Playlist
Show Playlist
Hide Playlist
Fetal Malpresentation
-
Slides FetalMalpresentation Obstetrics.pdf
-
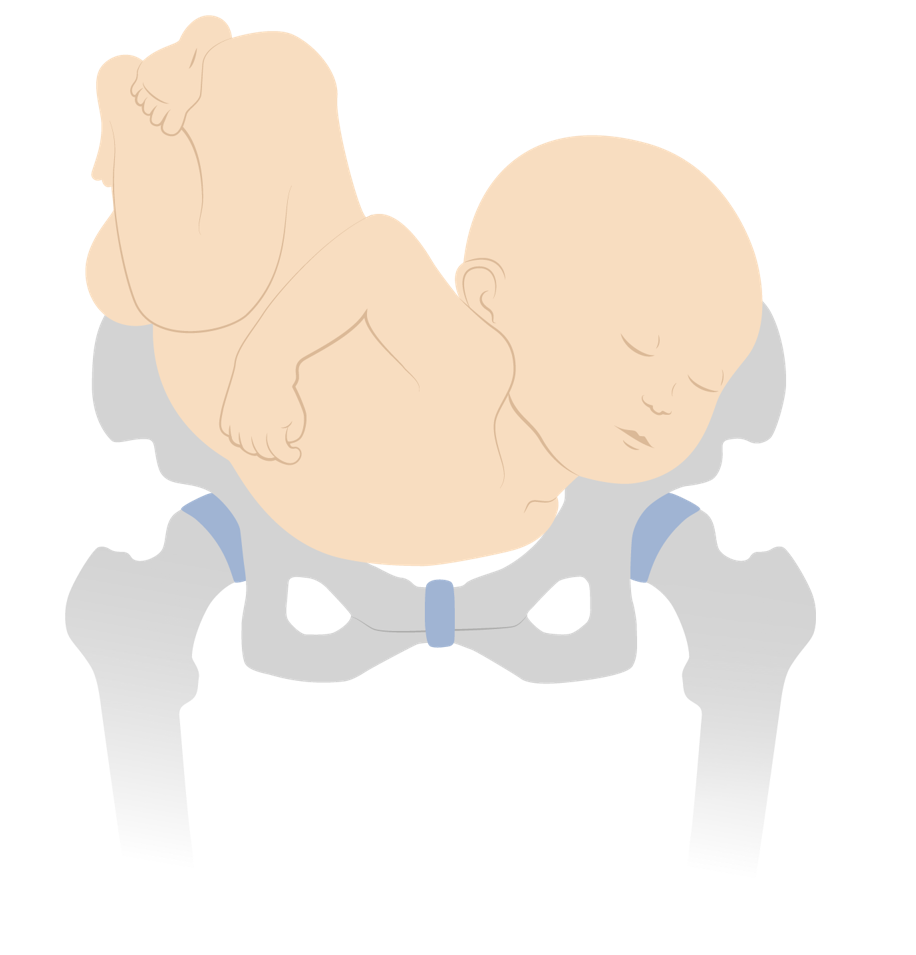
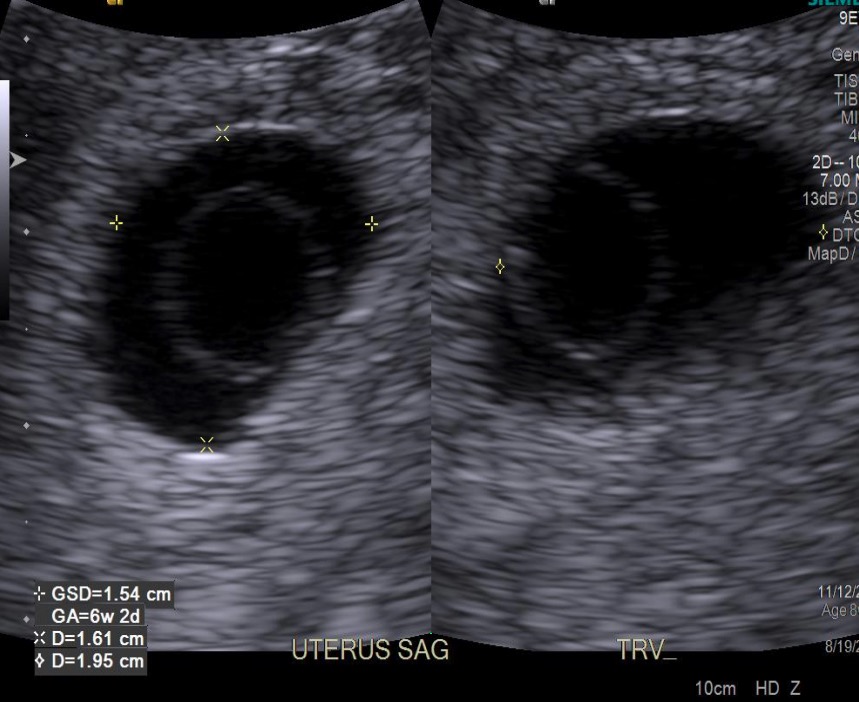
Download Lecture Overview
00:01 Now let's discuss malpresentation of the fetus. 00:05 So here's our patient. 00:06 She's a 27 year old gravida 3 para 2 female that presents for her 36 week prenatal visit. 00:14 Her pregnancy has been uncomplicated. 00:16 She's had two prior vaginal deliveries. 00:18 By Leopold's, the fetal position is felt to be in the breech presentation. 00:23 Ultrasound confirms the fetus is frank breech. 00:27 How would you counsel this patient on her delivery options? Let's go through the lecture to see. 00:32 First let's talk about malpresentation. 00:35 We can have Face presentation, Brow presentation or Breech. 00:40 Now in a normal vaginal delivery in the cephalic presentation, the fetal head is flexed and in the vertex presentation. 00:49 With that the fetal head is about 9 and half centimeters. 00:53 That's what needs to pass through the pelvis. 00:55 The pelvis at it's widest diameter is about 10 centimeters. 00:59 When the fetal head is in the face presentation or the brow presentation, you have a large diameter trying to get through the pelvis. 01:08 If the brow presentation particularly, there's about 14 centimeters of the fetal head trying to traverse the pelvis. 01:14 As you can see here in the picture. 01:16 So because of that brow presentation cannot be delivered vaginally. 01:20 With face presentation you also have a large diameter trying to get through the pelvis but not as large as brow. 01:26 And sometimes face presentation can be delivered vaginally. 01:29 Now, with the face presentation, when the fetus is mentum anterior, you can see that as the head goes through the pelvis, then the head is allowed to flex, meaning that the chin touches the chest. 01:44 That creates a fetal diameter about 9 and half centimeters. 01:47 Again this can be delivered vaginally. 01:50 However, when the fetus is in the mentum posterior presentation, you have a larger diameter trying to get through the pelvis. 01:58 The head is completely deflex. 02:00 Meaning the chin is looking to the ceiling. 02:02 And so you have a larger diameter that just cannot pass through the pelvis. 02:05 So mentum posterior face presentation cannot be delivered vaginally. 02:11 Now we have three types of breech presentation. 02:13 We have frank breech, where you can see the legs are straight. 02:17 Complete breech, where the legs are folded. 02:20 And then we can have footling breech, where one foot is actually trying to pass through the pelvis. 02:26 Now with breech presentations we don't usually recommend a vaginal delivery. 02:30 Why is that? Well, there is definitely some risks to go along with having a vaginal breech delivery. 02:35 First is cord prolapse. 02:37 Meaning the cord can come through before the baby does and this can lead to some fetal heart rate abnormalities. 02:44 Then we have fetal head entrapment. 02:46 If you think about it, the largest part of the fetus is the head. 02:50 So if it is the last part to come through, the cervix is not dilated enough so that the head can pass. 02:55 This can lead to fetal head entrapment and that can lead to hypoxia and death of the fetus. 03:01 Also with vaginal breeches, when we deliver those we have risk of fetal injury as well as fetal death. 03:09 Now with breech presentation, there are two things that we recommend. 03:14 Two routes of delivery. 03:15 One is external cephalic version and next is scheduled cesarean section. 03:20 Let's talk about those are in a little bit more detail. 03:22 So what is an external cephalic version, is the process by which the obstetrician physically turns the fetus from breech to cephalic presentation. 03:32 And you can see here in the diagram, that the obstetrician's arms and hands are on the belly and they are physically turning that baby all the way around. 03:44 Now we usually recommend doing this at 37 weeks and not prior to that. 03:49 We'll just talk about why in just a second. 03:51 The patient has to have no contraindications to a vaginal delivery. 03:55 Because again that's the point of doing the external cephalic version so that you can have a vaginal delivery. 04:00 And because some of the risks that are associated with external cephalic version, you have to have the availability to perform an emergency C-section. 04:08 So with external cephalic version, again this should be performed at 37 weeks because this is term. 04:17 We don't want to cause the patient to go into labor before 37 week with the things that we are doing. 04:23 So for that reason we do not perform external cephalic version until the patient is 37 weeks. 04:29 Now, what are the risks that are associated with external cephalic version. 04:34 First, placental abruption. 04:36 Because you are rotating the fetus, you can disrupt the placenta causing it to prematurely separate from the uterus. 04:43 Next is rupture of membranes. 04:45 Again because you're manipulating the fetus, that means you are also manipulating the amniotic sac and that can cause rupture of membranes. 04:55 Cord prolapse. 04:56 Again when you are manipulating the fetus, you can cause the cord to come out. 05:00 And this will necessitate a emergency C-section. 05:05 Now because you are moving the baby around, sometimes the babies don't like that and you can experience fetal distress. 05:12 Sometimes that will resolve, sometimes it does not resolve and that necessitate an emergency C-section as well. 05:19 And then another risk is fetal hemorrhage. 05:21 Again, if you disrupt the placenta or the cord through the external cephalic version that can cause hemorrhage and that also necessitates an emergency C-section. 05:32 Now if a patient decides she does not want to do an external cephalic version or if external cephalic version is contraindicated or if it is not successful, then elective C-section is performed at 39 weeks gestation. 05:47 So far our case, as we mentioned before she is a patient that's presenting at 36 weeks with a breech presentation. 05:56 So what are the things that we can offer her. 05:58 Again this patient is a candidate for an external cephalic version. 06:02 She's had two vaginal deliveries. 06:03 This again makes her a great candidate. 06:06 But we do need to discuss with her the risk, benefits and alternatives of doing that procedure. 06:12 So back to our patient that presented 36 weeks with her breech presentation. 06:16 Which of the following is not a risk of breech vaginal delivery? Is it A. Cord prolapse. 06:23 B. Head entrapment. 06:25 C. Postpartum hemorrhage or D. Fetal death. 06:29 The answer is postpartum hemorrhage. 06:32 Again because we are delivering the baby vaginally the cord can come down before the baby causing a cord prolapse. 06:40 As we stated before the head is the largest part of the baby, so if it is the last thing to come out, you can have head entrapment. 06:48 And because of these risks fetal death is also a risk associated with breech vaginal delivery. 06:52 However, postpartum hemorrhage is not.
About the Lecture
The lecture Fetal Malpresentation by Veronica Gillispie, MD, MAS, FACOG is from the course Antenatal Care. It contains the following chapters:
- Malpresentation of the Fetus
- Face Presentation
- Breech Presentation
- External Cephalic Version (ECV)
- Cesarean Section
Included Quiz Questions
A bedside ultrasound shows a fetus in mentum-posterior brow presentation. What is the recommended route of delivery?
- Cesarean section
- Expectant management for spontaneous vaginal delivery
- External cephalic version followed by expectant management for spontaneous vaginal delivery
- Operative vaginal delivery using a vacuum or forceps
- Episiotomy followed by expectant management for spontaneous vaginal delivery
Which of the following is NOT required in order to perform an external cephalic version?
- Platelet count over 110,000
- 37 weeks gestational age
- No contraindications to vaginal delivery
- Ability to perform an emergent cesarean section
- Maternal consent for the procedure
Which of the following is NOT a risk of external cephalic version?
- Fetal head entrapment
- Placental abruption
- Rupture of membranes
- Fetal distress
- Fetal hemorrhage
Which of the following is a contraindication to performing an external cephalic version?
- Placenta previa
- 38 weeks gestational age
- History of cord prolapse in a previous delivery
- First-time pregnancy with no history of vaginal delivery
- Maternal gestational diabetes
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like this lecture because the teacher explain clearly so i understood easily.