Playlist
Show Playlist
Hide Playlist
Paroxysmal Nocturnal Hemoglobinuria (PNH): Pathophysiology
-
Slides Paroxysmal Nocturnal Hemoglobinuria PNH.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
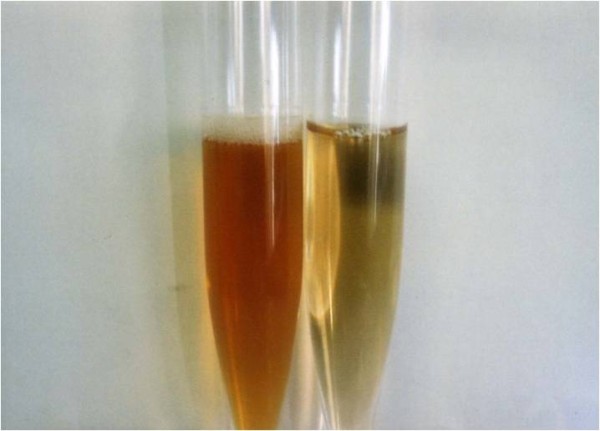
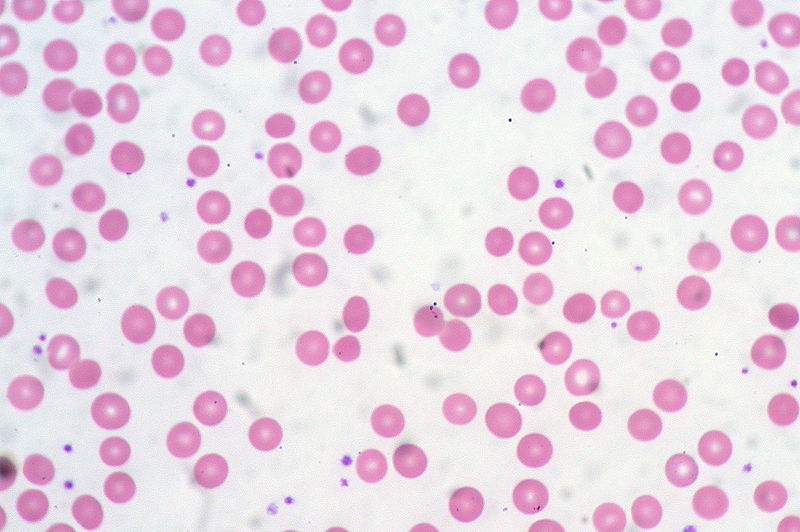
00:01 Let’s talk about PNH further and its pathophysiology. 00:03 You must know the following. 00:05 You have a component called – Your focus here, please find decay-accelerating factor. 00:12 So decay accelerating factor is a factor which normally controls how much complement activation takes place. 00:20 Is that clear? So for the most part, think about this, say that you have too much complement activity, examples of increased complement pathologies that you’re quite familiar with. 00:32 If the patient has angioedema and it’s the hereditary type, and so what’s happening? Around the mucus membrane, you have increased vasodilation, you all know about C1 inhibitor deficiency, correct? That’s hereditary angioedema. 00:50 Too much complement activation. 00:54 You can have too much complement activation that may then cause, well, destruction to the glomerular basement membrane. 00:59 That brings you to type II MPGN and it’s called nephritic factor where it stabilizes C3 convertase. 01:07 This is another major complement pathology where you cannot control the complement activity. 01:15 And so what happens is that we’ll take a look at this further and we have a mutation to decay accelerating factor, which isn’t functioning properly, and so therefore, you cannot regulate the amount of complement activity. 01:29 Once again, where is this complement activity and what kind of cells is this influencing? RBCs and platelets. 01:35 Those are the two that you pay attention to clinically. 01:39 Technically, yes, it’s the neutrophils as well. 01:41 Platelets, what are you going to have? Excess activity, thrombosis. 01:46 What about the RBC? You will destroy it. 01:50 Most likely where? Based on the name, hemoglobinuria. 01:53 Intravascular hemolysis. 01:55 Intravascular, right? So you have destruction of the RBC, right there and then in your blood vessel. 02:02 The absence of these proteins, which proteins? The decay-accelerating factor. 02:06 There’s another one that I will introduce to you. 02:09 It’s called membrane-inhibitor reactive lysis, MIRL. 02:13 We’re going to build bit by bit by bit so that when you deal with PNH, any angle that you’re asked on your boards, you’ll be able to answer it. 02:23 Let it be the biochemistry, the pathology, the clinical picture, and even some of the pharmacology here. 02:29 So in the absence of your proteins, who is now susceptible? The RBCs. 02:34 When? Well, now, take a look at the middle name of paroxysmal. 02:38 It’s nocturnal, so at night is when the RBCs are being destroyed by whom? The complement. 02:47 Why? Because decay-accelerating factor can’t control the complement anymore. 02:53 Why at night? Well, when you sleep at night, what happens to your breathing, your respiratory rate? Hopefully, you’re relaxing and your breathing rate decreases. 03:05 When your breathing rate decreases, then you end up building up transiently a little bit of carbon dioxide that is just enough carbon dioxide that the body’s retaining in which you created what kind of environment? Acidotic or alkalotic environment? Acidotic environment. 03:20 Good. 03:22 So at night, acidotic environment, wow! This is the perfect environment for complement. 03:27 You go crazy. 03:29 So they’re partying all night, the complement is, and in the process, they’re destroying your RBCs. 03:33 You wake up in the morning, what do you find? Oh, look at the third name. 03:38 Hemoglobinuria. 03:40 The name has everything that you require for you to properly diagnose your patient clinically. 03:43 The only thing that you cannot forget is the fact that your patient is going to present with thrombosis. 03:50 Do not forget that, please, when you’re dealing with PNH.
About the Lecture
The lecture Paroxysmal Nocturnal Hemoglobinuria (PNH): Pathophysiology by Carlo Raj, MD is from the course Hemolytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
In the absence of the decay accelerating factor (DAF), RBCs are susceptible to which of the following?
- Complement-mediated damage
- Loss of major histocompatibility complex
- Natural killer cells mediated destruction
- Lymphocyte-mediated destruction
- Extravascular hemolysis
Hereditary angioedema result from a deficiency of which of the following?
- C1 esterase inhibitor
- Membrane attack complex
- C3 convertase
- C5 convertase
- C4 esterase inhibitor
Hemolysis in PNH is mainly nocturnal due to which of the following?
- Acidic environment
- Increased melatonin production
- Decreased CO2 at night time
- Hyperventilation at night time
- Alkalotic environment
Hypercoagulable state in PNH is due to which of the following?
- Increased platelet function
- Blood stasis
- Decreased production of coagulation factors
- Increased production of coagulation factors
- Decreased platelet function
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |