Playlist
Show Playlist
Hide Playlist
Meningitis and Encephalitis: Diagnosis
-
Emergency Medicine Bord Meningitis and Encephalitis.pdf
-
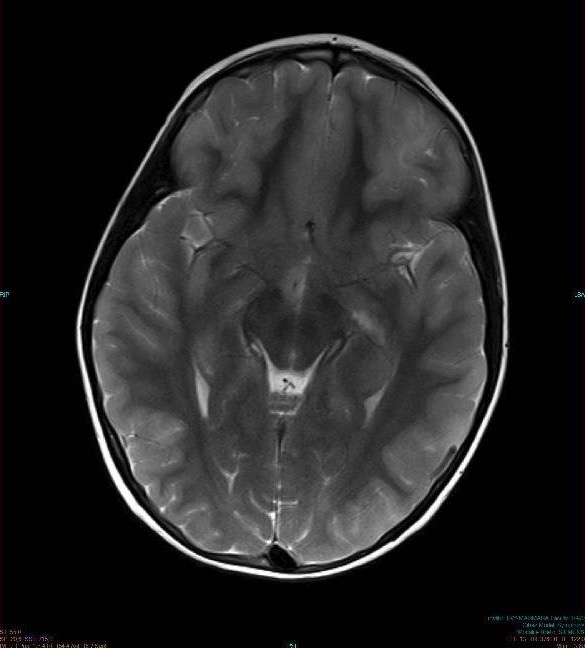
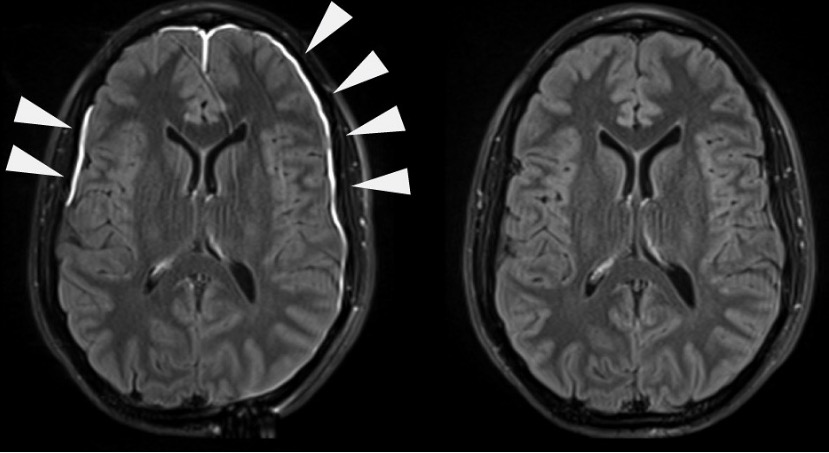
Download Lecture Overview
00:01 So how do we evaluate these patients? Key things are, especially when you’re worried about bacterial meningitis is you wanna get your work up done as quickly as possible. 00:10 Because we know that the sooner that patient gets antibiotics the better off they’ll do. 00:15 Now often times, we do start with some basic lab testing, so a CBC, an electrolytes. 00:22 Then you wanna consider checking blood cultures in a febrile patient, especially if you’re worried about meningitis. 00:27 And those don’t necessarily give you information immediately but they can help down the line if the patient is admitted to the hospital or when they’re admitted to the hospital. 00:38 Lumbar puncture is gonna be your test here that’s gonna give you the answer. 00:41 It’s gonna be the test that's gonna tell you whether or not your patient has meningitis. 00:45 So for the most part, almost every patient in whom there is concern for CSF infection should get a lumbar puncture. 00:51 Now one thing you wanna make sure you do is you wanna make sure that you — that you start thinking about whether or not your patient has elevated intracranial pressure. 01:02 Now elevated intracranial pressure is a contra-indication to doing a lumbar puncture. 01:07 So for the most part, a majority of patients can actually get an LP if they are able to get a look at the back of their eye and not see any papilledema before without getting any neuro imaging. 01:21 Now there are a certain subsets of patients and this is debated in the medical community, who should most likely get a head CT before they get a lumbar puncture. 01:31 Due to this concern for a mass lesion or some other process causing their symptoms. 01:37 For the most part, these are patients who are immunocompromised your concern for a mass lesion or an abscess or possibly also if a patient presents with seizure, maybe another indication to get that head CT before you do the lumbar puncture. 01:50 And the main thing that you’re making sure of is that the elevated intracranial pressure when you do the lumbar puncture, the theory that there is, mostly theoretical risk that you could cause the patient to then herniate their brain tissue due to the fact that you’re caused draining that CSF from the whole brain spinal fluid column. 02:10 So it’s the main thing you wanna make sure you prevent. 02:13 Now granted that this is a little bit of a theoretical risk and there have only been a very rare case reports. 02:19 But for the most part, its gold standard that if you’re worried about that, that you go ahead and take a look. 02:26 Now MRI is a test if you’re worried about spinal epidural abscessing and you would get that of the area of the spine in which the patient would be having pain. 02:39 Like I said, lumbar puncture is your test here that’s gonna give you your answer. 02:43 It’s important to note that you do not wanna delay antibiotics. 02:46 I’m gonna repeat that. 02:47 You do not wanna delay antibiotics. 02:50 You wanna give empiric antibiotics prior to the lumbar puncture. 02:54 So if someone comes in and they look sick and you’re worried they have meningitis, go ahead and treat. 03:01 The antibiotics may potentially affect the gram stain that you send so they may prevent you from actually looking at the slide and seeing what bacteria are there. 03:10 But they do not affect the cell counts, they do not affect the culture of the CSF. 03:15 Then you wanna make sure that you get your — that you go ahead and do the lumbar puncture within a few hours of giving those antibiotics if you’re able to. 03:26 But do not delay the antibiotic, so for the most part, after you give the antibiotics, you have between two and four hours before you need to get that LP and before that LP is affected. 03:36 So go ahead if you’re worried, give the antibiotics. 03:40 Now when you’re doing that lumbar puncture three to four tubes of cerebral spinal fluid should be collected if you're able to The first tube and the fourth tube are gonna be sent for cell count and differential. 03:52 The second tube is sent for protein and glucose levels. 03:55 And then that third tube is sent for any kind of bacterial cultures or PCRs for the most part. 04:00 So any if you’re worried about any viral studies or anything like that. 04:04 So I generally tell people when they’re first doing lumbar punctures, and first learning how to do it, to put a little bit more fluid in that third tube. 04:11 Just in case you’re not really sure what’s going on, that’s the tube that they use for the most part to send it out or to do additional testing for different viral PCRs and other cultures. 04:22 So the lumbar puncture analyze for white blood cells and red blood cells. 04:26 They look for xanthrohcromia which is if there is concern for blood in the CSF. 04:32 The digested blood appears a yellowish color in the CSF. 04:36 They look for glucose and protein. 04:38 gram stain and culture and then additional bacterial and viral testing. 04:43 Talking for a few moments about the CSF. 04:45 So what should be in the CSF? When it comes to cell count, pretty much nothing should be there. 04:50 So you should have a very low white blood cell count, less than five. 04:54 Very low PMNs so those are the polymorphonuclears cells and those are the primary cells that respond to bacterial infection, less than five eosinophils. 05:03 Now in meningitis, you have increased red blood cell counts in all types of meningitis and encephalitis. 05:09 Primarily PMN count suggests that it’s a bacterial pathogen, although not always. 05:16 So very high white count’s most indicative of meningitis. 05:22 Gram stain, classically, you don’t have any organism seen in your cerebral spinal fluid. 05:27 It should be a sterile fluid. 05:29 And meningitis or encephalitis, the offending organism maybe in fact seen there, so it might be seen on the cell that’s made. 05:38 Approximately 80% of the time in bacterial meningitis if again, you patient was pre-treated with antibiotics. 05:44 So if they got the antibiotics before the lumbar puncture that number decrease a bit. 05:49 Turbidity, that’s looking at it and seeing if it looks thick or clear. 05:53 Your CSF should be clear. 05:54 It should look like water. 05:56 So when it’s in the tube, it should look like something you could drink. 05:59 In meningitis, there’s increase turbidity. 06:02 So if you do that lumbar puncture and the fluid comes out yellow or you know a little cloudy looking, that should make you even more concerned that there is an infectious process going on. 06:16 Xanthrohcromia, none should be there and what that is, is its caused by red blood cells being in the spinal fluid for a period of time. 06:26 And what that is, is it's a slight yellowing of the cerebral spinal fluid. 06:31 We look at the CSF to serum glucose ratio. 06:34 So we’re comparing the level of glucose, the fluid, to the level of glucose in our blood. 06:39 The classic thing here is that in bacterial meningitis, you have a low glucose level. 06:47 I always say that the bacteria go around and they eat up all the glucose. 06:51 If that’s the good way for you to remember, you can go ahead and use that. 06:55 Protein level should be approximately between 15 and 45. 07:00 They oftentimes will get elevated in bacterial or fungal meningitis as well as other conditions as well in the CSF. 07:07 Other things to look for cryptococcal meningitis, there’s the India ink stain. 07:11 This is the classic way this was tested for where they put India ink on the slide and they look to see if there is any cryptococcal stuff seen. 07:21 The most classic thing that’s done now is the cryptococcal antigen and the cryptococcal antigen can actually be measured in the blood as well as in the CSF. 07:30 And it has a much higher accuracy for cryptococcal disease when compared with the India ink stain. 07:36 A lactic acid level can be sent which is elevated in bacterial and tubercular meningitis. 07:41 Bacterial antigen testing can be done as well as an acid fast stain which looks for tuberculous meningitis.
About the Lecture
The lecture Meningitis and Encephalitis: Diagnosis by Sharon Bord, MD is from the course Neurologic and Psychiatric Emergencies.
Included Quiz Questions
Which of the following tests is required for a diagnosis of meningitis?
- Lumbar puncture
- Complete blood count
- Head contrast computed tomography
- Head non-contrast computed tomography
- Magnetic resonance imaging
Which of the following statements is FALSE regarding the diagnosis of meningitis?
- Magnetic resonance imaging is indicated to rule out hydrocephalus.
- Empiric antibiotics can be given prior to lumbar puncture.
- 3-4 tubes of cerebrospinal fluid should be collected during lumbar puncture.
- Blood culture may assist in diagnosing meningitis.
- Elevated intracranial pressure is a contraindication for lumbar puncture.
Which of the following values is an abnormal finding in the cerebrospinal fluid?
- 2 polymorphonuclear cells/mm3
- No organisms on Gram stain
- Clear appearance
- 70 grams of glucose
- 30 grams of protein
Which of the following changes in glucose and protein of cerebrospinal fluid is most typical of antibiotic-naive bacterial meningitis?
- Low glucose, elevated protein
- Low glucose and protein
- High glucose, low protein
- High glucose and protein
- Normal glucose and protein
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |