Playlist
Show Playlist
Hide Playlist
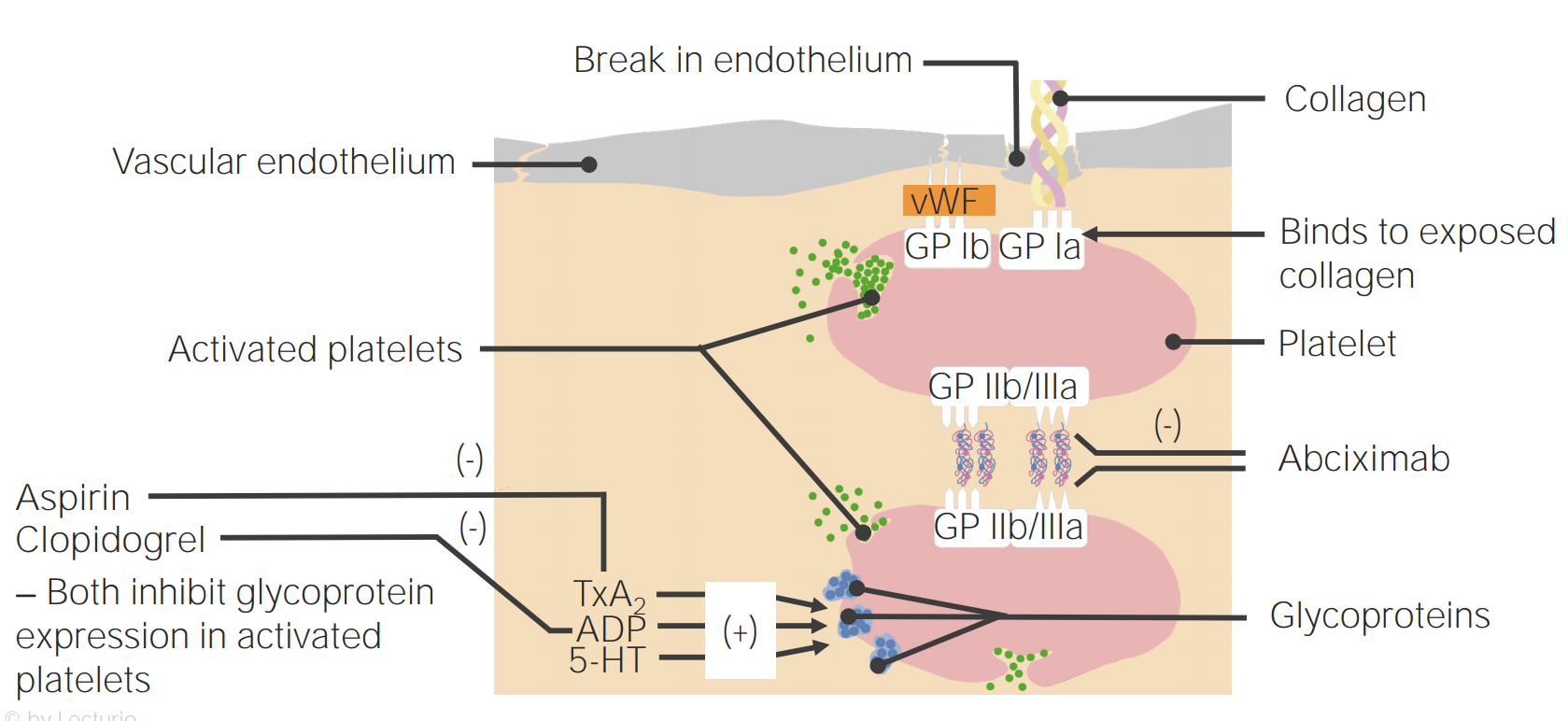
Mechanism of Antiplatelet Interaction
-
Slides Hematology-Pharmacology.pdf
-
Download Lecture Overview
00:01 From here we’ll take a look at antiplatelet interaction. 00:05 Now, step back for one second -- antiplatelet interaction. So what are we trying to do here? We’re trying to, let’s say on the arterial side, alright, arterial side, I want you to think of coronary arterial disease, that would be our prototype and you should be thinking about atheroma, can you picture that for me. Instead of the atheroma you have an LDL core, you have your foam cells and so on and so forth, great! Well, now these are drugs that would then breakdown your platelets. How do we go about doing this? Now here’s an important topic, now take a look at the picture here. 00:40 We’ll begin at the cell on top. The cell on top is showing you the vascular endothelium. 00:46 Now we had a huge discussion in the very beginning of this entire section in which we discussed one that endothelium has been damaged. 00:55 Remind me, what are you expressing underneath that endothelium that is then going to adhere to that platelet that you see there? Ah, vWF, Von Willebrand Factor, and that is going to be the ligand which is then going to receive the receptor known as which one? Glycoprotein 1b. That glycoprotein 1b, let’s talk about this in two ways. 01:22 Well, primarily one, but if there is a deficiency of glycoprotein 1b, what's the name of that disease? Bernard-Soulier. 01:33 Next, our entire discussion here only giving a platelet, you tell me clinically, what is the test that is going to represent the functioning of your platelet, would it be PT? Would it be PTT? Would it be BT? Or would it be D-dimer? If I told you that this picture and this mechanism is only dealing with platelet and it’s not going to be PT, it’s not going to be PTT, we're definitely not breaking down a clot, so it’s not D-dimer, and the only test that could be affected would be bleeding time, period. Is that clear? I told you, too, that glycoprotein 1b deficiency increase in bleeding time, you don’t have adhesion, you don’t have adhesion would be your Bernard-Soulier, or you have a patient that has autoimmune disease such as immune thrombocytopenic purpura. 02:26 Those of you that had memorized that ITP is only autoantibodies against 2b3a is incorrect or should I say inaccurate. 02:35 That, autoantibody not only couldn’t attack 2b3a, it could potentially attack 1b, keep that in mind. 02:43 We don’t really have a drug here for 1b, but important nonetheless. 02:48 What do we wanna do next after adhesion? You're gonna activate the platelet, don’t we? You tell me what’s the name of that receptor that we have on the surface of the platelet? It’s called P2Y12. So you're gonna identify P2Y12. 03:04 So this new -- these drugs we know more about this now. 03:08 This P2Y12 receptors are for ADP activation. 03:13 Here’s some drugs that you should know. 03:16 On the very left you can see the drug called Clopidogrel. I want you to focus on the suffix, g-r-e-l, grel. 03:25 From now on, if you see a drug that has the suffix or has letters grel in them, such as Prasugrel, such as clopidogrel, such as ticagrelar, and the other one maybe ticlopidine you've heard of. 03:41 All of these are prototypic P2Y12 receptor antagonist. 03:47 You’ll notice it is pointing to ADP, it inhibits the ADP in your platelet, huh! If that happens, if ADP never gets properly stimulated or activated, the platelet doesn’t get activated. 04:05 If the platelet doesn’t get activated, guess what, that’s your blood thinner, right? So from now on, when you see the letters g-r-e-l, you should be thinking, oh, ADP inhibitor, and if that ADP or a P2Y12 receptor antagonist and if that ADP is not activated, then that platelet will never express 2b3a. Let’s go and then take a look at that 2b3a next. 04:31 A couple of important things about 2b3a, in fact a multiple of things -- the first thing is, let’s go ahead and try to look take a at the monoclonal antibody here. 04:40 The name of that drug on the right as you see is called abciximab. 04:44 Abciximab is a monoclonal antibody Fab fragment which is then going to particularly target 2b3a. 04:53 Now, why would you think about giving these drugs? Well, you might be thinking about giving clopidogrel, you might be thinking about giving abciximab in the patient that has “aspirin” allergies, right? Well, you know what aspirin does so if you don’t mind I'm just gonna very quickly mention aspirin obviously inhibits our COX pathway irreversively. 05:19 You are going to inhibit the functioning or creation of thromboxane, you are never gonna have or you diminish platelet aggregation, correct? Now, if the patient has aspirin allergy then you might be thinking about abciximab as an alternative. 05:34 One down. 05:36 Let’s go ahead and talk about how maybe the patient has type 2 hypersensitivity, as autoantibodies attacking 2b3a, that would then be called immune thrombocytopenic purpura, there your focus is gonna be on the fact that you have decreased platelet count and the patient is bleeding. Purpura. 05:54 Or let’s say that your patient is deficient of 2b3a. 06:00 If you are deficient of 2b3a this brings us to a condition that is called Glanzmann's Thrombasthenia. 06:05 What the test will be elevated, please? Good, bleeding time, excellent! What is the one last thing that I need to bring to your attention here? Inside the platelet we have something called cyclic AMP. What do you know about cyclic AMP? How do you breakdown cyclic AMP? What's the name of that enzyme that you learned way back in biochemistry? Go phosphodiesterase. There is a classification of drugs called phophodiesterase inhibitors, a drug called cilostazol. 06:37 Cilostazol is a drug that inhibits phosphodiesterase; you therefore increase the concentration of cyclic AMP within the platelet and guess what happens? You inhibit aggregation. Alright, so big picture? We're looking at platelet function and management only. 06:54 You are thinking about a patient prototypically that has coronary arterial disease. 06:59 You are trying to breakdown that thrombi and what we’ve done now is taking the discussion that we had initially with normal temporary platelet plug formation and along the way now, we have now put in some management drugs that you want to keep in mind. 07:16 A very important figure for you to have in mind so that when you know that you're dealing with a DVT versus an arterial thrombi, you know exactly how to manage it effectively.
About the Lecture
The lecture Mechanism of Antiplatelet Interaction by Carlo Raj, MD is from the course Hemostasis: Basic Principles with Carlo Raj.
Included Quiz Questions
Bernard-Soulier syndrome results from a deficiency of which of the following?
- Glycoprotein 1b
- Glycoprotein 1a
- Von Willebrand factor
- Factor VIII
- Factor IX
Which of the following tests is most likely abnormal with platelet dysfunction?
- Bleeding time
- D-dimer
- Thromboplastin time
- Prothrombin time
- International normalisation ratio
Which of the following is mainly affected in Bernard-Soulier syndrome?
- Platelets adhesion
- Endothelial integrity
- Platelet aggregation
- Fibrin cross-linking
- Fibrinogen activation
Which of the following medications is a glycoprotein IIb/IIIa inhibitor?
- Abciximab
- Rivaroxaban
- Heparin
- Dabigatran
- Warfarin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I understand the explanation because he explains it slow and clear, also with very good clinical scenarios.