Playlist
Show Playlist
Hide Playlist
Neuroleptic Malignant Syndrome and Catatonia
-
Slides Pharmacology Antispychotics.pdf
-
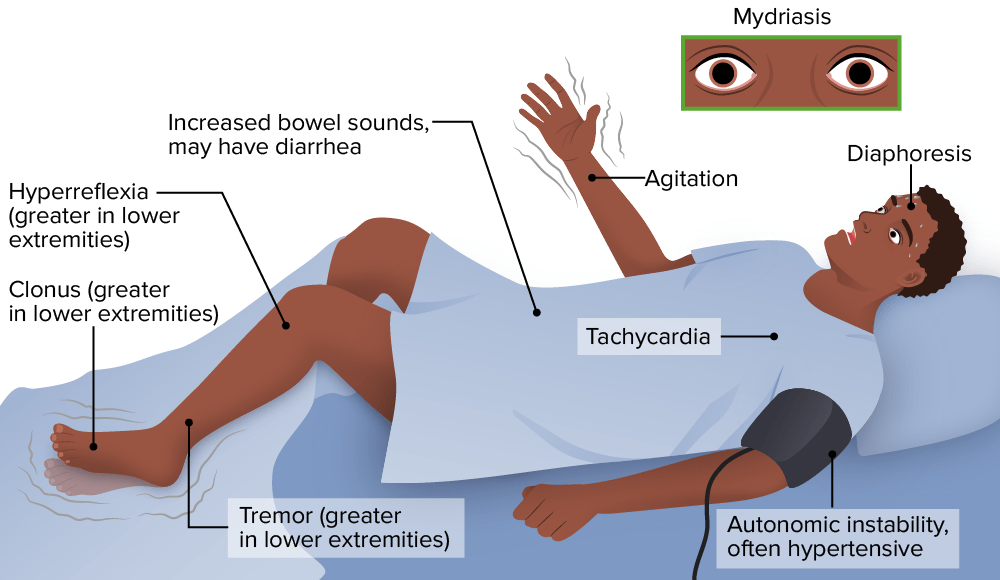
Download Lecture Overview
00:00 Now, neuroleptic malignant syndrome is a very noteworthy side effect coming from antipsychotics. 00:07 So this is life-threatening. It’s characterized by a fever, altered mental status, muscle rigidity, and autonomic dysfunction. 00:16 This often can occur on exams, so let’s take a moment to talk about it. 00:20 It’s more common in males. In fact, probably most common in young African American males in their 20s. 00:27 Although it’s a significant side effect, thank goodness, it is rare but still important to know about, especially on exams. 00:34 And it’s a true medical emergency that can in fact lead to death. 00:38 So in your assessment, what you’re going to look for when determining whether or not somebody has neuroleptic malignant syndrome. 00:46 Well, before they actually will develop the syndrome, it’s usually preceded by the patient being in a catatonic state. 00:54 Then they’ll develop a fever, instability like tachycardia, blood pressure changes, and they'll be sweating profusely. 01:02 They may have a leukocytosis, a tremor, elevated CPK, and also rigidity. 01:08 Fever and rigidity are really the two hallmarks of NMS that you want to be looking for. 01:14 So they may also have muscle spasms, trouble swallowing. 01:19 They may have some parkinsonian symptoms, and sustained motion or restlessness. 01:25 They may have uncontrollable repetitive movements. 01:29 We already mentioned the fever, rigidity, unstable vital signs. And you’re looking for blood work that shows a high CPK, high potassium, and elevated white blood cells. 01:38 So there's a lot of different ways to treat the patient with NMS. 01:42 You're probably gonna be thinking of doing something like beta blockers, benzodiazepines, of course, stop the offending agent. 01:49 Treat them with Dantrolene, cool them, and give them IV hydration and fluids. 01:53 And consider switching to atypical agent or newer antipsychotic. 02:00 Something important to note is that unlike what many people think, NMS is not actually an allergy to a medication. 02:07 It’s a very adverse and bad reaction, but it doesn’t mean that somebody can never take an antipsychotic again or try different antipsychotic later. 02:17 You simply want to treat the emergency, let the patient stabilize, and it’s actually okay to slowly introduce an antipsychotic in the future. So NMS is not an allergy. 02:28 Catatonia is a behavioral symptom that is diagnosed in patients who are ill with an underlying psychiatric and or general medical disorder. 02:39 It requires the presence of at least three of the following stupor a decreased psychomotor activity or decreased reactivity to the environment. 02:50 Number two, cataplexy passively allowing the examiner to position the body or a part of the body. 02:58 Waxy flexibility, a slight even resistance to positioning by the examiner as inventing a candle. 03:06 Mutism. Lack of verbal response. 03:09 Not applicable to patients with an established aphasia and negativism. 03:15 Motive was to resist ance to instructions or external stimuli. 03:19 Posturing. 03:21 Voluntarily maintaining a position of the body or a body part against gravity for a long time. 03:29 Mannerisms which are odd. 03:31 Movements stereotyped, which are repetitive. 03:36 Movements that are not goal directed and are often awkward or stiff. 03:41 Agitated or excessive motor activity that is purposeless and not influenced by external stimuli. 03:49 Grimacing Echo Lilia which is the mimicking of another person's speech. 03:55 Echo Proxy to the mimicking of another person's movements.
About the Lecture
The lecture Neuroleptic Malignant Syndrome and Catatonia by Helen Farrell, MD is from the course Schizophrenia and Thought Disorders.
Included Quiz Questions
Which of the following statements regarding neuroleptic malignant syndrome is FALSE?
- It is a life-threatening reaction to tricyclic antidepressants.
- Autonomic dysfunction is often seen including diaphoresis, tachycardia and tachypnea.
- The patient can have altered mental status.
- It is more common in African American males.
- Hyperthermia often beyond 38 °C/100.4 °F and severe muscular rigidity are seen.
Which of the following options are therapeutic options for the management of neuroleptic malignant syndrome?
- IV fluids, cooling, and Dantrolene
- Dantrolene, Benzodiazepines and heating pads
- IV fluids, anticholinergics and high potency D2 blockers
- β-blockers, cooling and Cholinergic agents
- IV fluids, high potency D2 blockers and β-blockers
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The title is quite misleading. I would recommend to split the part with neuroleptic malignant syndrome & atypical drugs for better functionality. However, the content is great
1 customer review without text
1 user review without text