Playlist
Show Playlist
Hide Playlist
Other Primary CNS Tumors
-
Slides 08 Tumors of the CNS Neuropathology II.pdf
-
Download Lecture Overview
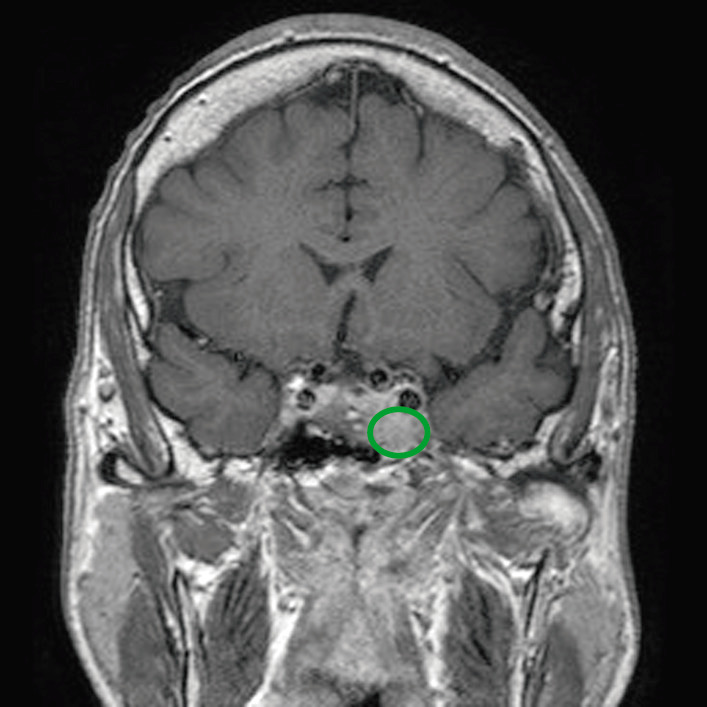
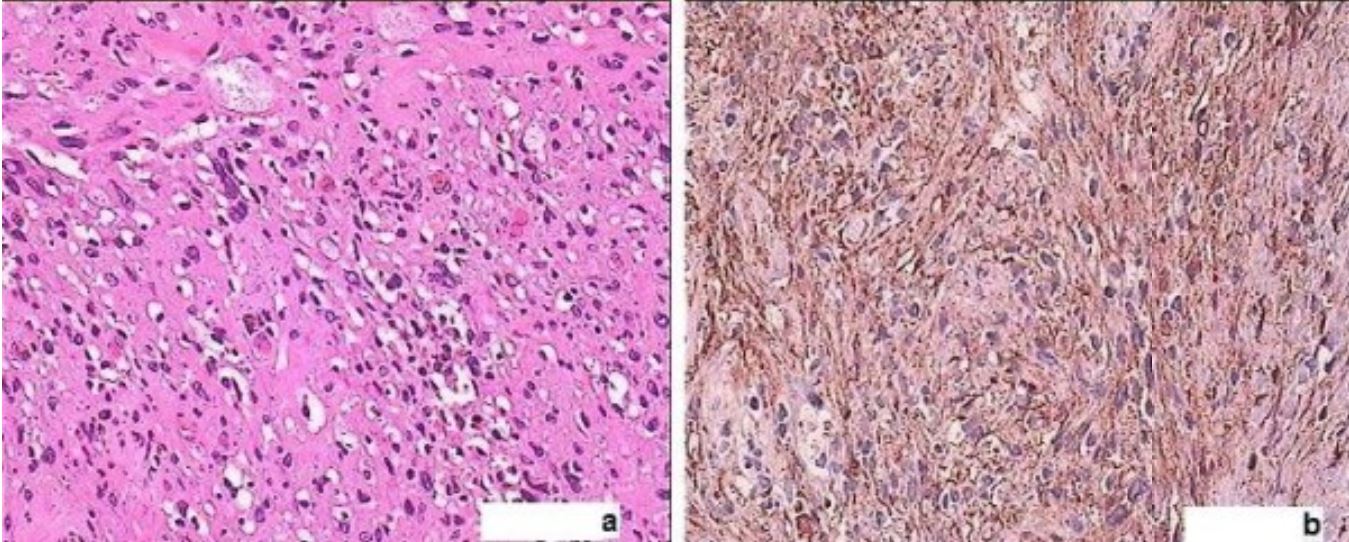
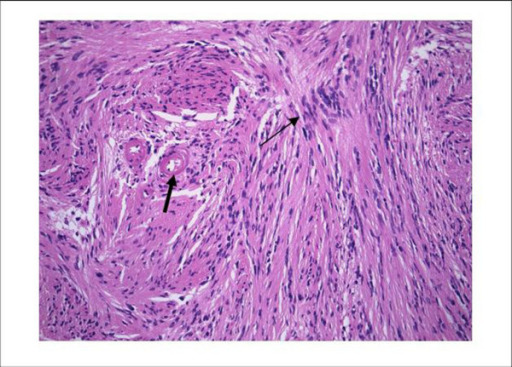
00:02 At this point, the classification we’ll take a look at is primary CNS lymphoma. 00:08 It’s the first time that we’re dealing with a lymphoma in the brain. 00:12 The classification thus far that we’ve walked through have been primary CNS tumors including our astrocytomas, under the category of neuroepithelial tumors. 00:23 And then after astrocytomas, we walked through oligodendrogliomas, ependymomas and so forth. 00:29 So here we have a lymphoma. 00:31 Accounts for 1% of intracranial tumor. 00:33 1%. 00:35 Most common CNS in what kind of individual? Think about an HIV patient or in other words, immunocompromised patient. 00:42 That’s extremely important. 00:44 In fact, we have perhaps even diffuse large B cell lymphoma that may be taking place in your CNS. 00:52 And if you remember from WBC pathology that whenever you talk about lymphomas, you’re dividing this into Hodgkin’s and non-Hodgkin’s. 01:00 And under non-Hodgkin’s, if you remember, those are the ones that love to actually be extranodal. 01:06 You’ll have high-grade B cell neoplasia. 01:09 Once again, diffuse large B cell lymphoma is something that could be found in these immunocompromised patients. 01:17 Our topic here, ladies and gentlemen, is a primary CNS tumor. 01:22 But this is of the lymphoma variant, a major clinical pearl here is, think, HIV or immunocompromised patient, unfortunately. 01:35 The clinical features of your lymphoma: Deep gray structure and white matter. 01:39 Multifocal lesions are common. 01:41 Diffusely enhanced on MRI. 01:45 Diffusely enhanced. 01:47 The reason I say that is because on MRI, you have another description that you want to know in pathology called ring-enhancing. 01:54 But this is lymphoma, so therefore, it’s diffusely enhancing. 01:58 Now, remember, there are different routes of metastasis. 02:03 You could take your hematogenous route, which are mostly likely sarcomas. 02:07 The carcinomas would take the lymphatics. 02:11 With the carcinomas, we’ve talked about a bunch of exceptions. 02:15 And the third route of possible metastasis would be seeding. 02:19 What does seeding mean to you? It means that these neoplastic cells are then metastasizing to the adjacent structure, right? So seeding into the CSF is once again common. 02:31 And we’ve talked about this a few times with seeding. 02:34 For example, I’ll bring this to your attention so that your thoughts are organized. 02:38 The most common brain tumor, primary brain tumor in a child is medulloblastoma. 02:44 There’s every possibility that these small blue cells may then seed into the CSF. 02:50 And glioblastoma multiforme, one of a common adult type of primary CNS tumor may seed into the CSF. 02:59 Is that clear? It can also spread to the eye, this particular CNS lymphoma. 03:05 Well-defined, with central necrosis. 03:08 Treatment is based on the patient's age, comorbidities and their wishes. 03:12 It may include chemo, radiation, stem cell transplants and in cases of palliation glucocorticoids. 03:19 Leave the brain behind and now, we go into the sella. 03:23 Now, normally, what do you have in your sella? We have the pituitary. 03:28 So here, we’ll talk quickly about some pituitary adenomas without going into great detail as to the endocrinology because that has already been covered. 03:35 It may present with endocrine, neurologic manifestation. 03:38 Think about the pituitary gland. 03:40 Think about what you have superior to it. 03:43 And obviously, you are then going to compress the chiasm. 03:46 It may result in bitemporal hemianopsia. 03:49 It may result in headaches, right? May have visual issues, bitemporal issues. 03:54 Most endocrine presentation might be hypopituitarism. 03:58 Be very careful with an adenoma, please. 04:01 What do I mean by that? Because as soon you hear an adenoma, do not think that it’s always going to be functioning. 04:08 You can have an adenoma that is non-functioning. 04:11 And in fact, with an adenoma, whether it be micro or macroadenoma, you really, really want to pay attention to the clinical picture. 04:20 And by that, I mean the following: Microadenomas granted tend to be functioning, that we talked about earlier. 04:26 In microadenoma, if we’re talking about functioning, prolactin might be the most common hormone to then be secreted. 04:33 If it’s macroadenoma, these then tend to be non-functioning. 04:36 And if it’s non-functioning, it may result in hypopituitarism. 04:40 However, even with macroadenomas, you could have a secreting tumor such as a growth hormone, macroadenoma. 04:47 Is that clear? So we talked about this earlier in endocrinology. 04:51 I’m bringing this to your attention once again, the first thing that you always ask yourself is my adenoma functioning or not? And as soon as you have something like a macroadenoma that’s non-functioning, every single hormone will be compromised from the pituitary except prolactin. 05:10 Why? Because this large adenoma might then compress the stalk. 05:16 If you compress this stalk, you’re not able to deliver the dopamine. 05:19 And thus, you’ve increased your release of prolactin. 05:23 I’m not going to review that. 05:24 At this point, you should be well versed with the effect of dopamine, influence of dopamine on prolactin. 05:30 Most common, hyperfunctioning presentation will be excess prolactin as we talked about. 05:35 So therefore, this female, if she has a functioning prolactinoma, she’s going to present with galactorrhea and you know from feedback mechanism, your prolactin inhibits your GNRH, doesn’t it? And so therefore, your prolactin inhibits GNRH. 05:51 She is then going to present with amenorrhea and decreased libido. 05:58 Treatment, obviously surgical. 06:00 You get in there, and try to remove the prolactinoma. 06:02 However, with the prolactinoma, you know that you’re going to use your dopamine agonist, either it be bromocriptine or cabergoline. 06:10 These are dopamine agonist to then halt or control the amount of prolactin being secreted. 06:18 Here, we’ll take a look at acoustic neuroma. 06:21 So what does an acoustic neuroma mean to you? As soon as you hear acoustics, you’re thinking about what? Oh, yeah, hearing. 06:28 And as soon as you hear about hearing, then you should be thinking about what cranial nerve? Eighth, right? Vestibulocochlear. 06:36 It’s not a primary brain tumor. 06:39 Schwannoma of the vestibular branches of the eighth cranial nerve. 06:42 Stop there and make sure whenever you hear the word or description acoustic neuroma, you should be thinking about the cerebellar pontine angle. 06:52 Cerebellar pontine angle and here, you have your bilateral schwannomas. 06:58 And a bilateral schwannoma, in general, would then come from what’s known as a preceding event and that’s called neurofibromatosis type II. 07:08 We’ll talk a little bit more in a second. 07:09 At this point, acoustic, automatically cranial nerve VIII. 07:15 Automatically, thinking vestibular branch of the eighth cranial nerve. 07:20 In terms of location, you’re at the cerebellar pontine angle. 07:24 It’s the most common tumor of the cerebellar pontine angle. 07:27 And here once again, in meningioma perhaps number 2. 07:32 Benign tumors, surgical resection is curative treatment. 07:35 Often presents with unilateral tinnitus or hearing loss. 07:38 Symptoms could be unilateral if you’re affecting the vestibular. 07:42 So look for hearing issues or tinnitus. 07:46 In terms of an acoustic neuroma and where it’s arising from, how many ears do you have? One, two. 07:53 Okay. 07:54 So therefore, an acoustic neuroma would arise from neurofibromatosis type 2. 08:02 A type 2 neurofibromatosis would give rise to an acoustic neuroma, a.k.a., a schwannoma. 08:10 Now, what I’m not going to describe to you but you want to keep in mind is that if at some point in time, you hear about neurofibromatosis type 1, then you’re thinking about giving rise to your neurofibroma. 08:25 With neurofibromatosis type 2, this is then referred to as being your Merlin.
About the Lecture
The lecture Other Primary CNS Tumors by Carlo Raj, MD is from the course Tumors of the CNS. It contains the following chapters:
- Primary CNS Lymphoma
- Sellar Region Tumors: Pituitary Adenoma
- Acoustic Neuroma
Included Quiz Questions
Which of the following is a feature of primary CNS lymphomas?
- Predominantly high-grade B-cell neoplasms
- Predominantly high-grade T-cell neoplasms
- Predominantly high-grade plasma cell neoplasms
- Predominantly high-grade erythrocytic neoplasms
- Predominantly high-grade B-cell and T-cell neoplasms
How does a primary CNS lymphoma appear on an MRI?
- Diffuse enhancement
- Ring-enhancing lesion with a thin cortex
- Ring-enhancing lesion with a thick cortex
- Cystic lesion
- Necrotic lesion
Bitemporal hemianopsia results from compression of which area by a pituitary adenoma?
- Optic chiasm
- Right optic nerve
- Left optic nerve
- Optic tract
- Oculomotor nerve
A 25-year-old man presents with multiple swellings over his body. On examination, there is a loss of hearing in both ears. A diagnosis of acoustic neuroma is made. Which of the following is most likely associated with this condition?
- Neurofibromatosis type 2
- Neurofibromatosis type 1
- MEN 1
- Tuberous sclerosis
- MEN 2
Which of the following associations are correct in the pathology of an acoustic neuroma?
- Eighth cranial nerve and protein merlin
- Eighth cranial nerve and protein neurofibromin
- Tenth cranial nerve and protein merlin
- Tenth cranial nerve and protein neurofibromin
- Eleventh cranial nerve and protein merlin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |