Playlist
Show Playlist
Hide Playlist
Pancreatitis: Diagnosis & Management
-
Slides Pancreas General Surgery.pdf
-
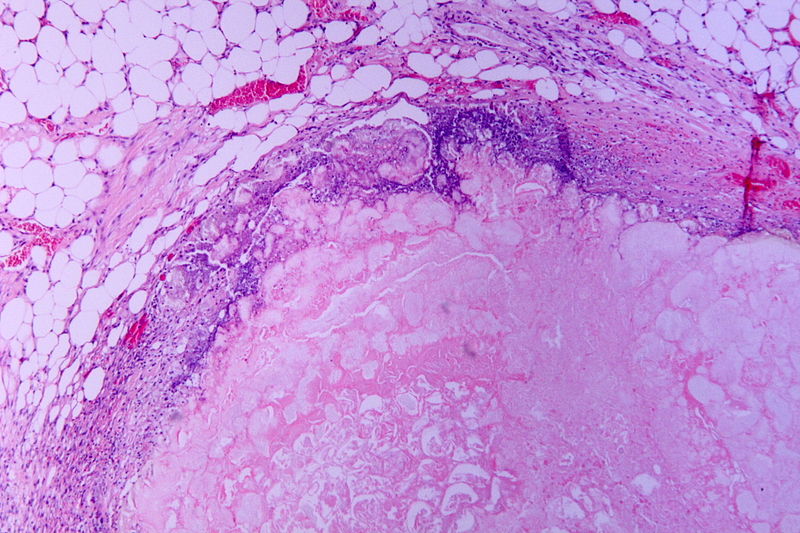
Download Lecture Overview
00:01 Here’s my management schematic of acute pancreatitis. When a patient presents with pancreatitis, I like to say, does the patient have a biliary source or a non-biliary source. For biliary source, in other words, gallstone-related diseases, a cholecystectomy whether it’s done laparoscopically or open should be offered to the patient on the same admission. The reason for this is because recurrence of pancreatitis can occur if the patient is discharged after the resolution of pancreatitis but before the gallbladder is removed. If there is a common bile duct obstruction, our GI doctors are called to perform an endoscopic retrograde cholangiopancreatography. Remember from previous lectures that an ERCP may be both diagnostic and therapeutic. The therapeutic side of an ERCP allows the clearance of the common bile duct of the bile stones. Now, let’s take a look at the non-biliary causes. Remember, alcohol, hypertriglyceridemia, hypercalcemia, and hyperparathyroidism. 01:09 The main determinant of the next step of management is whether or not you suspect there is necrosis of the pancreas. If you do not suspect necrosis of the pancreas, the treatment is largely supportive. 01:20 Early nutrition is advocated in modern medicine. We want to minimize further risk of pancreatitis. 01:28 This involves very important counseling to the patient to minimize smoking and drinking. 01:33 If, however, the non-biliary pancreatitis is suspected to be necrotic, this is where a CT scan cross sectional imaging may be very, very important. These patients have partial ischemia of the pancreas and can deteriorate quite rapidly. Oftentimes, these patients are transferred to the intensive care unit. Depending on whether or not there is clinical deterioration, a surgical necrosectomy or removing the portions of the pancreas that’s necrotic may be necessary. I like to pose a question to you. What is the difference between acute and chronic pancreatitis? I’ll give you a second to think about this. Chronic pancreatitis is a progressive inflammatory process that results in permanent damage to both the exocrine and the endocrine function of the pancreas, specifically for endocrine function of the pancreas. Remember that oftentimes, these patients require replacement of pancreatic enzymes. One of the hallmarks of exocrine dysfunction or the lack of endocrine secretions is fatty stools. Acute pancreatitis on the other hand is usually limited with supportive therapy. Of course, acute pancreatitis patients can progress to chronic pancreatitis particularly if they continue imbibing alcohol. What about labs for chronic pancreatitis? We visited the labs for acute pancreatitis. Very different than acute pancreatitis is the fact that in chronic pancreatitis, your total bilirubin, amylase, lipase, alkaline phosphatase may all be normal and especially the amylase/lipase. This is what we call a burnt out pancreas. A burnt out pancreas, it is lacking endocrine function. Therefore, amylase and lipase may also be normal or even in fact, decreased. Now, some important signs, although rarely seen but often tested. 03:35 Hemorrhagic pancreatitis is an important topic to discuss. As you see from these images, there are classic Cullen sign and Grey Turner's signs associated with hemorrhagic pancreatitis. 03:46 This may be induced by vessel necrosis in intraparenchymal activation of enzymes that may cause bleeding in the retroperitoneum. Classically speaking, we find periumbilical or flank ecchymosis. Once again, to remind you, these are signs of potential retroperitoneal bleeding tracking along the abdominal wall.
About the Lecture
The lecture Pancreatitis: Diagnosis & Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is NOT standard in biliary pancreatitis management?
- Pancreatectomy
- Laparoscopic cholecystectomy
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Supportive treatment
- Intravenous fluid resuscitation
A patient is deteriorating after a diagnosis of pancreatitis was made. Further workup including a CT scan was performed and showed extensive areas of necrosis in the pancreas. Which of the following is the most likely next step?
- Necrosectomy
- Pancreatectomy
- Laparoscopic cholecystectomy
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Observation
Which one is NOT associated with hemorrhagic pancreatitis?
- Virchow’s sign
- Grey-Turner's sign
- Vessel necrosis
- Cullen's sign
- Flank ecchymosis
When comparing acute pancreatitis to chronic pancreatitis, which of the following is true about lab findings?
- Amylase and lipase levels are typically lower in chronic pancreatitis than in acute pancreatitis.
- Amylase and lipase levels are elevated in both acute and chronic pancreatitis.
- Alkaline phosphatase levels are always higher in chronic pancreatitis than in acute pancreatitis.
- Total bilirubin is always elevated in chronic pancreatitis.
- Alkaline phosphatase levels are normal in acute pancreatitis and low in chronic pancreatitis.
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
YOU DO NECROSECTOMY ONLY IN CASES OF INFECTED NECROSIS AFTER 4 WEEKS OF ADMISSION