Playlist
Show Playlist
Hide Playlist
OMM: GERD and PUD
-
Slides OMM Gastrointestinal Considerations.pdf
-
Reference List Osteopathic Manipulative Medicine.pdf
-
Download Lecture Overview
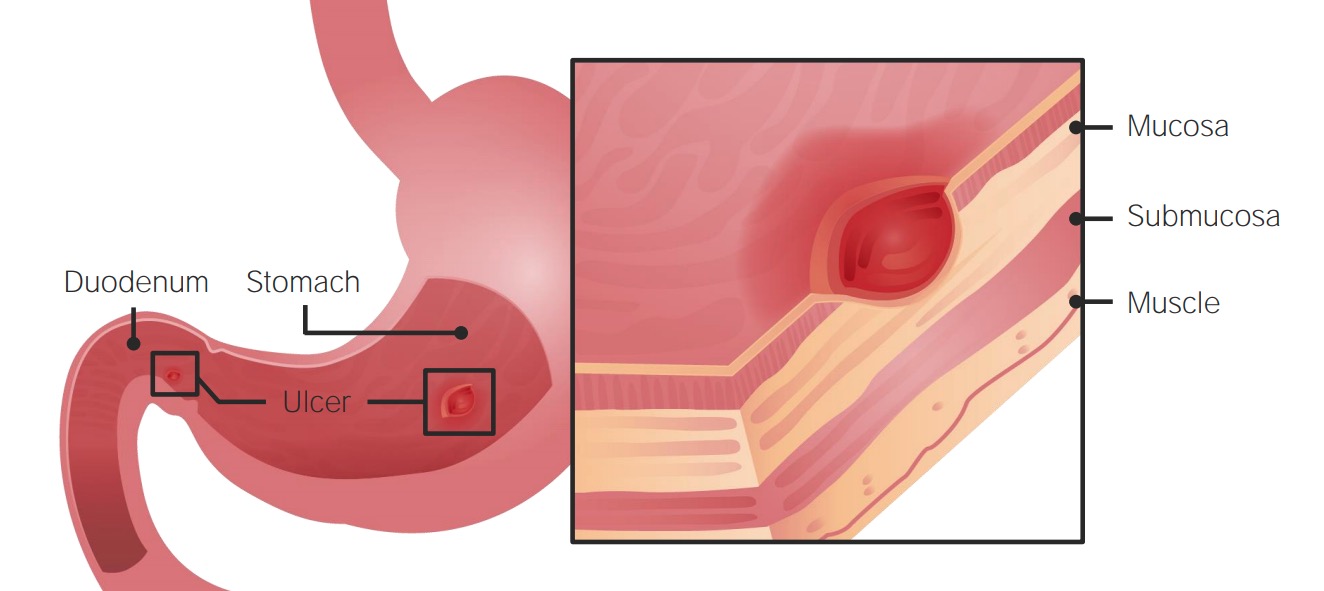
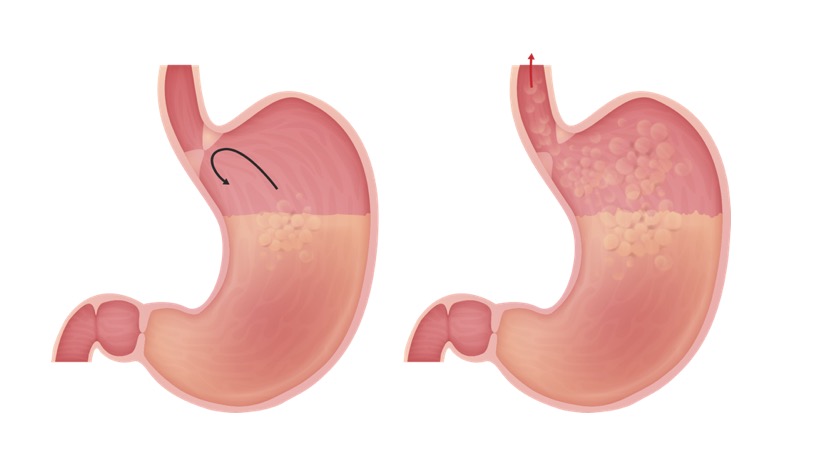
00:00 Gastroesophageal reflux disease is another potential presentation that could be treated with OMM. So, GERD is a motility disorder. The primary symptom is heartburn and is usually due to reflux of gastric contents up from the stomach and into the esophagus. So usually that reflux is due to lack of tone at the lower esophageal sphincter. There are potential causes for decreased tone there. One includes different medications, another includes different foods that might decrease pressure or increase gastric acid secretion. So these are things that we need to take a look at and ask our patients and try lifestyle modifications or discontinue some of these medications to help them potentially with their symptoms. So GERD could cause a lot of different symptoms. 00:53 One of the things to keep in mind is the potential that acid to come up and burn the esophagus causing pain. It could come all the way up to the throat, into the mouth causing irritation of the pharynx thus triggering a chronic cough and bronchospasm. Patients could also have complaints of abdominal fullness, bloating, belching and so there is increased risk for esophageal adenocarcinoma if untreated with prolonged GERD because of that constant burning irritation of the esophageal lining. Peptic ulcer disease is another presentation that is more severe than GERD but similar in etiology. So, peptic ulcer disease is ulceration of the stomach or the duodenum resulting from an imbalance of the mucosal protective factors and also other injuries and damages to the mucosa. So, what happens is you develop an ulcer in the stomach called a gastric ulcer or in the duodenum called a duodenal ulcer. So, duodenal ulcers are more common than the gastric ulcers. There are a lot of different factors that play into it. There are things that potentially decrease our ability to protect the lining. These include H. Pylori infections, NSAID use, steroid use, cigarette smoking and alcohol. So a lot of these different things may potentially be lifestyle changes for the patients or avoidance of difference medications. So the cause of peptic ulcer disease usually lies with either an incompetent pylorus or lower esophageal sphincter, bile acids or impaired proximal duodenal bicarb secretion or sometimes there is decreased blood flow to the gastric mucosa or increased acid and pepcid secretions. So in both GERD and peptic ulcer disease, there are similar osteopathic findings. So again, base your assessment with a thorough history and physical, perform your osteopathic structural exam and check for possible somatic dysfunctions. So areas of facilitation for both GERD and peptic ulcer disease pretty much will reflect around the esophagus. So esophagus is innervated from like T3 to T6 more on the right side, possible stomach reflexes T5 to T10 more on the left side and possible duodenal viscerosomatic reflexes from T6 to T8. So, you want to check for possible viscerosomatic reflexes in this region based on the presentation and the possible organs that are being irritated. So, we want to make sure that we also check for proper functioning of the lymphatic system so that includes looking at the thoracic inlet and the different diaphragms. We want to address parasympathetics and autonomics. So we definitely want to treat and diagnose any somatic dysfunctions of the OA and the upper cervicals for the vagus nerve and the sacrum for the pelvic splanchnics. You want to check for Chapman reflexes. So viscerosomatic reflexes could cause these Chapman reflexes that you could find along the anterior intercostal spaces and so the left 5th intercostal space is responsible for stomach acid and the left 6th intercostal space correlates with stomach peristalsis. So those are 2 regions you definitely should check for the symptoms of GERD. The esophagus is actually the 2nd left intercostal space. The small intestines again are bilaterally in the 8th to 10th intercostal spaces. So again, check for these potential Chapman reflexes and if they are present go ahead and treat them. So make sure to check for postural dysfunctions, muscle and balances, possible somatic dysfunctions along the spine especially at the spinal junctions because those are the regions that correspond with Zink patterns. 04:56 The diaphragm plays a real important role with these presentations. So the right crus of the diaphragm forms a major portion of the gastroesophageal junction and so when we take a breath in, the contraction of the diaphragm actually helps to close the lower esophageal sphincter. So that right crus attaches to the thoracolumbar spine, you also have fascial connections of that region to the right 12th rib so it is important to definitely look at the spine, the rib and all the attachments of the diaphragm in general because any sort of dysfunction in that region could potentially affect the lower esophageal sphincter tone biomechanically. Your sympathetic chain also passes through the medial arcuate ligament.So again, any sort of restriction in the diaphragm could potentially irritate and cause problems with sympathetic innervation. So, treatment for GERD and peptic ulcer disease, again it is important to treat the structural dysfunctions that you find. You want to again treat facilitative segments first. Possible treatments include utilizing the ganglion release technique. So we talked about how the different ganglion innervate different portions of the organs. The celiac ganglion corresponds with the esophagus and stomach and duodenum. So, when you are doing ganglion release you may focus a little bit more just on the celiac ganglion for GERD and peptic ulcer disease. You want to treat Chapman points and then potentially find corresponding counterstrain points that may be associated with the GI tract. 06:40 You could also perform rib raising to address any viscerosomatic, suboccipital release to address vagal tone and again looking at the attachments of the diaphragm and treating the diaphragm directly to remove any somatic dysfunctions in that region will help with GERD and peptic ulcer disease. 06:59 Here is a schematic of the Chapman points that we discussed, stomach acid in the left 5th intercostal space and stomach peristalsis in the left 6th intercostal space. Here are additional upper GI tract Chapman points that you should be familiar with and be able to correlate these viscerosomatic reflexes based on location back to the organ of origin. So let us go into detail on how we perform the abdominal ganglion releases. So remember we utilize these techniques to try to decrease hypersympathetic tone to the gut. So to perform the technique, the patient starts off lying supine, the physician is going to stand to the side of the patient and the physician is going to contact the skin overlying the ganglion with your finger pads. You are going to utilize either one hand over the other when you are applying pressure over a single ganglion or you could target all three ganglion at the same time kind of spreading your finger out so it is right underneath the xiphoid, the bottom hand is going to have the fingers right above the umbilicus and the middle finger is going to be right in between. You are going to gently meet the resistance of the tissue. So when the patient breathes in, you are going to feel resistance into your fingers and when they breath out you are going to follow exhalation. 08:23 So your finger is going to sink in during exhalation, pushing inferiorly towards the table. You are going to repeat until there is softening of the soft tissues. Really as you are pushing down, you should kind of start to get a sense of the pulsations of the aorta. Now if you feel a large pulsatile mass, that would be a contraindication, you would have to double check to make sure that there is no aortic aneurysm but in general your sinking in when the patient exhale of getting the sense of the tension around the tissue and what you will feel is more of a release of that soft tissue.
About the Lecture
The lecture OMM: GERD and PUD by Sheldon C. Yao, DO is from the course Osteopathic Treatment and Clinical Application by System.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |