Playlist
Show Playlist
Hide Playlist
Local Invasion and Metastases
-
Slides 07 LungCancer Tumors and Metastases Neoplasias RespiratoryAdvanced.pdf
-
Download Lecture Overview
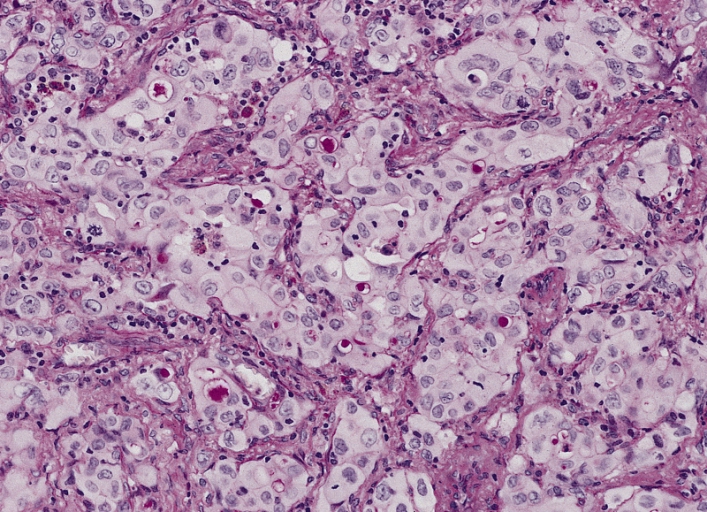
00:00 So we talked about how cancers may cause the symptoms in the lung with cough haemoptysis. But there are other problems and it might cause in the thoracic cavity. And these are due to local invasions of either the chest wall or the pericardial mediastinal structures or metastases in that area. So for example, you can have metastases that go the hilar and then to the mediastinal lymph nodes. So you end up with enlarged nodes within the mediastinum. These are frequently asymptomatic and just picked up on x-ray. However if it is next to the superior vena cava, an enlarge node as it gets bigger can cause obstruction of the superior vena cava. 00:49 And that will present the patient with poor return of blood to the heart down the superior vena cava causing edema of the upper limbs, the face, potentially head ache due to that venous congestion and a very fixed and engorged JVP that you can see in the neck which doesn’t move because the normal pulsations that you see in the JVP occur in the atrium and they're not transmitted through the obstructed path in the higher part of the mediastinum. And there may be dilated veins across the chest because those are collaterals which are trying to get around the obstructions of the superior vena cava. 01:25 Another presentation of mediastinal tumours is recurrent laryngeal nerve palsy and that is because the left recurrent laryngeal nerve. Before it goes to the larynx comes down into the mediastinum around the arterial aorta and that makes it vulnerable to enlarge nodes and cancers at that site to be paralyzed and that will cause a hoarse voice and what we called a bovine cough. It's a specific nature of cough that sounds a little bit like a cow. It's slightly odd. Other nerves could be damaged by mediastinal tumors through the phrenic nerve which can be paralyzed and cause a right or left hemidiaphragmatic paralysis which is seen on an x-ray by raised hemidiaphragm. Posterior tumours can cause esophageal obstruction and that will present with dysphagia, an inability to swallow and potential aspiration because of that obstructions from esophagus into the lungs. Of course we have already mentioned this collapse of the major bronchi could occur not just by primary tumour but can occur by secondary’s affecting enlarged nodes which are positioned around the major bronchi and that will cause lobar collapses and breathlessness as the consequence of that. 02:35 Further out of the chest. If you have a cancer that is in the periphery, then it may invade the periphery of the lung. It may invade into the chest wall. The lungs is quite unusual, it doesn’t have much in the way of pain fiber, so in fact you can have a very large tumour within the lung that you will never know due to pain. But as soon as it starts invading the chest wall, then the pain becomes a problem and this pain would be normally a constant pain that has been evolving and getting worse over a period of a weeks. If you hear a history where the patient describes a pain which is getting worse all the time and never goes away, can be relieved to a degree by pain-killers. But never goes away otherwise that you need to think about the potential cancer. So for example, if you have a pancoast's tumour which is an apical cancer, the one which we showed in x-ray, then the pain occurs because the tumour is eroding into the brachial plexus and causing the referred pain down the arm. 03:43 So the patient presents with pain in the arm rather than chest. If it’s a tumour affecting a lateral chest wall then infact the pain will be localized down to that area and to the distribution of the intercostal nerves distal to that surround there. 03:58 In addition to pain you can get what we call a Horner’s syndrome where the cervical sympathetic nerves has been affected by an apical tumour and that presents with patients with a droopy eyelid, a partial ptosis, a small pupil and loss of sweating on that side affected. If you do x-rays of patients with chest wall invasion then you can see that the ribs have been destroyed by a soft tissue mass and that’s very suggestive that there is a cancer and very occasionally patients will have such a severe chest wall invasion that actually you can feel it when you examine the patient that the mass is large enough to be palpable for the skin and occasionally even all straight through the skin.
About the Lecture
The lecture Local Invasion and Metastases by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Lung Cancer.
Included Quiz Questions
Which of the following is NOT a feature of superior vena cava obstruction due to a tumor mass?
- Raised hemidiaphragm
- Arm and face edema
- Headache
- Fixed and engorged jugular vein
- Dilated superficial chest wall veins
Which of the following is a characteristic of left phrenic nerve palsy due to compression by a tumor mass?
- Raised left hemidiaphragm
- Raised right hemidiaphragm
- Hoarseness
- Dysphagia
- Fixed and engorged jugular vein
Which nerve palsy can present with hoarseness due to the mediastinal tumor?
- Left recurrent laryngeal nerve palsy
- Right recurrent laryngeal nerve palsy
- Left pharyngeal nerve palsy
- Right anterior laryngeal nerve palsy
- Right phrenic nerve palsy
Which of the following is NOT part of Horner syndrome?
- Hoarseness
- Ptosis
- Miosis
- Anhidrosis
- Enophthalmos
Which of the following is unlikely seen with a Pancoast tumor?
- Phrenic nerve palsy
- Brachial plexus invasion
- Pain in T1 distribution
- Wasting of the small muscles of the hand
- Horner syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |