Playlist
Show Playlist
Hide Playlist
Laryngomalacia and Tracheomalacia
-
Slides LaryngomalaciaTracheomalacia Pediatrics.pdf
-
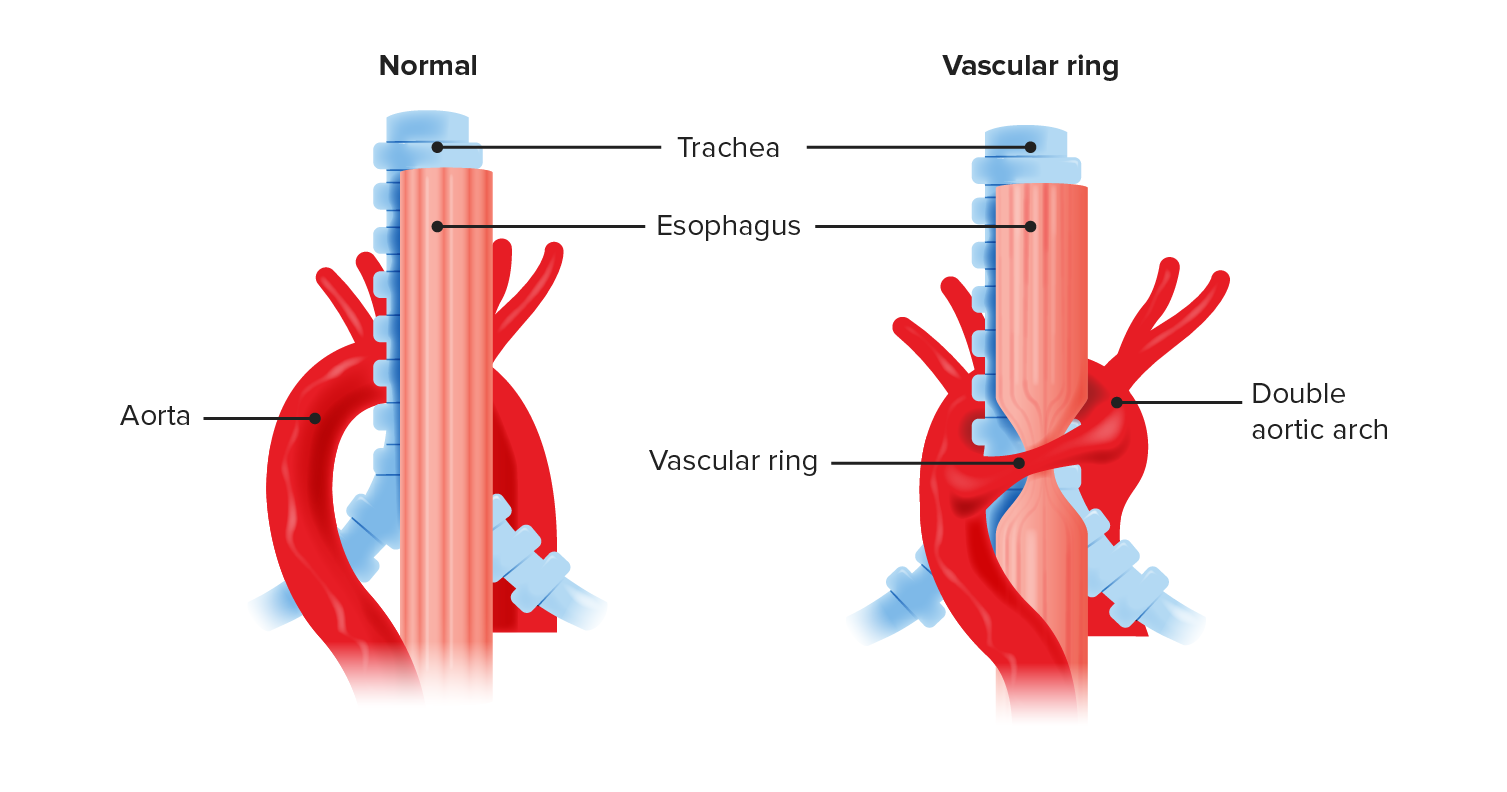
Download Lecture Overview
00:08 So basically, malacia means narrowing or it’s a floppy area. 00:13 And this can happen in either the larynx or the trachea. 00:17 It’s a common problem especially in premature infants. 00:21 We see this all the time. 00:23 There are some genetic influences, but the cause is basically unknown. 00:28 And it’s basically a collapse in the airway, in the larynx, or in the trachea due to probably mostly poor airway motor tone. 00:37 These infants have just a hard time keeping it stented upon when they're breathing. 00:42 So it presents with noisy breathing. 00:46 And typically depending on where the location is primarily will depend on what that noise is. 00:53 Stridor usually occurs for patients who have a higher area of malacia. 00:59 In other words, in laryngomalacia, for example, their airway collapse is a little bit higher up. 01:05 This means that when they breathe in, it’s like breathing in through the neck of a balloon. 01:11 It collapses and makes a stridorous noise. 01:14 But when they breathe out, it will sort of billow open and there’ll be less noise. 01:19 Or alternatively, patients could have laryngomalacia, but also have some tracheomalacia. 01:26 And the tracheomalacia will have more of an exhalational component to it. 01:31 So it may be biphasic or just stridor or if it’s all low down, just wheeze. 01:37 It will give you a clue as to the location of the airway collapse. 01:42 The reason why it’s important to remember the clue of the airway collapse and where this is likely happening is because there is a differential diagnosis. 01:50 We can’t just assume that any baby with stridor doesn’t have something more substantial going on. 01:57 Patients may get superglottic webs. 02:01 These areas of tissue that are inappropriately growing in the airway and thus making the airway narrower and having it harder to breathe in. 02:10 Patients may have airway hemangiomas. 02:13 This is particularly likely if you see some also on the baby’s skin. 02:18 An airway hemangioma can be very challenging. 02:20 It may require laser therapy or other things. 02:23 Or we simply hope they’ll outgrow it and gradually wait until they get bigger because just like hemangiomas on the legs, these will gradually shrink over several months. 02:33 But this can be very challenging because they will also grow for the first few months and so we need to watch these children very carefully. 02:41 Another potential cause of stridor or wheeze in an infant is a vascular ring. 02:47 There are many different types of vascular rings and it will take forever to list them all. 02:51 And for example, the aorta may be together come apart and then go back together again. 02:57 And in that space in between, that sort of like an island on a highway, that trachea can run through that area. 03:04 Oftentimes, the esophagus does as well. 03:07 This can lead to not only spitting up of food, but also a narrowing of the tracheal airway which may happen a bit after birth as they sort of grow into that vascular ring. 03:17 Then we could hear more respiratory symptoms. 03:19 Another possibility is the patient has a cyst or another structure that’s pressing on that airway like a lingual thyroid or a thyroglossal duct cyst. 03:29 And patients may have subglottic stenosis, just an area of narrowing that’s causing the problem. 03:36 Subglottic stenosis is common in infants who have recently been intubated. 03:40 That intubation can cause damaging below the vocal cords and a little stenotic area, which can present with noisy breathing. 03:49 So for any infant with stridor, we have to think about what might be causing it. 03:53 And so we’ll probably do some studies to try and get a sense of what exactly is going on. 03:59 One thing we can do is the neck X-ray. 04:01 By looking at a neck x-ray, we can seen an area of focal narrowing and get a sense of where is it and is that consistent with a mass or is it consistent with a general floppy airway. 04:12 If we aren’t convinced by the neck X-ray but we don’t have any specialist nearby who can look in with a camera, we might also do airway fluoroscopy. 04:22 What we’re doing is making a video with x-rays and we can see that airway collapsing and we can make a diagnosis. 04:28 Lastly, if we’re just not sure what’s going on, it’s very reasonable to consult ear, nose and throat doctors to do direct video laryngoscopy. 04:36 They can actually look inside and see what’s going on. 04:39 They can diagnose laryngomalacia or tracheomalacia, but they can also see the airway hemangioma or see an area that’s compressed by an external mass, et cetera. 04:51 So how do we support these infants. 04:53 Well, in most cases, the treatment is entirely supportive because as they grow, this problem goes away. 04:59 Usually, by two or three years of age, it’s all gone. 05:02 So we’ll provide CPAP in some severe cases. 05:06 This will help stent open that airway of collapse and keep them breathing comfortably. 05:10 Most children do great with this. 05:13 There is a frequent readmission in these infants specifically with upper respiratory tract infections. 05:20 Bronchiolitis or even just the common cold can tip them over the edge and make it very hard for them to breathe. 05:26 And typically, they’ll outgrow this by two years of age. 05:30 So that’s a brief summary of laryngomalacia and tracheomalacia in kids. 05:35 Thanks for your time.
About the Lecture
The lecture Laryngomalacia and Tracheomalacia by Brian Alverson, MD is from the course Neonatology (Newborn Medicine).
Included Quiz Questions
Which of the following diseases does NOT cause stridor in the infant?
- Bronchiolitis
- Supraglottic web
- Laryngomalacia
- Vascular ring
- Subglottic stenosis
Which of the following is an important risk factor for acquired subglottic stenosis in children?
- Prolonged mechanical intubation
- Prematurity
- Poorly controlled diabetes in mother
- Delivery by Cesarean section
What is the most appropriate management in infants with a confirmed diagnosis of tracheomalacia without an associated problem?
- Observation and supportive therapy
- Surgical intervention before the age of 6 months
- Surgical intervention between 6 months and 1 year
- Immediate surgical intervention at the time of diagnosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture as usual. Well-summarized, well-explained, easy to remember.