Playlist
Show Playlist
Hide Playlist
Pancreatic Abnormalities
-
Slides Pancreatic Abnormalities.pdf
-
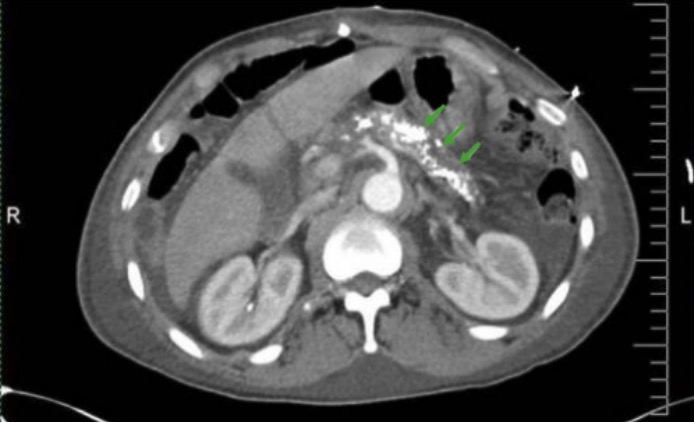
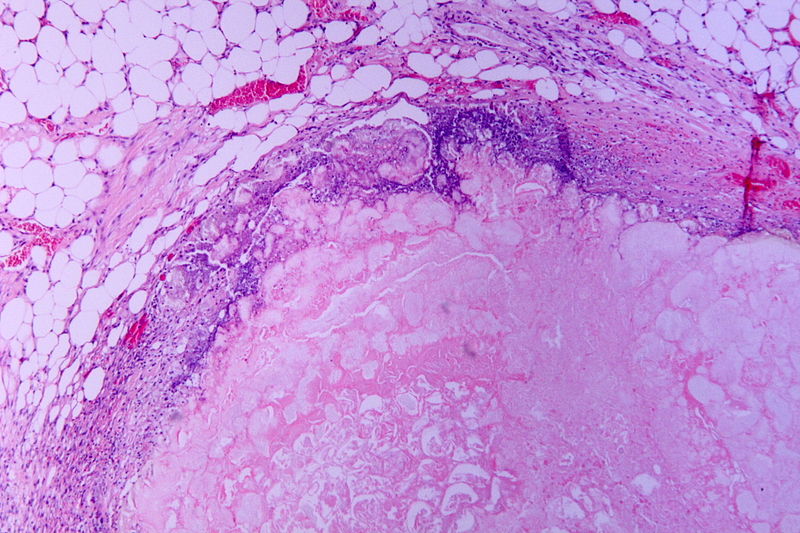
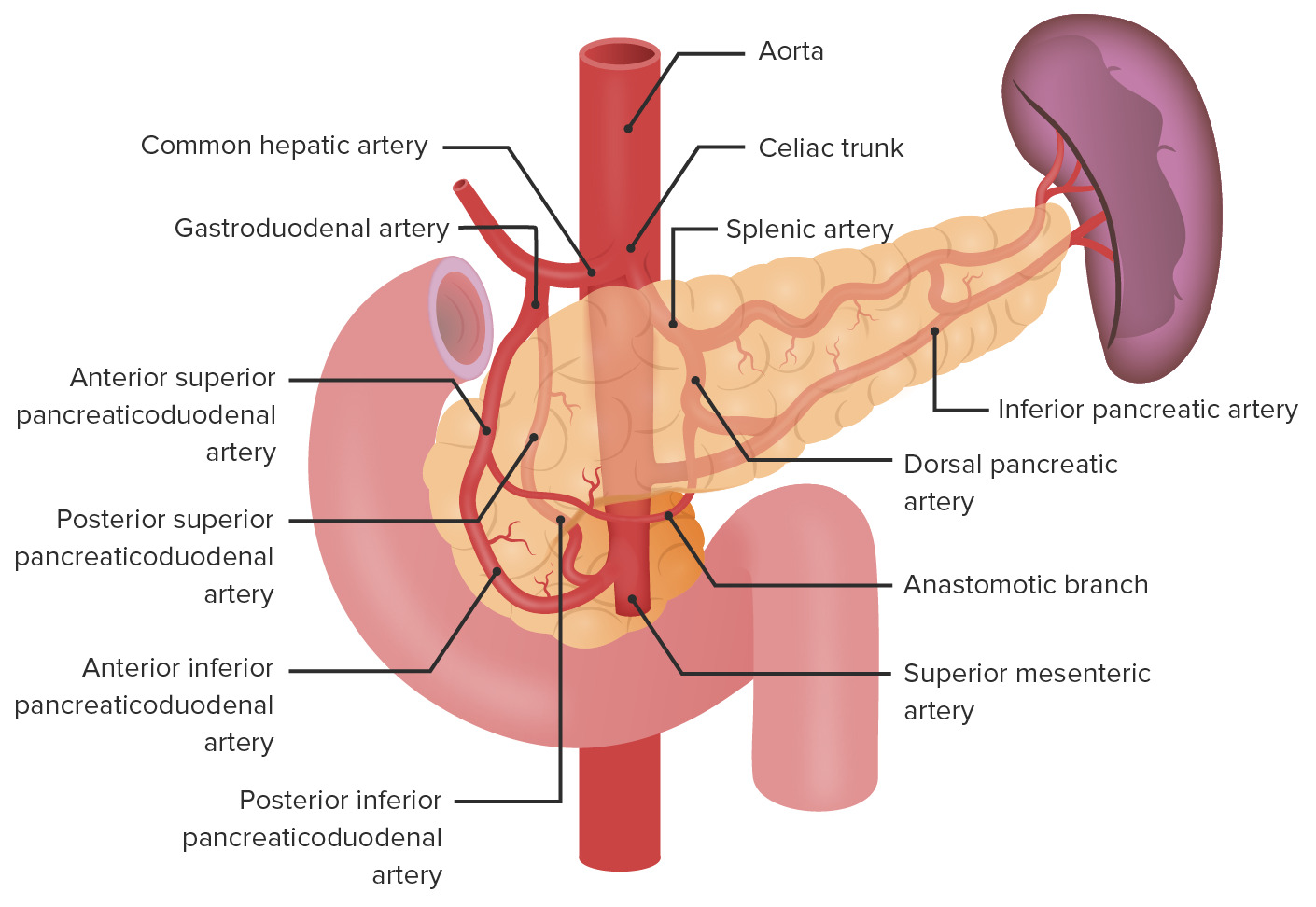
Download Lecture Overview
00:00 So let's talk a little bit about pancreatic abnormalities now. 00:04 Let's start by taking a look at this case. 00:06 This patient came in with abdominal pain and had a CT of the abdomen and pelvis. 00:10 So can you describe these findings? What do you see here? And let's keep this image in mind as we move on to the rest of the talk and we'll come back to it in the end. 00:21 So pancreatitis is inflammation of the pancreatic tissue which results in breakdown of the ducts and leakage of the pancreatic juices. 00:30 Clinically this presents as persistent upper abdominal pain, nausea and vomiting. And really pancreatitis is the clinical diagnosis. 00:39 However, imaging is often performed to take a look at any other causes of the pancreatitis that may not be clinically decided. 00:47 So what are some common causes? Alcoholism is really the most common cause of pancreatitis. 00:54 Obstruction of the duct by gallstones is also very commonly seen. 00:58 A contrast enhanced CT is really used primarily to look at the cause and the complications, and that's usually where we began when the patient comes in with the possibility of pancreatitis. 01:11 So what are some imaging findings of acute pancreatitis? You can have diffused or focal enlargement of the pancreas. 01:19 You can have peripancreatic inflammatory change and you can have ductal dilatation. 01:25 Those are the three key findings. 01:27 There are many complications associated with acute pancreatitis and these are usually a result of the enzymes that leak out. 01:34 An acute fluid collection is one of them and we'll review all of these in detail. 01:39 You can have development of a pseudocyst. 01:41 You can have pancreatic necrosis which is a result of the juices that causes destruction of the pancreatic tissue. 01:49 You can have pancreatic abscess formation and you can have pseudoaneurysm. 01:54 Again because of those enzymes that leak out and destroy the walls of the blood vessels surrounding the pancreas. 01:59 So let's take a look at the CT image. 02:02 What do you see here? So let me point out some of the anatomy, so here right is the pancreas. 02:08 This is normal pancreatic tissue. 02:11 Here you have bowel with air and contrast within the bowel. 02:17 And then what is this area in between? This is not seen in normal anatomy. 02:22 So this is something pathological. 02:24 This is what pancreatic inflammation looks like. 02:27 So the pancreas is slightly enlarged and there is a lot of peripancreatic fats stranding. 02:31 So this is one of the earliest signs of acute pancreatitis. 02:34 What's the difference between a pancreatic pseudocysts versus an acute fluid collection? So both of these can develop as a complication of acute pancreatitis. 02:46 An acute fluid collection actually develops within 48 hours of the onset of the acute pancreatitis whereas a pseudocyst develops 4 weeks after the onset. 02:55 So it's more delayed. An acute fluid collection lacks of fibrous walls so it's a collection of fluid but isn't really walled off, while a pseudocyst does actually have a fibrous wall associated with it. 03:05 And an acute fluid collection commonly occurs in or near the pancreas, whereas a pseudocyst commonly occurs near the pancreas but can occur remotely as well. 03:16 About half of acute fluid collections resolve on their own, the other half progress on to pseudocyst. 03:23 So let's take a look at the findings associated with a pseudocyst. 03:27 You see here a very large cystic collection that extends inferiorly from the pararenal space down to the left groin. 03:35 Pancreatic abscess can also develop and has a similar appearance to a pseudocyst but usually has a very thick wall. 03:42 So this is again as we go further down in the abdomen. 03:45 This is an axial CT image that's almost near the pelvis and you can see the extent of the pseudocyst all the way down near that pelvis. 03:52 So pancreatic necrosis, this is also a very important finding because as the pancreas becomes necrosed it can then become infected. 04:00 So you really wanna be able to identify this. 04:02 It's identified by lack of enhancement of a portion of the pancreatic parenchyma and that's what the necrosis is. 04:08 So the pancreas should normally enhance on a post contrast image but when it doesn't, as you see in this image here, then you have pancreatic necrosis. 04:15 Here is normal pancreas and you could compare that with the abnormal pancreatic tissue that's right here. 04:21 This may become hemorrhagic as well and it may become infected. 04:27 So again it's very important to recognize this early. 04:30 So what do we see on this image? We have this arrow pointing to an abnormality within the upper abdomen. 04:37 You can see a lot of inflammatory chain surrounding these region. 04:40 So this slice is taken slightly below the level of the pancreas, so we don't see the actual pancreas but we do see this abnormality right here. 04:48 It's kind of a well circumscribed hyperdense structure. 04:52 This is a pseudoaneurysm. 04:55 So the enzymes that are released during pancreatitis can erode the surrounding vasculature and that's what result in pseudoaneurysm formation. 05:02 The splenic artery is the most commonly involved and that's what we see in this case. 05:05 And this can actually rupture and cause life threatening bleeding. 05:08 So again when a CT is done looking for abnormalities associated with pancreatitis, it's very important to look for pseudoaneurysms. 05:15 This is an example of a celiac artery angiogram. 05:21 So pseudoaneurysm can be treated using angiography. 05:26 This patient has severe pancreatitis and the patient had an upper GI hemorrhage. 05:30 So you can see this angiogram demonstrates a pseudoaneurysm of the gastroduodenal artery. 05:36 So you can see that right here where the arrow is and it's a little out pouching that you see. 05:40 So normal vessels on the angiogram should look very linear like this. 05:43 When you see an outpouching similar to this, then this is a pseudoaneurysm and this is what they look like. 05:48 So the interventional radiologist can actually place coils into the pseudoaneurysm and that completely occludes the pseudoaneurysm and can stop the bleeding. 05:56 And you can see here there's coils in this region and this is what they look like. They are actually metallic coils but we don't actually see them in the angiogram because it's a subtracted image so it's subtracts out the metal so we can see the rest of the structures but you can see that the pseudoaneurysm is no longer present. 06:11 Chronic pancreatitis is the chronic inflammation of the pancreatic parenchyma. 06:15 It results in fibrosis and it results in pancreatic atrophy and this is best evaluated by a contrast enhanced CT as well, very similar to acute pancreatitis but the findings are different. 06:26 So some of the imaging findings of chronic pancreatitis include multiple course calcifications, pancreatic gland atrophy and ductal dilatation. So let's take a better look at these. 06:39 So this is an example of a patient that comes in with chronic pancreatitis. 06:44 This is a contrast enhanced axial CT image and you can see multiple course calcifications within the pancreatic parenchyma right here. 06:52 On this image you can also see the pancreatic duct which is the low density linear area within the pancreas is actually dilated. 06:59 So normally you shouldn't really see the pancreatic duct on a CT. 07:02 If you do see it, then there's a suggestion that it's dilated and in this patient we do see it well and the duct is dilated and it's associated again with the surrounding coarse calcification. 07:12 So let's move on to pancreatic adenocarcinoma. 07:18 Pancreatic adenocarcinoma is a very important cause of pancreatic malignancy and it often presents at a stage when it's not resectable. Because of this, it has a very poor prognosis and the majority of these are located within the pancreatic head. 07:32 So what are some risks factors of pancreatic adenocarcinoma? Chronic pancreatitis is actually one of them as is alcoholism, and smoking, diabetes is another risk factor with a low association, family history again is another risk factor of pancreatic adenocarcinoma and any other type of hereditary condition can also be associated with it. 07:55 This is also best evaluated on multiphase abdominal CT so usually we perform multiple phases of a post contrast examination. 08:04 MRI can also be performed if you need further clarification of the extent of disease but usually CT can provide a good idea of what's going on. 08:13 So some of the imaging findings of pancreatic adenocarcinoma include a focal low density pancreatic mass that can be very subtle and difficult to see. Again ductal dilatation is a common feature because the mass obstructs the pancreatic duct and results in the dilatation of the duct. 08:30 And you can also see enlarged lymph nodes that are surrounding the pancreas and again this would be due to metastatic disease in the lymph nodes. 08:37 So here's an example of a pancreatic adenocarcinoma, so we have a coronal CT image and we have an axial that's going to follow which I'll show you in a second. 08:46 It demonstrates a very poorly enhancing mass in the pancreatic head which is right here. Again, somewhat difficult to see. 08:55 The soft tissue density actually appears to be invading the duodenum which is just adjacent to it right here. 09:02 And you can see here that it obstructs the pancreatic duct which looks dilated right here. And this is the axial CT image that we're looking at right now. So let's take a look at a case. 09:12 This patient is presenting with abdominal pain. 09:15 Are there any relevant clinical questions that you would like ask this patient? Let's take a look at this enlarged image. 09:23 You can take a pause, take a good look at it. 09:26 And then see if there's anything that you would like to ask this patient. 09:36 So the patient reports that they drink one bottle of whiskey per day. 09:41 Does that help you at all? So let's take a look at the findings again. 09:48 Again hit pause, take a good look at this image and see what you can find. 09:51 There are multiple findings associated with the pancreas here. 10:01 So the pancreas is enlarged. 10:04 There's peripancreatic fat stranding as you can see all around here. 10:08 There are calcifications within the pancreatic tail and there's a fluid collection that's adjacent to the pancreatic tail right here. 10:18 So a variety of different findings. 10:20 And it's a patient that drinks a lot of alcohol. 10:24 So these findings are all associated with acute and chronic pancreatitis. 10:28 So this is a combination of what we've talked about today. 10:30 We've talked about findings of acute pancreatitis and we've also talked about findings of chronic pancreatitis but it's good to keep in mind that a patient who drinks regularly or who has other risks factors associated with pancreatitis may have a combination of both. 10:43 They may have repetitive attacks of pancreatitis that can result in findings associated with chronic pancreatitis but then also come in with about of acute pancreatitis and this is an example of that.
About the Lecture
The lecture Pancreatic Abnormalities by Hetal Verma, MD is from the course Abdominal Radiology. It contains the following chapters:
- Acute Pancreatitis
- Chronic Pancreatitis
- Pancreatic Adenocarcinoma
Included Quiz Questions
Which of the following is an accurate statement about acute pancreatic fluid collections?
- They may resolve spontaneously
- They develop about four weeks after the onset of pancreatitis.
- They are encapsulated by a fibrous wall.
- They can occur remotely from the pancreas
- They can result in pancreatic necrosis.
A 52-year-old man presents to the emergency department with complaints of abdominal pain which started gradually, now reaching 8/10 in intensity. Past medical history reveals a similar episode a year ago. The patient has a chronic history of heavy alcohol consumption. A CT scan of the abdomen reveals ductal dilatation, peripancreatic inflammatory changes, and diffuse enlargement of the pancreas. What is the most likely diagnosis?
- Acute pancreatitis
- Pancreatic carcinoma
- Pancreatic abscess
- Choledocholithiasis
Which of the following is NOT a complication of acute pancreatitis?
- Cholelithiasis
- Acute fluid collection
- Necrosis
- Abscess
- Pseudoaneurysm
Which statement helps to differentiate a pseudocyst from an acute fluid collection?
- A pseudocyst has a fibrous wall.
- A pseudocyst usually develops within 48 hours after the onset of acute pancreatitis.
- A pseudocyst resolves spontaneously.
- An acute fluid collection never resolves on its own.
- A pseudocyst contains hemorrhagic fluid.
Which blood vessel is most commonly damaged resulting in pseudoaneurysm?
- Splenic artery
- Portal vein
- Hepatic artery
- Short gastric artery
- Pancreaticoduodenal artery
What CT scan finding suggests pancreatic adenocarcinoma?
- A poorly enhancing mass in the pancreatic head
- Fluid collections adjacent to the pancreatic tail
- Cystic lesion in the pancreatic head
- Pancreatic gland atrophy
- Inflammatory changes in the periphery of the pancreatic head
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
good and very very goood and thanks i wish i meet you some day