Playlist
Show Playlist
Hide Playlist
Endocarditis: Microbiologic Dx
-
Slides InfectiveEndocarditis InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
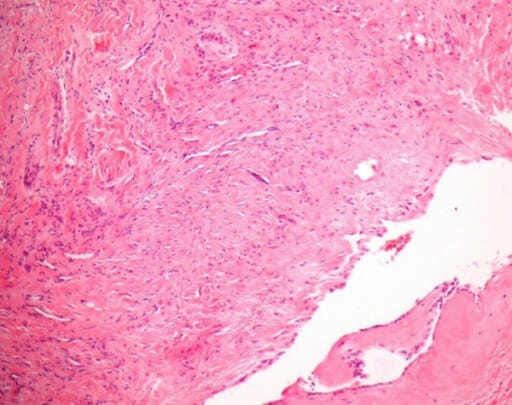
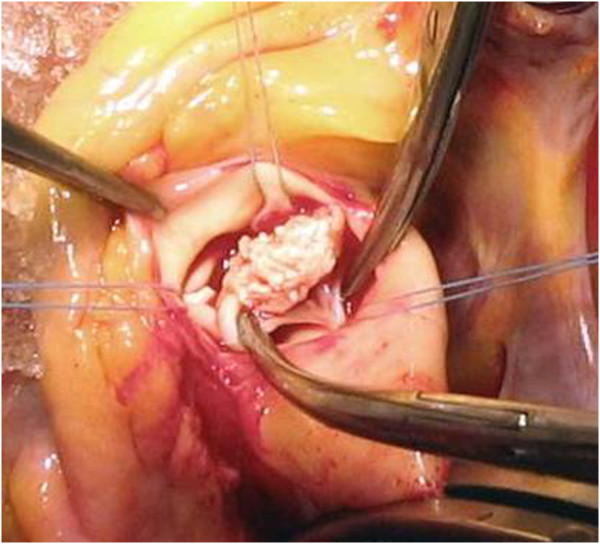
00:00 So, how do you make a microbiologic diagnosis? Draw blood, draw blood cultures. You always draw at least three and ideally before any antibiotics have been given. Now, let’s say a patient got antibiotics 24 hours before you saw the patient and let’s say they are stable. They don’t have heart failure. 00:28 They don’t have any major problems. Can you wait a couple of days and draw some more blood cultures before you treat? The answer is yes, you probably can. Nowadays, we’re moving to faster treatment of patients empirically. But if the patient is stable and is not sick but has fever, you can work up the cause of that fever and that would include blood cultures. But anyway, you would never get a single blood culture. The reason you wouldn’t get a single blood culture is what if it’s positive? Well, how do you know that it wasn’t some kind of procurement contaminant because somebody didn’t disinfect the skin adequately. Maybe you’re dealing with a skin bug that just contaminated your blood culture media? So the control for that is to get several blood cultures. For endocarditis, at least three so that in endocarditis, all blood cultures should be positive if antibiotics aren’t in the pie. 01:37 So, you would expect more than 90% of the blood cultures for common organisms to yield a positive result. There are some series that say blood cultures are negative in up to 31%. 01:54 I’m not certain about that. That’s just what is written. Now, what about these fastidious organisms? The main way we diagnose those is through serology. That includes Coxiella burnetii. 02:17 That includes Brucella, Bartonella, and Chlamydia, as well as Mycoplasma pneumoniae. 02:28 These are hard to demonstrate that they cause endocarditis. So, what we do is when we have a patient we think has endocarditis, we go ahead and get this serologic test cooking because some of them have to be sent off to other laboratories. So, why wait for several days to find out that your blood cultures are negative? Meanwhile, there’s been a delay in diagnosing these. So, we send these off so that the turnaround time is more rapid for the patient. We can get them on appropriate therapy if that’s what they turn out to have. Now, for the cerebral complications, if we suspect those, we would get an MRI. That’s the best confirmatory test. We can demonstrate cerebral abnormalities in about 80% of individuals with infective endocarditis. Now, exactly what they mean without having symptoms, I’m not certain. But we definitely can find them. About 50% of patients get embolic events because after all, that’s what these vegetations are releasing organisms into the entire circulatory system. So, you shouldn’t be surprised about that. But most of the time, they’re asymptomatic. But the MRI is the best confirmatory test. Now, what about these cardiac devices? Let’s say you suspect an infection in a defibrillator or in a pacemaker, should you take it out? That’s a big question. It costs a lot of money to put this thing in. You don’t want to just say, "Oh, well, just take it out." No. Removal would be recommended if you demonstrate a definite lead infection. 04:31 That’s got to come out because it’s not going away unless you pull the leads; or if a patient presents with sepsis, obviously very sick and they have a pacemaker in or a defibrillator. You would definitely remove those because if they’re not the cause of the infection, they probably will become infected with the sepsis. Let’s say the pocket in which the defibrillator sits has got a definite infection and the device is surrounded by pus, it’s got to come out and so did the leads because the leads that go to the heart are very likely infected. If you’ve demonstrated that the valves are infected but you haven’t demonstrated that the wires are infected, you should assume that the wires are infected and take the device out. Let’s say you’ve got a pacemaker in a patient who doesn’t have vegetations on the heart valve but they have positive blood cultures for staphylococcus. So, they’ve got a bad bug in their bloodstream and they’ve got one of these devices in. Take it out. If they have persistent occult gram-negative bacteremia, the reason for that is that gram-negative rods and gram-negative organisms easily can cause sepsis. So, if they’re not causing it when you see the patient, if you don’t remove those devices, they may soon get septic on you. Let’s say the device has just been put in. Now, they’ve got a little, tiny infection in the wound. You don’t necessarily have to pull it. Simply, treat the wound infection and observe the patient closely. That would be a superficial skin infection above the pocket site. 06:45 So, just because you have a little bit of stitch abscess around the site doesn’t mean you have to pull the entire device. You certainly should do a Gram stain and culture of any pocket abscess and also the lead tips. Those lead tips can actually be rolled on an agar plate to see what organisms might grow. 07:12 What about various kinds of imaging? The classic would be echocardiogram. What is often performed first is a transthoracic echocardiogram because it’s less invasive. It’s not as good as a transesophageal echocardiogram in general. It’s not as good. But it may be better to enable you to see anterior abscesses in a prosthetic aortic valve. But if I start talking like an expert on echocardiography, you’ll probably go away because I’m an infectious disease specialist. I’m not going to pass myself off as an echocardiographer. 08:05 But suffice it to say that the TEE has greater sensitivity and specificity and should be done in everybody who’s got infective endocarditis. It certainly should be done if the TTE is negative or of poor quality or if they have an intracardiac device. In general, a TEE should follow up even an abnormal TTE. 08:35 It’s recommended to do combined when you have any kind of vegetations, when you have any kind of valve regurgitation, a valve abscess, when a prosthetic valve is dehiscing, when it seems to be rocking or not stable and in an obvious paravalvular abscess. It’s good to have both TTE and TEE. 09:04 So, how do you definitively diagnose infective endocarditis? Well, the literature would say that you use the modified Duke criteria. So, let’s go through these and then I’ll have a comment about them. 09:23 The major criteria would be a positive blood culture times two of viridans strep, Strep, gallolyticus one of the HACEK organisms, Staph aureus, or enterococcus. It would be another major criterion to have persistently positive blood cultures, or any blood culture positive for Coxiella burnetii, the cause of Q fever. More major criteria would include evidence of endocardial involvement. 10:02 Here, we’re talking about an oscillating mass on the valve leaflet, positive echocardiogram. 10:10 The minor criteria would be some kind of predisposing heart condition or IV drug use. 10:20 The patient, along with that, has fever usually greater than 38, vascular phenomena such as those Janeway lesions, immunologic phenomena. I ought to mention right now that immune complex glomerulonephritis is one of the findings occasionally in patients with infective endocarditis usually due to low-virulence organisms where the diagnosis is delayed; or microbiologic evidence that does not quite meet major criteria, didn’t have persistent positive blood cultures but they had positive blood cultures. Then of course, definite would be pathologic criteria. 11:12 You find microorganisms in a vegetation. You have pathologic lesions on valves. Definite clinical criteria would be two major or one major and three minors or 5 minors. Possible endocarditis will be one major, one minor, or three minors. Now, why go through all these? Well, it certainly helps you understand infective endocarditis a little bit better. But let me say that this is not usually what clinicians use at the bedside. This is what researchers use to study the various outcomes and treatment for endocarditis. So, if you wanted to prove, let’s say Wondercillin was effective in endocarditis and you want to test a hundred patients, well, you’ve got to say whether they had proven or possible endocarditis. Do you see what I’m getting at? In other words, these kinds of criteria are useful for categorizing the patients that you’re studying. So, it’s mainly for research purposes that we use the Duke criteria. Are they testable? I’m not really certain whether they would test you about possible being one major and one minor or three minor. That seems to me to be outside the purview of step exams. But they’re available for you if that’s what you want to use them for.
About the Lecture
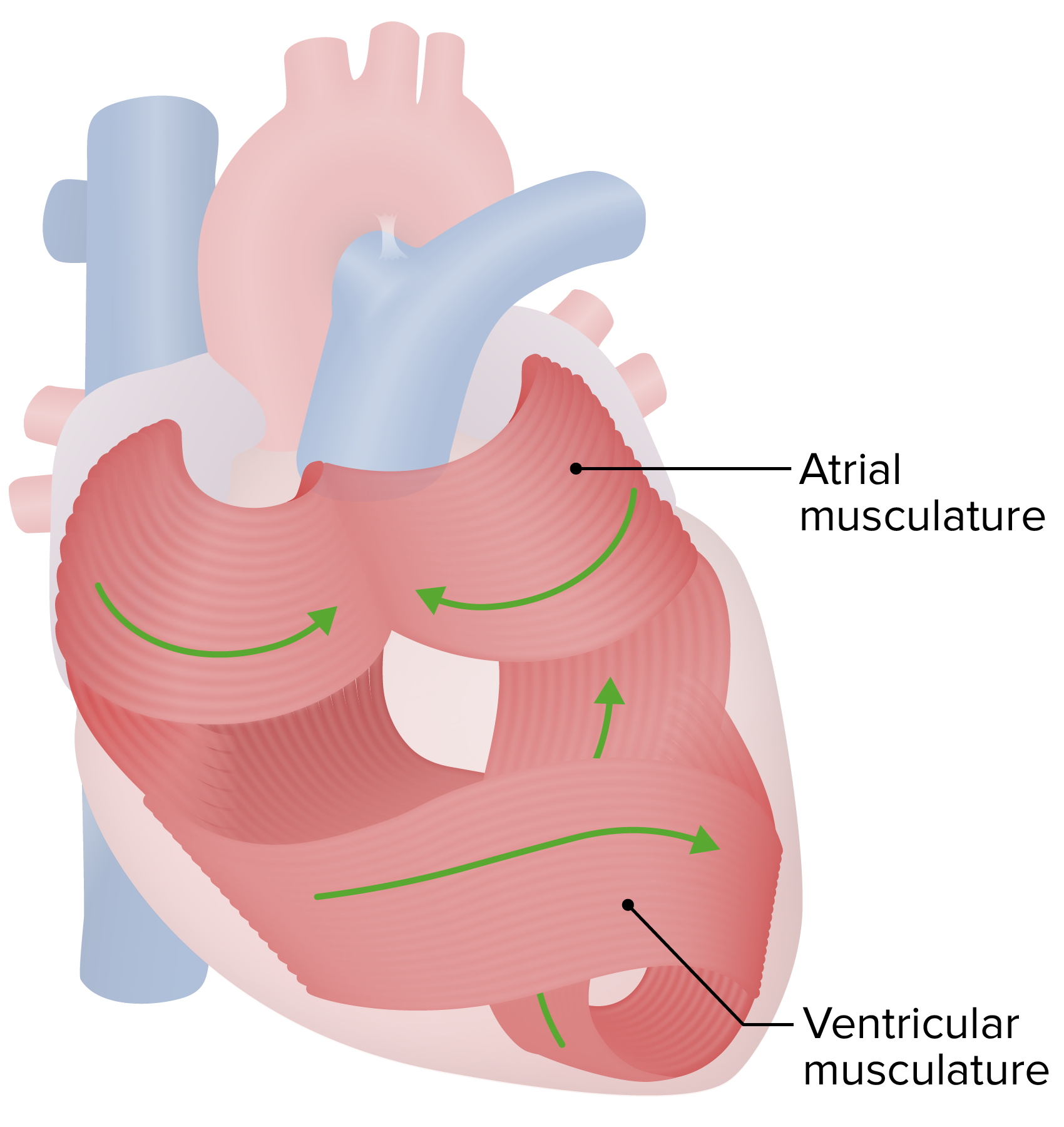
The lecture Endocarditis: Microbiologic Dx by John Fisher, MD is from the course Cardiovascular Infections. It contains the following chapters:
- Diagnosis – Microbiologic Dx
- Overall Dx of IE — Modified Duke Criteria
Included Quiz Questions
At least how many blood culture specimens should be negative before making a diagnosis of culture-negative infective endocarditis?
- 3
- 1
- 2
- 4
- 5
Which of the following most strongly indicates cardiac device removal in a patient suspected of having infection of cardiac implantable electronic devices?
- High-grade bacteremia with coagulase-negative staphylococci
- Fever greater than 38°C
- No device manipulation over the past three months
- Superficial cellulitis with no involvement of the generator pocket
- New murmur
Which of the following imaging studies has the greatest sensitivity and specificity for infective endocarditis?
- Transesophageal echocardiography
- Transthoracic echocardiography
- Cardiac magnetic resonance imaging
- Chest CT scan with and without oral and intravenous contrast
- Chest x-ray
Which of the following organisms should be suspected if cultures are negative during the workup of infective endocarditis?
- Coxiella burnetii
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus mutans
- Streptococcus sanguinis
Which of the following is not a major criteria on the modified Duke criteria for endocarditis?
- Single positive blood culture for Staphylococcus aureus
- Persistently positive blood cultures
- Single positive blood culture for coxiella burnetti
- Vegetations seen on echocardiography
- Typical microorganisms consistent with IE from two separate blood cultures
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |