Playlist
Show Playlist
Hide Playlist
Paroxysmal Nocturnal Hemoglobinuria (PNH): Etiology
-
Slides Paroxysmal Nocturnal Hemoglobinuria PNH.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
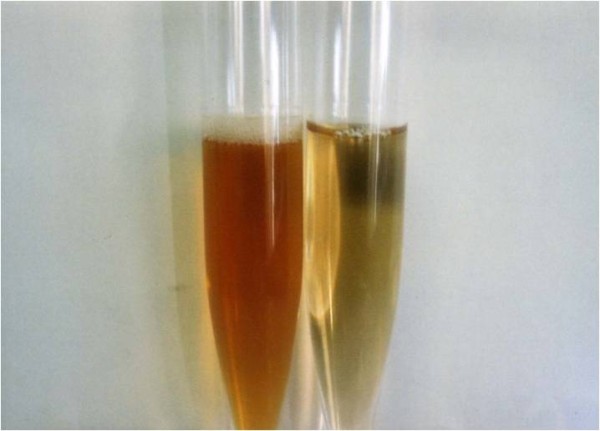
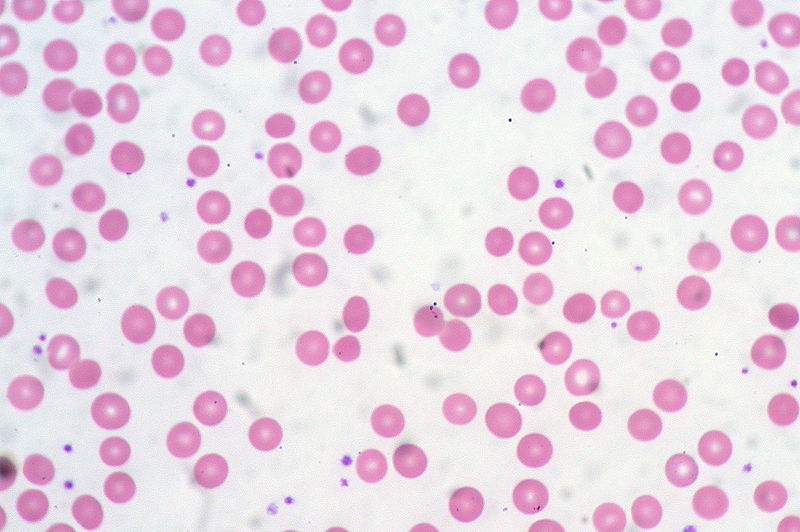
00:01 Let’s take a look at paroxysmal nocturnal hemoglobinuria. 00:04 Everything that you want to know about this condition is actually in the name. 00:09 And so let’s go ahead and dissect each part of this. 00:12 First, my issue is the fact that, well, I’m not able to properly control the destruction of my RBC. 00:21 Really? Mm-hmm. 00:22 Now, a couple of other things as well that you want to keep in mind, remember earlier, we had our discussion of G6PD deficiency and I told you to keep it as a differential, chronic granulomatous disease. 00:34 Well, here, with this picture of paroxysmal nocturnal, granted we’re going to focus upon the RBC. 00:41 However, as far as you’re concerned, the clinical picture is a lot broader. 00:46 What I mean by that is if you take a look at the statement here, you’ll understand that not only is my RBC being affected, as is my neutrophil, but you really, ladies and gentleman, the clinical picture of platelets becomes important. 00:59 What I mean by that is it's not that you’re going to have excess destruction of your platelet. 01:04 In fact, you end up having excess stimulation of platelet function. 01:09 So if you have excess platelet functioning or you have excess activity of your platelets, then you’re forming tons of? Thrombi. 01:16 Where? Up and down the body. 01:19 That’s your first clinical picture. 01:21 The patients that walk in with PNH are suffering from some kind of thrombotic episode, including what? Well, maybe there might be portal hypertension. 01:31 Why? Well, the portal vein underwent thrombotic episodes. 01:35 So imagine now, the portal vein, which should normally be draining your superior mesenteric vein and the splenic vein have now become thrombosed. 01:46 And if it’s thrombosed, then you’re going to back up into, well, your portal hypertension. 01:50 So that will be your esophageal varices, that will be caput medusae, and that will be your hemorrhoids, wouldn’t it? And so that’s portal vein thrombosis. 01:58 What if it was an issue with my hepatic vein? You’d call that Budd-Chiari, don’t you? So Budd-Chiari type of syndrome would be an issue in the liver, especially zone 3 or there might be inferior vena cava thrombosis, you get my point. 02:11 So you want to be very smart about how you are developing the thrombus, where you’re developing the thrombus and how your patient’s going to present with that thrombus. 02:21 Platelets is an issue. 02:23 What about these RBCs? Take a look at the name. 02:26 Paroxysmal, episodically. 02:29 Nocturnal, most commonly at night. 02:32 And then you wake in the morning and you find red urine, hemoglobinuria. 02:37 At this point, you should be really familiar with the term hemoglobinuria and understanding what kind of hemolysis would this be. 02:46 Intravascular hemolysis, what happens to your haptoglobin level? Decreased. 02:51 Remember hemoglobin requires a chaperone. 02:55 It binds to haptoglobin, free levels of haptoglobin will drop. 03:00 This complex will then go to your glomerulus and the hemoglobin will then get filtered, resulting in hemoglobinuria. 03:07 Well, one of the discussions that we had earlier when we did microcytic anemia, was that when you are losing hemoglobin, along with it what might you be losing? What is that heme comprised of? Oh, yeah, iron. 03:22 So during hemoglobinuria, you might also be losing iron resulting in iron deficiency anemia. 03:27 A lot of things here of this particular statement, but I’m giving you a global picture of paroxysmal nocturnal hemoglobinuria. 03:34 We will then walk into further details. 03:37 Now, there is a specific component of your deficiency and this is known as a glycosylphosphatidylinositol. 03:47 Keep that in mind because at some point you will be responsible in great depth to go into what’s known as flow cytometry with PNH, GPI-linked proteins.
About the Lecture
The lecture Paroxysmal Nocturnal Hemoglobinuria (PNH): Etiology by Carlo Raj, MD is from the course Hemolytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following types of cells are NOT affected in paroxysmal nocturnal hemoglobinuria?
- Mast cells
- Platelets
- Lymphocytes
- RBCs
- Neutrophils
Which of the following is NOT a manifestation of portal vein thrombosis?
- Pleural effusion
- Esophageal varices
- Ascites
- Hemorrhoids
- Caput medusae
Which of the following structures with thrombosis results in Budd-Chiari syndrome?
- Hepatic vein
- Portal vein
- Inferior vena cava
- Superior mesenteric vein
- Splenic vein
Which of the following types of anemia can be accompanied by paroxysmal nocturnal hemoglobinuria?
- Iron-deficiency anemia
- Sideroblastic anemia
- Pernicious anemia
- Dilutional anemia
- Anemia of chronic disease
Which of the following is deficient as a result of paroxysmal nocturnal hemoglobinuria?
- GPI-linked proteins
- Ankyrin
- None of these
- Tyrosine kinase
- Spectrin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This topic is so well explained. I really like the clear and succint style.