Playlist
Show Playlist
Hide Playlist
Pancreatic Pseudocyst and Pancreatic Cancer
-
Slides Pancreas General Surgery.pdf
-
Download Lecture Overview
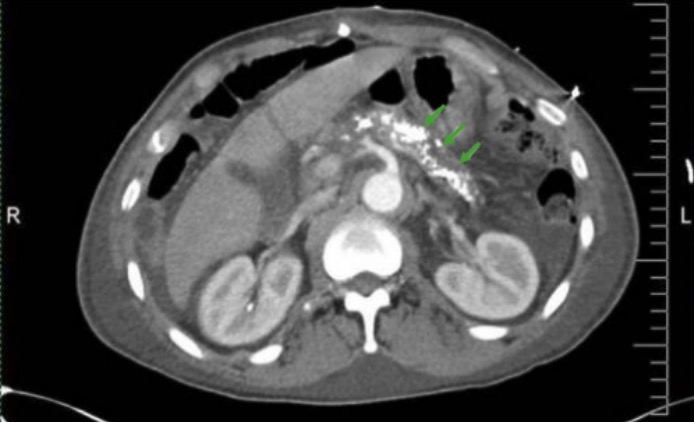
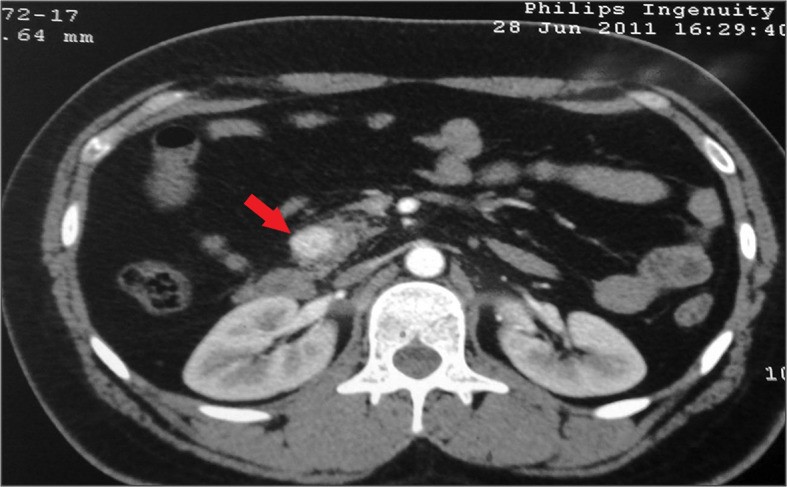
00:01 Let’s move on to a potential complication of acute pancreatitis. We’re going to discuss next the pancreatic pseudocyst. Pancreatic pseudocyst can be a sequelae of chronic or acute pancreatitis. 00:17 Usually, there is a pancreatic ductal disruption. Pseudocysts have high concentrations of digestive enzymes and the walls are formed by the stomach, pancreas, colon, and mesocolon. 00:31 As the name implies, pseudocyst means that it does not have all the layers of the epithelium. 00:37 The enlargement of pseudocyst can cause pain and obstruction. This is how patients typically present. 00:45 When a CT scan of the abdomen and pelvis is obtained, one noticed on this image a large fluid containing cyst budding both the pancreas and the stomach. From this image, you can imagine how the large size of the cyst can both cause compressive symptoms on the stomach. This may lead to early satiety, nausea, or vomiting. Certainly, with the continued enlargement may also cause significant midepigastric to left upper quadrant abdominal pain. There are some indications for drainage or surgery for this cyst. We used to always drain pseudocysts if it reached a certain size. 01:24 But that’s no longer necessary. Here are the indications for surgery. If there is a rapidly enlarging pseudocyst as indicated by symptoms or by interval of CT scans, that might be an indication for surgery. 01:39 Patients with worsening pain or unmanageable pain or early satiety resulting in weight loss may be candidates for a drainage. Lastly, complications of a pseudocyst including rupture and infection are clearly indications for surgery. Luckily, rupture is a rare phenomenon. Now, let’s move to pancreatic cancer. Although lots of progress has been made in pancreatic cancer in terms of surgical management, unfortunately, most of pancreatic cancer patients die within a short amount of time after surgery. What are some risk factors that are associated with pancreatic cancer? Chronic pancreatitis, diabetes, smoking, family history, as well as age and gender; pancreatic cancer can lead to obstructive jaundice, weight loss, and epigastric discomfort. 02:40 There may be common bile duct dilatation particularly with the head of the pancreas' lesions. 02:47 We usually get a CT, CT scan of the abdomen and pelvis and ERCP as part of the workup. 02:53 More and more in modern medicine, we do endoscopic ultrasound potentially with a guided biopsy. 03:00 Pancreatic cancer is likely due to multifactorial causes. The picture is very complex. 03:09 We do associate them with diabetes, pancreatitis, and smoking and yet, not a single one of these entities can explain pancreatic cancer alone. Remember, the vast majority of pancreatic cancers are de novo. 03:26 It’s hard to delineate exactly what the etiology is. As we previously alluded, weight loss, jaundice, and maybe pain to the back, or a distended gallbladder when the common bile duct or the head of the pancreas is obstructed. That sign is called the Courvoisier's sign. If it's determined that surgery is necessary, we perform a pancreaticoduodenectomy commonly known as the Whipple procedure. 03:57 In the Whipple procedure, part of the stomach, duodenum, and pancreas are all resected. 04:03 Following this surgery, like plumbers, all of the GI system is reconfigured to allow proper drainage. 04:11 Determinants of resectability is very important. Any significant peripancreatic vessel encasement such as the superior mesenteric vein may deem the patient unresectable. Clearly, at the time of surgery, all patients undergo thorough examination of the abdomen evaluating for potential distant metastases such as liver or stomach. Upon entering the abdomen, if it is noted that there’s peritoneal seeding of cancer also known as peritoneal carcinomatosis, the patient is deemed unresectable. 04:48 I like to pose a question to you. What's the next step of management with patients with unresectable pancreatic cancer? I’ll give you a moment to think about this. The answer is biliary bypass. 05:04 Unfortunately, because no cure can be expected with patients with unresectable disease, at this point, we do palliative surgery for symptomatic control. Biliary bypass includes bypass of the common bile duct to a loop of small intestines. Important clinical pearls to remember: In acute pancreatitis, early nutrition is advocated and does not impair resolution of the pancreatitis. Remember, a high yield association between hyperparathyroidism, hypercalcemia, and pancreatitis. Thank you very much for joining me on this discussion of pancreas.
About the Lecture
The lecture Pancreatic Pseudocyst and Pancreatic Cancer by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is TRUE about pancreatic pseudocysts?
- It may result as a sequela of both acute and chronic pancreatitis.
- It is located posterior to the pancreas.
- The pancreatic ductal system is usually intact.
- It is lined by a membrane with all layers of epithelium.
- It is precancerous.
Which of the following scenarios is LEAST likely to require surgical drainage?
- A 31-year-old male with a stable and asymptomatic 10 cm pancreatic pseudocyst.
- A 29-year-old female with a rapidly enlarging pancreatic pseudocyst.
- A 51-year-old female with worsening abdominal pain found to have a pancreatic pseudocyst.
- A 32-year-old female with progressing necrotizing pancreatitis.
- An 85-year-old female with a ruptured pancreatic pseudocyst.
Which one of the following factors does NOT increase the risk of developing pancreatic cancer?
- Female sex
- Smoking
- Diabetes mellitus
- Family history of pancreatic cancer
- African-American race
In which of the following scenarios is the Courvoisier's sign MOST likely to be positive?
- A 31-year-old male with pancreatic cancer located in the head of the pancreas.
- A 29-year-old female with a rapidly enlarging pancreatic pseudocyst.
- A 51-year-old female with gallbladder cancer.
- A 32-year-old female with necrotizing pancreatitis.
- An 85-year-old female with pancreatic cancer located in the tail of the pancreas.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |