Playlist
Show Playlist
Hide Playlist
Pulmonary Embolism: Diagnosis
-
Emergency Medicine Bord Pulmonary Embolus.pdf
-
Download Lecture Overview
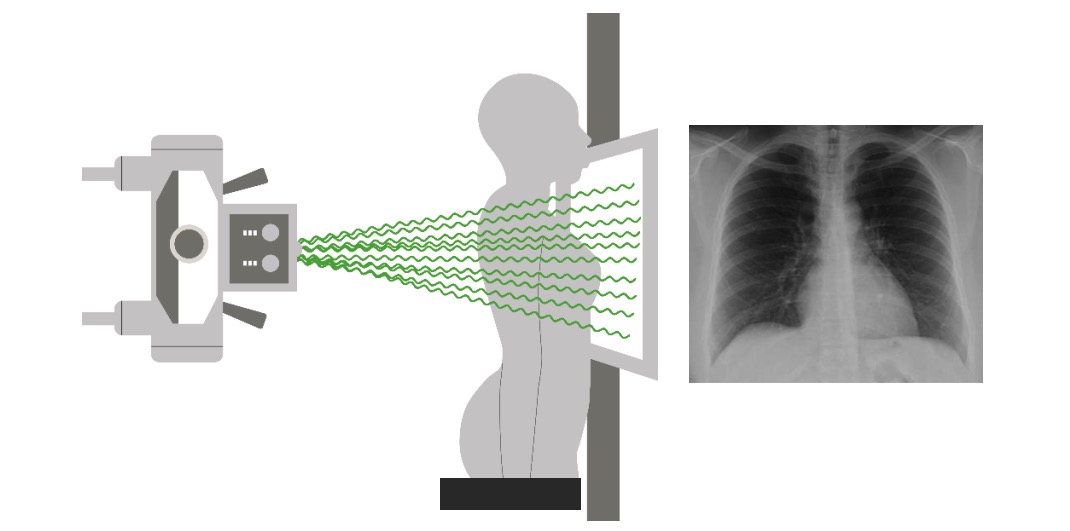
00:00 So when we’re thinking about other testing for patients in whom we’re thinking about a pulmonary embolus, we wanna go back and start thinking about keeping our differential broad. 00:10 So we’re thinking about a pulmonary embolus but we also wanna make sure we’re thinking about other things potentially as well. 00:16 So we wanna do our basic lab work. 00:18 We wanna get an EKG to assess for any evidence of ischemia, to assess for an arrhythmia. 00:24 Often times when patients come in with shortness of breath or chest pain, for the most part they’ll get a chest x-ray to take a look and make sure there’s not something else causing it. 00:33 So chest x-rays can show you if there’s pneumonia, if there is a pneumothorax, if the lung has collapsed. 00:38 You potentially might wanna get a troponin if you're thinking about a pulmonary embolus. 00:43 A troponin is helpful to evaluate for acute coronary syndromes but also in patients who have large pulmonary embolus. 00:49 They can have a positive troponin due to the fact that there’s strain placed on the heart. 00:55 You potentially consent a pro-BNP. 00:58 Pro-BNP is thought to be a marker of a strain on the heart as well and also heart failure and can be elevated in patients who have pulmonary embolus. 01:08 And then our PE specific testing, so the D-dimer is the screening blood test for pulmonary embolus and as a screening test we send it and if it’s negative we’re done and if it’s positive then we need to go ahead and do additional testing. 01:23 The last test that we do for pulmonary embolus is a CT angiogram of the chest or VQ scan, and these are more advanced imaging techniques than a chest x-ray. 01:33 The CT angiogram takes a look at the blood vessels very closely and it’s a CT scan that’s done with IV contrast and it’s a good test to look for pulmonary embolus. 01:44 And if the patient is unable to get a CT angiogram of the chest, they can get a VQ scan and we’ll talk about both of these studies in a moment. 01:52 So let’s go back to calculating our risk score. 01:56 Now we mentioned if our patient is PERC negative, they have a less than 2% risk of pulmonary embolus and for this patient who fall into this category there is no indication for additional testing. 02:06 For a patient who is Well’s criteria low risk, for those patients we wanna think about D-dimer testing, so someone is positive in the world of PERC and they are low risk in their D-dimer score, we can go ahead and get a D-dimer. 02:23 If the D-dimer is negative, you can likely stop your work up. 02:26 For patients who are moderate or high risk in Well’s criteria, those are patients who need additional imaging. 02:34 You don’t wanna send a D-dimer in those patients because you already have a higher suspicion that the patient may have a pulmonary embolus. 02:40 So when they fall into that category where they’re moderate or high risk in Well’s, for those patients you can get a CT angiography as the initial testing for pulmonary embolus. 02:49 For patients who can’t get a CT angiography study, they can get a VQ scan. 02:55 So patients who can’t get a CT angiography are patients who potentially have renal disease because it does involve IV contrast and IV contrast is contraindicated in patients with severe renal disease. 03:08 Our patients who are allergic to IV dye also cannot get CT angiography. 03:14 You know, subset of patients who is always a little bit controversial about what imaging study to get are pregnant patients. 03:20 Pregnant patients, generally, CT angiography is actually recommended. 03:25 Meaning, you always wanna make sure that you discuss that with your patient because it does expose them to some radiation and as well as the baby to some radiation. 03:33 But we generally will recommend CT angiography because it can tell you if there’s a pulmonary embolus there but can also tell you whether or not there is other stuff going on in the lungs that might not necessarily have been seen on the chest x-ray. 03:45 VQ scan does have some limitations that we’ll talk about in a moment. 03:49 Now, I just wanna be clear here that one thing that’s very important to think about is that you are thinking about your clinician gestalt. 03:56 So we have all of these decision rules but actually there have been lots of studies that show that clinician gestalt, so whether or not you think that the patient has a PE, is actually sometimes performs better than any of these testing. 04:09 So we talk about these tests a lot and these decision rules a lot but really using your medical instincts can sometimes really serve you well in this situations. 04:19 So definitely make sure you’re using these decision rules but as you get on in your training and in your careers, your clinical gestalt can really serve you quite well.
About the Lecture
The lecture Pulmonary Embolism: Diagnosis by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
Which of the following tests is NOT recommended in the evaluation of pulmonary embolism?
- Venous doppler
- Troponin
- Pro-BNP
- D-Dimer
- VQ scan
In calculating the risk for pulmonary embolism, which of the following statements is INCORRECT?
- D-dimer testing is indicated in a patient with high risk on Well’s criteria.
- Additional testing is not indicated in PERC-negative patients.
- There is less than 2% risk of pulmonary embolism in a PERC-negative patient.
- If the D-dimer is negative in a low-risk Well’s criteria patient, further work-up can be discontinued.
- VQ scan may be done in patients who cannot undergo contrast angiography.
Which of the following statements regarding CT angiography is INCORRECT?
- Pregnancy is an absolute contraindication to CT angiography.
- CT angiography is indicated as the initial test for pulmonary embolism in patients who are in the moderate or high-risk categories by Well's criteria.
- CT angiography is done with the use of IV contrast.
- Renal failure patients may opt for VQ scan instead of CT angiography.
- CT angiography is superior to a VQ scan in evaluating pulmonary embolism.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |