Playlist
Show Playlist
Hide Playlist
Pediatric Orthopedic Leg Problems: Blount's Disease, Legg–Calvé–Perthes Disease (LCPD), Slipped Capital Femoral Epiphysis (SCFE) and Osgood-Schlatter Disease (OSD)
-
Slides ChildrenLegProblems Pediatrics.pdf
-
Download Lecture Overview
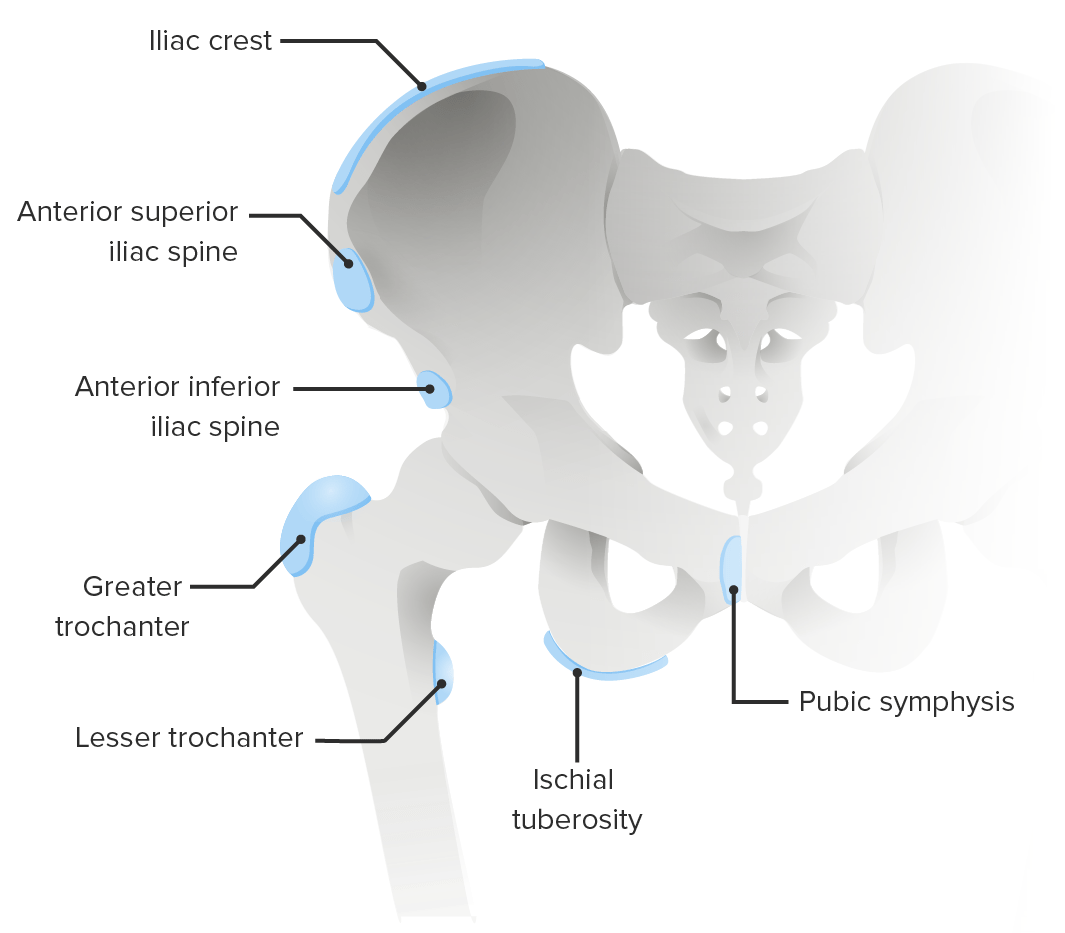
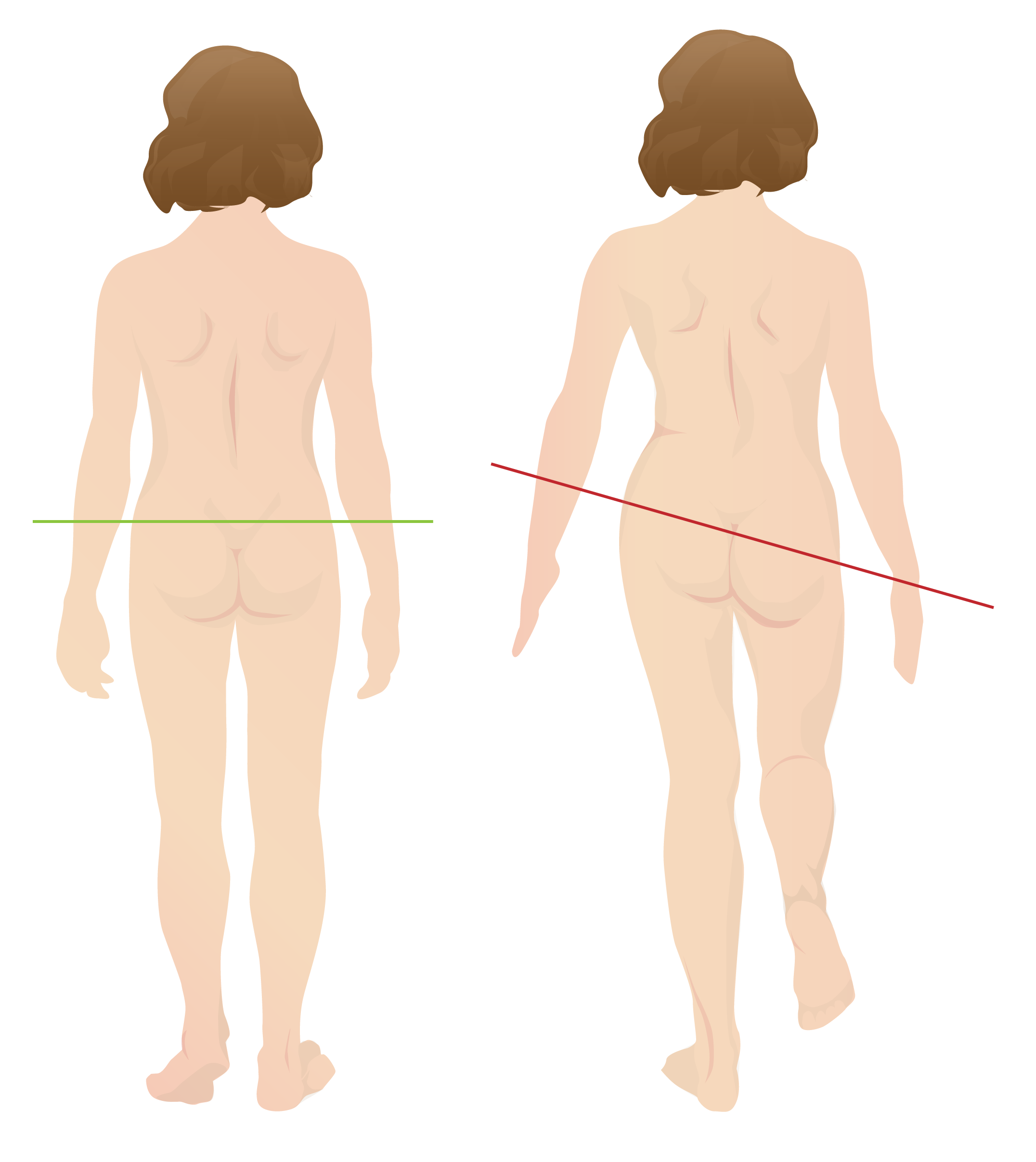
00:01 In this lecture, we’re going to discuss a variety of pediatric orthopedic leg problems. 00:07 Let’s start with Blount's disease. Blount’s disease is an abnormality on the medial aspect of the proximal tibial epiphysis where that side is a little bit shorter. This results in bowed legs or varus. 00:22 It usually presents in infants between one and three years of age. They tend to be walking on bowed legs. Usually, they're without pain, though sometimes there is some pain involved. 00:34 They also usually have a little bit of intoeing. The diagnosis can be confirmed on X-ray. If a patient is below three years of age, we generally will first brace them. This lowers the risk of degenerative joint disease and a later deformity. However, if it's severe or if they’re a little bit older, we use surgery to correct the structure of the joint especially if the brace isn’t working. You can see an example of this surgery having been performed here. Moving on to Legg-Calve-Perthes, Legg-Calve-Perthes is an interruption of blood flow to the femoral head and/or neck of the femur. This results in avascular necrosis of the hip. Patients may be shorter or have a delay in skeletal maturation. This can also cause a permanent deformity of the femoral head and acetabulum. Typically, Legg-Calve-Perthes happens in patients between 4 and 10 years of age. These patients will have a Trendelenburg gait. 01:43 They’ll have an irritable hip, slight pain, and a decreased range of motion. Later, there can be leg length discrepancy. We diagnose this condition on hip X-ray. As you can see on this X-ray here, this patient has a flattened acetabulum. Where the femoral head is sticking in, it’s flattened. 02:04 On the patient’s right side on the left side of the screen, you can see that hip is involved and the other side is normal. So, with Legg-Calve-Perthes disease, we often will start off with conservative management, rest, decreased activity, NSAIDs, and physical therapy. 02:24 For severe disease in children after about the age of eight, we will have a surgical repair. 02:30 Most patients function reasonably well until their 40s. But then they often need a hip replacement because the chronic damage to that hip results in a chronic osteoarthritis. Another condition of the hip that is very important and often shows up on exam is the slipped capital femoral epiphysis. 02:53 We call it SCFE for short. A SCFE is a really Salter–Harris 1 fracture. That is a transverse fracture right through the growth plate of the capital femoral epiphysis. This is due generally to mechanical forces on the hip in an adolescent child. Most of these patients are obese. The classic story is a child playing basketball, jumps off for a layup and then lands funny on his hip and suddenly has acute hip pain. 03:24 That would be an acute presentation. Sometimes patients present with chronic hip pain and then finally come in to see the doctor or they may have acute-on-chronic disease where their hip's been hurting a little bit for a long time and then they’re playing basketball and boom, it hurts a whole lot. 03:43 Typically, this happens in boys more than girls and around the age of 12 or 13. They may complain mostly of knee pain. Remember, pain can be referred when it's at the hip. The problem, the pain can be felt at the knee. Pain refer was common in this area. So, when we suspect a SCFE, we’re going to take a look at the patient’s X-ray and look at the lateral and AP views of the hip. 04:15 We’re going to draw something called Klein's line. Let’s look at this X-ray or this drawing of an X-ray for a minute. Do you see that dotted line there on the normal one? It should cut through the epiphysis of the hip joint. If the patient has a SCFE, the epiphysis has floated down and thus the Kline’s line will not cut through that epiphysis. So, that’s how you can tell the difference as to whether there’s been a SCFE or not. So, here’s a few examples of SCFEs. You can see that before X-ray, if you were to draw that Kline’s line, the epiphysis has floated down on the physis and is now off the metaphysis. In patients with SCFE, there is a risk for avascular necrosis and eventual further slippage. So, this is an orthopedic emergency. These patients will be needed to be admitted to the hospital for a definitive surgical repair. What they will do is they will re-approximate that epiphysis and then put a screw through it to hold it in place. So, let's switch gears now to the knee and let’s talk about Osgood-Schlatter disease. Osgood-Schlatter disease is a painful traction apophysitis of the tibial tubercle on the anterior part of the tibia. Let me say that clearly. 05:44 Where the insertion is of the quadriceps past the knee and down on to the tibial tuberosity, that area right there over time is undergoing stress and will have small microfractures. You can see that in this picture here. It’s more common in teens who are active in sports especially those who are doing running or jumping activities. Basically, this is a repetitive microtrauma on that tibial tubercle which results in inflammation, microfractures, and pain. 06:19 I think it would be beneficial to explain how bone growth outpaces muscle and tendon development, resulting in increased tension and irritation at the apophysis. 06:30 This phenomenon is especially significant during adolescent growth spurts when bones grow more rapidly than muscles and tendons can adapt, creating tension at the tibial tuberosity where the patellar tendon attaches. 06:46 If we were to get an X-ray which is not necessary, you may see protrusion of the tibial tubercle on exam and you may see it on the X-ray as well. 06:56 Typically, a good physical exam maneuver is to have them squat. When they’re standing from a squat position, they should have pain over that tibial tuberosity. Also, you may have tenderness to palpation over that tibial tubercle. Like I said, the X-ray isn’t usually needed. But in this X-ray where that white arrow is, you can see that the tibial tuberosity has become inflamed, has some microfractures and they start to calcify. 07:24 How do we treat Osgood-Schlatter’s? We treat it generally with NSAIDS, and rest, and elevation. 07:31 We like to give children quadriceps and hamstring stretching exercises. In fact, stretching the hamstrings is one of the most important ways that we can prevent this in runners. We like to do hip and core strengthening as well. With core strengthening of the core muscles, Osgood-Schlatter is less likely to happen. 07:52 If it does happen, we usually refer to physical therapy. This is not an operative condition. 07:59 That’s all I have to tell you today about orthopedic problems in children in the legs. Thanks for your attention.
About the Lecture
The lecture Pediatric Orthopedic Leg Problems: Blount's Disease, Legg–Calvé–Perthes Disease (LCPD), Slipped Capital Femoral Epiphysis (SCFE) and Osgood-Schlatter Disease (OSD) by Brian Alverson, MD is from the course Pediatric Rheumatology and Orthopedics. It contains the following chapters:
- Pediatric Orthopedic Leg Problems
- Legg-Calvé-Perthes Disease (LCPD)
- Slipped Capital Femoral Epiphysis (SCFE)
- Osgood-Schlatter Disease (OSD)
Included Quiz Questions
Slipped capital femoral epiphysis (SCFE) is an example of which of the following types of fracture?
- Salter-Harris 1 fracture
- Salter-Harris 5 fracture
- Colles fracture
- Salter-Harris 3 fracture
- Jones fracture
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I enjoyed the overview and the clear explanations of the different diseases. I would have liked more details concerning the clinical exam. However this lecture does serve the purpose of giving the student a clear view of the most common paediatric diseases.