Playlist
Show Playlist
Hide Playlist
Lead Poisoning (Plumbism) in Children
-
Slides Poisonings in Children.pdf
-
Download Lecture Overview
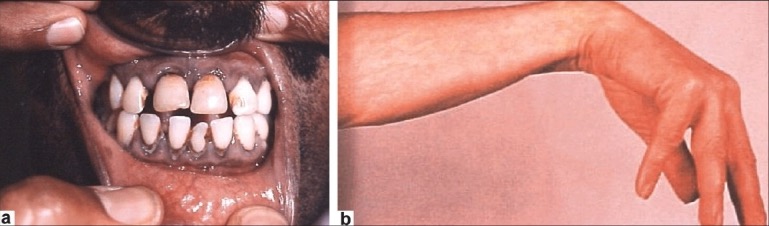
00:01 Okay. 00:02 Let’s switch gears to another type of poisoning. 00:06 The picture of the city you can see here, this is Flint, Michigan. 00:11 And last year, in 2016, there was a maneuver where a mayor wished to save money on the water bill for the city and accepted another source of water. 00:25 The government failed to treat that water appropriately and it caused lead to leach out of pipes that existed in the old city system and they provided lead into the drinking water for the entire city. 00:41 This poisoned thousands of children and the government was very slow to respond and knew about the problem and kept telling people that it was safe to drink the water, further hurting children in this city. 00:54 Children especially because children tend to be more severely affected than adults by lead poisoning because they have developing brains. 01:03 So lead poisoning can happen as a result of a system-wide abuse of water or some kind of systemic pollution. 01:12 But it can also happen in the home of an older home where they may be a history of lead paint and that paint is now peeling and the child can eat it. 01:22 Or it can be from other exposure such as having lead on the parent’s clothes if they work in certain places. 01:29 So children under six are more susceptible to brain damage as a result of lead poisoning. 01:36 And this can cause chronic or acute toxicity. 01:42 Let’s go through lead poisoning. 01:44 It’s often inhaled as dust or it’s old paint in old houses that children peel off because it’s interesting to peel off and maybe chew. 01:54 They can ingest these paint chips or if they have psychiatric disturbances, they may have pica and just want to eat things. 02:01 You can also find it in contaminated soil or water like in Flint, Michigan. 02:07 And typically, the presentation is worse in children who have a low calcium or a low iron diet because iron and calcium compete for lead absorption. 02:17 So a high calcium or a high iron diet is protective against lead poisoning. 02:23 The symptoms are important to remember. 02:26 A common one with a relatively low exposure is anemia. 02:30 This is usually a microcytic or sometimes normocytic anemia. 02:35 Patients with acute ingestion may first develop abdominal pain. 02:39 If it’s very severe exposure and the lead levels are high, they may develop peripheral neuropathy, hearing loss, they may incur developmental delay, and they may have frank encephalopathy. 02:53 The developmental delay is key. 02:55 No amount of lead in the environment is safe for children. 03:00 Children need to be lead-free. 03:02 They’ve even shown that lead levels as low as 5 to 10 may cause, if exposed chronically, developmental issues with resulting loss of IQ. 03:16 There may be some things on exam or on testing that can yield evidence of lead poisoning. 03:21 For instance, we sometimes see children who get an X-ray for a broken bone and we see lines on those bones. 03:27 That’s a sign of lead toxicity. 03:29 They develop these lead lines at the time of accrual of the lead. 03:33 It can adhere to the growing surface of the bone and create lines. 03:37 We see it on CBC. 03:39 When we see a microcytic or a normocytic anemia, more commonly microcytic, and you may even see basophilic stippling, which you can see with these arrows, these little blue dots. 03:52 If we suspect lead poisoning, we need to check a serum lead level. 03:56 And always provide iron supplementation to poisoned children because that can help compete with lead ingestion. 04:04 It’s important for patients who have lead exposure to have long term followup for developmental problems and early intervention and other ways we can do to maximize their potential. 04:15 But we generally will treat children based on what their lead level is. 04:20 So if their lead level is 5 to 14, we will remove exposures and retest them in three months and watch for associated learning defects. 04:29 For lead levels that are 15 to 44, we will need to confirm with a venous sample, because normally, we usually just get capillary test. 04:38 And we get an abdominal X-ray if they have pica for fear that there may be lead chips in their bellies. 04:44 So we ask about paint because that’s so common and if there is paint in the house, we’ll get an abdominal X-ray to look for other lead in the abdomen. 04:52 If that’s present, we may give NG GoLYTELY to flush it out so that they don’t absorb it. 04:59 Charcoal doesn’t really work. 05:01 Next, if they’re 45 to 69, they’re usually asymptomatic but we’re going to treat with oral succimer. 05:09 We’re going to chelate them with an oral agent to try and suck the lead out. 05:14 We have to continue to watch them carefully because the oral succimer will transiently raise their lead levels as some of that lead was stored in their bones and is getting sucked to their plasma. 05:26 For patients with a lead level over 70, these patients will require a hospitalization. 05:31 They often have encephalopathy and we have to give both succimer and calcium EDTA as ways of controlling their lead toxicity. 05:41 So that’s my review of common poisonings in children. 05:45 Thanks for your time.
About the Lecture
The lecture Lead Poisoning (Plumbism) in Children by Brian Alverson, MD is from the course Pediatric Emergency Medicine.
Included Quiz Questions
Lead poisoning can cause all of the following symptoms, EXCEPT?
- Thyrotoxicosis
- Tingling of the hands and feet
- Encephalopathy
- Abdominal pain
- Hearing loss
Which of the following can exacerbate lead poisoning?
- Iron deficiency
- Hypercalcemia
- Anemia
- Administration of zink
- Chelation therapy
What percentage of lead in the environment is safe for children?
- No amount of lead is safe for children
- 2-10
- 10-15
- 15-20
- 20-30
Which of the following is the most appropriate next step in the diagnosis of a child with lead levels of 35 micrograms/dL and a history of chronic paint chip ingestion?
- Abdominal X-ray
- Abdominal ultrasound
- Esophagogastroduodenoscopy
- No further diagnostic tests required at this time
- Echocardiography
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |