Playlist
Show Playlist
Hide Playlist
Juvenile Idiopathic Arthritis (JIA)
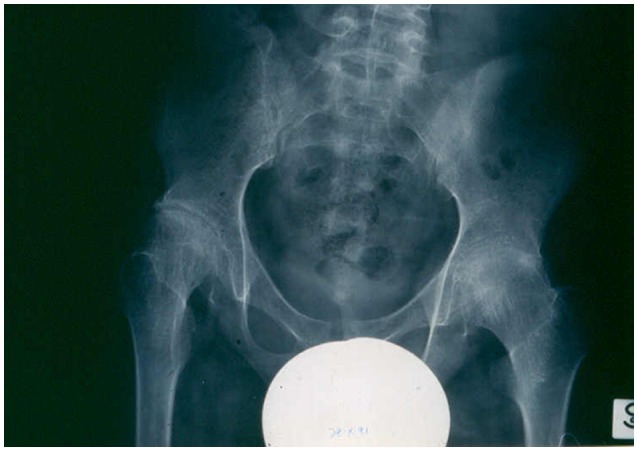
00:01 In this lecture, we will discuss Juvenile Idiopathic Arthritis. 00:07 Here's a classic case. 00:09 An 11-year-old child is presenting to you after several rounds of antibiotics with a complaint of long standing pain and swelling of the fingers, wrists and ankles. 00:20 What's the most likely diagnosis? In this case, it's probably Juvenile Idiopathic Arthritis or JIA for short. 00:30 JIA causes pain and swelling in the joints that typically lasts longer than six weeks. 00:37 It's an autoimmune disease that primarily affects children, and is typical onset is before 16 years of age. 00:46 There are three different major types of JIA and a few smaller less common types. 00:53 The major types that are likely to show up on our exam are Oligoarticular JIA which usually involves fewer than six joints, Polyarticular JIA which is multiple joints, and Systemic JIA which may involve a wide variety of systemic symptoms. 01:12 There are other types of JIA too that are less common. 01:17 Enthesitis-associated JIA is a variety of JIA that causes enthesitis which is an inflammation of the insertion of around the joint. 01:29 Psoriatic JIA is associated with psoriasis of the skin. 01:33 And Undifferentiated JIA may be a variety of different types of JIA that don't really fit into one category in that particular patient. 01:43 So, JIA characteristics do usually involve joint inflammation. 01:49 And the synovium is the target for that autoinflammatory process. 01:54 It results in a proliferation of synovial tissue and increased joint fluid. 02:00 You may see increased blood flow, swelling and inflammatory cells if you were to tap that joint. 02:07 The progression of symptoms is generally it starts off with a persistent synovitis which then results in joint destruction, which can cause long term bone, tendon, ligament problems. 02:21 So of the three major types, they tend to present slightly differently. 02:26 Let's start with Oligoarticular JIA. 02:29 This is about half of cases, females are more commonly affected than males. 02:34 And it's really in the 2-3 year range. 02:38 It would be very rare for this disease to present after 10 years of age. 02:43 Polyarticular JIA is about a third of cases. 02:47 Again, females are more affected than males. 02:50 And there seem to be two periods of time when it shows up the most between 2 and 5, and between 10 and 14. 02:59 Systemic JIA is the minority of cases only about 1 in 10. 03:04 And there's no predominance for either gender. 03:06 It can happen at any age, really under 17 years of age. 03:12 So let's drill down on the three major types of JIA. 03:17 Oligoarticular JIA is usually less than five or at least less than six joints that are affected. 03:25 Those joints include medium and large joints, the disease tends to be asymmetric and how it attacks the child. 03:33 It's rarely that involves the hips, and this tends to be a non-destructive arthritis. 03:40 There are usually no systemic features. 03:42 These children are a febrile and otherwise doing well. 03:45 But there are two groups. 03:48 If the child has ANA+, they are more likely to have a uveitis about 20% of the time. 03:54 The ANA- patients are less likely to. 03:59 Polyarticular JIA usually involves multiple joints. 04:03 It can involve any joint it wants to but this disease is usually more symmetric. 04:09 So our initial case with involvement of the hands, the feet, the ankles would be classic for a Polyarticular JIA. 04:18 It rarely involves the hips as well and this is a destructive arthritis unlike the oligoarticular variety. 04:26 It less frequently causes uveitis. 04:30 Polyarticular JIA is broken down into 0- and 0+ Polyarticular JIA depending on whether the rheumatoid factor is negative or positive. 04:41 0+ Polyarticular JIA, an analogue of adult rheumatoid arthritis is seen in less than 10% of pediatric patients. 04:50 0- Polyarticular JIA, an entity more specific for childhood appears with widespread large and small joint involvement. 05:03 Systemic JIA may have any joints or no joints. 05:08 If it involves joints, it's often a destructive arthritis. 05:12 These patients usually come in complaining of high fevers daily. 05:17 They may have an evanescent salmon-pink rash, and I'll show you a photo of that in a minute. 05:22 They may have a hepatosplenomegaly, lymphadenopathy, or heart, lung or liver involvement. 05:29 These children have a systemic autoimmune process. 05:34 Here's an example of how children can be affected. 05:38 These are two sisters. 05:39 And this 4-year-old sister is substantially affected in terms of her ability to have functioning joints long term. 05:47 This is the chronic destruction you see in what is likely in this child. 05:52 Polyarticular JIA, it's symmetric, it's involving multiple joints. 05:58 So when you're diagnosing a patient, you will want to hear a history of joint pain and typically, unless it's the systemic variety that you're suspecting. 06:08 Oftentimes patients will have morning stiffness or stiffness still for after being still for a prolonged period of time we call this gelling. 06:18 In other words, if a patient is just sitting there for a while and then gets up, they have that stiffness again, These patients often have limp, especially when the lower extremities are involved. 06:30 About 25% of patients with JIA will have no report of pain and only swelling, and the massage doesn't seem to help. 06:41 So here is that salmon-pink rash that evanescent rash of systemic onset JIA. 06:47 I'll be honest, I have not seen this rash in the patients that I've seen with systemic JIA. 06:53 It's not always there and it doesn't always show up in any individual patient.
About the Lecture
The lecture Juvenile Idiopathic Arthritis (JIA) by Brian Alverson, MD is from the course Pediatric Rheumatology and Orthopedics. It contains the following chapters:
- Juvenile Idiopathic Arthritis
- Types of JIA
- Historical Findings of JIA
Included Quiz Questions
Which of the following statements is TRUE about systemic juvenile idiopathic arthritis?
- It can affect any age of children.
- It's the most common form of JIA.
- Fewer than 6 joints must be involved.
- Patients present with psoriasis.
Which type of juvenile idiopathic arthritis involves fewer than 6 joints, has a higher prevalence in girls, and has an onset around the age of 2-3 years?
- Oligoarticular JIA
- Polyarticular JIA
- Systemic JIA
- Psoriatic JIA
- Undifferentiated JIA
Which of the following is NOT a feature of polyarticular juvenile idiopathic arthritis?
- Daily fevers
- Involvement of multiple joints
- Symmetric joint involvement
- Destructive arthritis
- Inflammation of five or more joints
Which of the following is the target organ for inflammation in juvenile idiopathic arthritis?
- Synovium
- Articular ligaments
- Articular cartilage
- Subchondral bone
- Articular capsule
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. As usual, a complex topic made simple: easy to understand, easy to remember. Good first layer of knowledge. Thanks!