Playlist
Show Playlist
Hide Playlist
Obstructive Lung Diseases: Diagnosis
-
Emergency Medicine Bord Obstructive Lung Disease.pdf
-
Download Lecture Overview
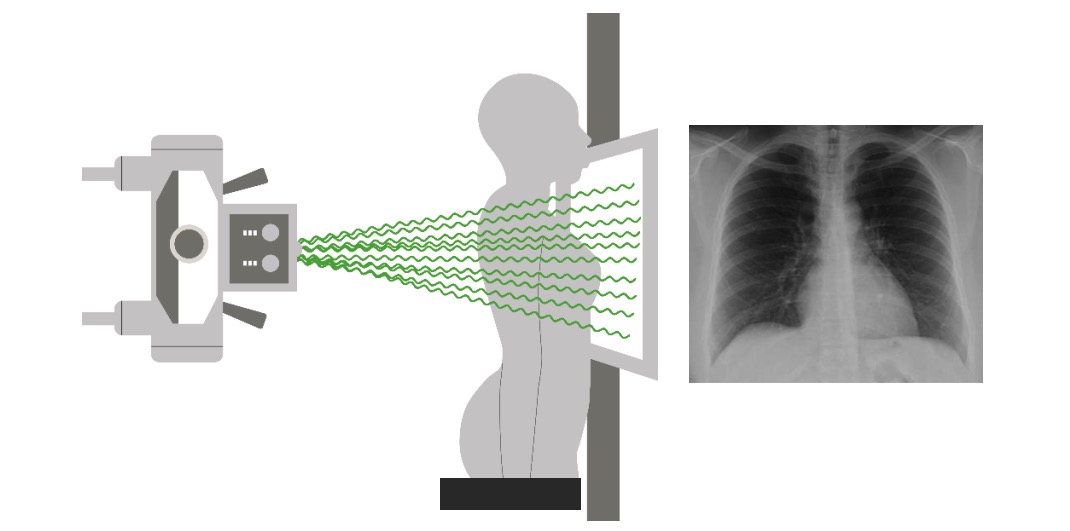
00:01 Now, again, this is often an exacerbation of a chronic problem. 00:04 So someone will come in and say, "I feel like I'm having an exacerbation of my asthma or of my COPD." But in the ED, we always wanna think about our differential of consequence and we always wanna make sure we're thinking broadly because if someone comes in and they say, "This is my asthma exacerbation." Potentially, it may be something else, right? Potentially that maybe a red herring and we don’t wanna close too early for these patients; we don’t wanna automatically just assume that that’s what's going on, we wanna think about other things. 00:33 Now, this is not an exhaustive list here but just to kind of address, pneumonia, is something that could be there so you wanna ask about any other associated symptoms that could point you in that direction. 00:43 Do you have a fever or a cough? Pulmonary embolus is discussed in another lecture, but you wanna ask about potential risk factors and we’ll get more of this in a moment. 00:52 You wanna ask about or think about acute coronary syndrome especially for older people. 00:58 You wanna be checking in EKG and troponin test and be thinking about this as a possible etiology. 01:04 And congestive heart failure is the other thing. 01:07 I mentioned on physical exam, your patient may have wheezing or will likely have wheezing but this is where that cardiac wheeze comes in to play. 01:15 So does your patient have a cardiac related wheeze? And you wanna make sure you're thinking about that and something that can help you is thinking about the patient’s prior medical history. 01:24 So do they have a history of congestive heart failure" And if so, you definitely wanna be thinking about that as a possible etiology of their shortness of breath. 01:32 You know, just taking a moment to think about pulmonary embolism patients with COPD. 01:39 So, like I just said, we don’t wanna close too early on this patients and in a lecture on pulmonary embolus, you could see that it can be a very tricky diagnosis to make. So we wanna make sure that we're thinking about it in our differential diagnosis for patient’s presenting with COPD exacerbation. 01:54 There was this study that highlighted that after 25% of patients who were admitted to the hospital with COPD exacerbation actually had concomitant PE. 02:05 So keeping this on your differential to avoid early closure is very important. I always, whenever I'm taking care of a patient with COPD, I always take a moment to think about whether or not they could have a pulmonary embolus as well. 02:17 Your on initial testing for COPD. The first test you wanna get is the chest x-ray. 02:22 Now chest x-ray can help you take a look at the lungs and it can also help you take a look at the potential other etiologies that could be going on like the pneumonia that we mentioned or the pneumothorax. 02:32 You know the classic chest x-ray finding is that you would have a patient who has larger lung volumes. 02:39 So if generally for a patient, most patients have -- you could see down to a certain number of ribs and COPD patients you will see that their lungs are what we call hyperinflated. 02:49 Additionally, you will see potentially that the patient has flattened diaphragms, that their diaphragms which are normally dome shaped appear to be flat in nature and then the last thing that we sometimes think about is that your patient may have what we call a barrel chest and that would something that you would see on a lateral chest x-ray that the patient has an increase AP diameter on that chest x-ray. 03:09 The other test you get is an EKG. EKG again can help look for other possible etiologies of the patient’s shortness of breath. 03:17 Definitely an EKG for an older patient who's coming in with the COPD exacerbation often times for those young or asthmatic patients an EKG isn't necessarily indicated. 03:27 A chest x-ray actually for the asthmatic patient’s who come in with wheezing and no cough might not necessarily be indicated as well. 03:35 We're gonna talk in a bit about blood gasses but a blood gas can help differentiate in those patients who have severe shortness of breath. What your next steps would be? So does your patient need noninvasive ventilation? Does your patient need nebulizer treatments? And the blood gas can help steer you in one direction or the other. 03:52 Troponin testing for older patients and whom you're concerned about coronary syndromes or potentially even just strain on the heart should be considered. 04:02 And then when we’re thinking about that pulmonary embolus patient possibly a D-dimer maybe indicated for the lower risk patient or on whom a patient who you're concerned about a PE but you considered to be in that lower risk category and that’s’ a screening test for the pulmonary embolus. 04:19 When thinking about blood gasses, the blood gas can be used to both tell whether or not the patient has oxygenation issues as well as ventilation issues. 04:31 Arterial blood gas can tell you both of those things. It can look at oxygenation and ventilation. 04:37 But it can be painful for a patient and can be a little bit challenging to obtain. 04:41 For the most part in the emergency department we get venous blood gasses. 04:45 A venous blood gas can be sent off with the rest of the blood work that’s obtained when an IV is placed or when a venous blood draw takes place. 04:51 And then the venous blood gas it actually does a really good job at looking at the pH as well as the carbon dioxide levels the PCO2. 05:00 In asthmatic patients, we always wanna think about when we're interpreting our blood gases whether or not we should be concerned, if we draw venous blood gas on a patient and they have a normal pH and a normal carbon dioxide level in a patient presenting with asthma exacerbation. 05:16 Now in order to talk about this, we need to understand a little bit about physiology and I understand that when a patient is presenting with an asthma exacerbation, they will have an increase respiratory rate. 05:28 And when you have an increase respiratory rate, what's gonna happen to your carbon dioxide levels? They're gonna go down, right? So in a patient who has a normalize blood gas, so a pH of approximately 7.4 and a PCO2 level of about 40, you should actually start to be concerned in a patient with a moderate to severe asthma exacerbation. 05:48 This may indicate that the patient is tiring out and in need of ventilator support. 05:53 So a patient with a normalize blood gas actually you would think she'd reassure you, it should make you feel pretty good, it’s normal, right? Really, in reality, that patient may need additional assistance because they may be tiring out, they may not be able to keep up with the responsible rate. 06:10 Now, the blood gas in patients with COPD can be a little bit tricky to interpret as well. 06:15 Patients’ with COPD generally chronically retains CO2 due to their underlying pulmonary changes. 06:21 So in those patients they may have a baseline elevated carbon dioxide level so their carbon dioxide level for a normal person is 40, but in a person with COPD it may be around 70, 80 and somewhere in that range, potentially 60. 06:37 So for those patients, overtime, cuz keep in mind this is a chronic problem our bodies compensate. 06:45 And the body compensates by our kidneys reabsorbing more bicarbonate level so when we reabsorb more bicarbonate it kind of creates this pH balance. 06:55 So with those patients you wanna look in conjunction at their pH as well as their PCO2 level. 07:01 And when in acute exacerbations what potentially might happen is that PCO2 level may get even higher and the pH level will get lower. 07:09 It’s hopeful in these patients to sometimes have a baseline blood gas so you know where they normally live but looking at that pH in conjunction with the PCO2 is the key for these patients because their original level and there baseline levels not in the state of exacerbation will not be normal usually. 07:28 So it’s helpful to compare the blood gases to priors for patients with COPD.
About the Lecture
The lecture Obstructive Lung Diseases: Diagnosis by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
Which disease was noted to be concomitantly present in up to 25% of patients presenting with an apparent COPD exacerbation?
- Pulmonary embolism
- Pulmonary tuberculosis
- Sarcoidosis
- Allergic rhinitis
- Heart failure
What should be the first test to order in a patient with COPD exacerbation?
- Chest x-ray
- EKG
- Blood gases
- Troponin
- D-dimer
What finding in a lateral chest x-ray suggests COPD?
- Increased anteroposterior (AP) diameter
- Retrocardiac shadow
- Consolidation
- Retrosternal opacification
- Lobar collapse
What is the physiological effect of an increased respiratory rate on the carbon dioxide level in a blood gas analysis?
- Decrease in carbon dioxide
- Slight increase in carbon dioxide
- No change
- Doubling of the carbon dioxide level
- Tripling of the carbon dioxide level
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |