute pancreatitis. 03:24 Let’s go through these three major causes one at a time, starting with duct obstruction. 03:30 The most common cause of duct obstruction is gallstones or biliary sludging. 03:36 We see this more commonly in patients with sickle cell disease. 03:39 This is because these patients have a high rate of red blood cell turnover requiring more bilirubin to be excreted, and they can get sludging in their gallbladder. 03:51 Patients with cystic fibrosis often have pancreatic problems because the chloride channel is defective and they have thicker secretions inside the pancreas. 04:01 Very rarely in children, there can be neoplasms which might obstruct flow of pancreatic fluids. 04:09 Choledochal cyst, and there are several types, can involve the pancreas. 04:14 And so, this cyst may obstruct outflow of pancreatic enzymes. 04:23 Very rare but you can see especially Ascaris lumbricoides cause obstruction of the pancreatic outflow. 04:31 And lastly, congenitally, pancreas divisum can cause it as well. 04:37 All of these causes can result in an interstitial edema within the pancreas, an impaired blood flow and an ischemia to the pancreas, which results in acinar cell injury. 04:49 Thus, the enzymes that the pancreas is producing become activated. 04:54 There is an autodigestion of the pancreas resulting in acute pancreatitis. 05:02 Patients can rarely have direct acinar cell injury that’s not from an obstruction of the pancreatic drainage system. 05:10 Examples would be alcohol or drugs, direct trauma to the pancreas, an ischemic process in the pancreas. 05:18 Viruses can rarely cause this. 05:22 Patients with diabetes because of the autoimmune process occurring in their pancreas may have impairment of exocrine function as well as endocrine function of the pancreas. 05:33 Also, hypercalcemia is associated with acute pancreatitis. 05:41 These acinar cell injuries cause release of pro-enzymes resulting in acinar cell injury that further occurs. 05:50 These enzymes are activated just like in ductal obstruction resulting in the acute pancreatitis. 06:00 Patients may also have some problems with intracellular transport of some of these digestive enzymes. 06:07 This happens during metabolic injury through exposure to alcohol, and also as a response to duct obstruction. 06:14 This further enhances the auto-wide digestion phenomenon. 06:18 This interruption of delivery of proenzymes to the lysosomal compartment can result in intracellular activation of the enzymes so these cells aren’t essentially eaten from the inside. 06:31 This acinar cell injury, again, results in activated enzymes and acute pancreatitis.
About the Lecture
The lecture Pancreatitis in Children: Pathology by Brian Alverson, MD is from the course Pediatric Gastroenterology.
Included Quiz Questions
Which lab test is most sensitive and specific for pancreatitis?
- Lipase
- Amylase
- GGT
- AST
- ALT
Which of the following is the most common cause of bile duct obstruction leading to acute pancreatitis?
- Gallstones
- Cystic fibrosis
- Choledochal cyst
- Neoplasm
- Parasite
Which of the following statements about pancreatitis is true?
- Children suffer attacks, which are more acute
- Children suffer less acute attacks of pancreatitis
- Adults suffer fewer pancreatitis attacks
- Incidence of attack is similar in all ages
- Incidence in children is greater
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is very helpful. Well organized and taught - I learned a lot
Not a typical pediatric topic, however very important topic as it is a diagnosis that must be considered in children. Thank you!