Playlist
Show Playlist
Hide Playlist
Type 2 Diabetes: Insulin Treatment
-
Slides Diabetes ChronicCare.pdf
-
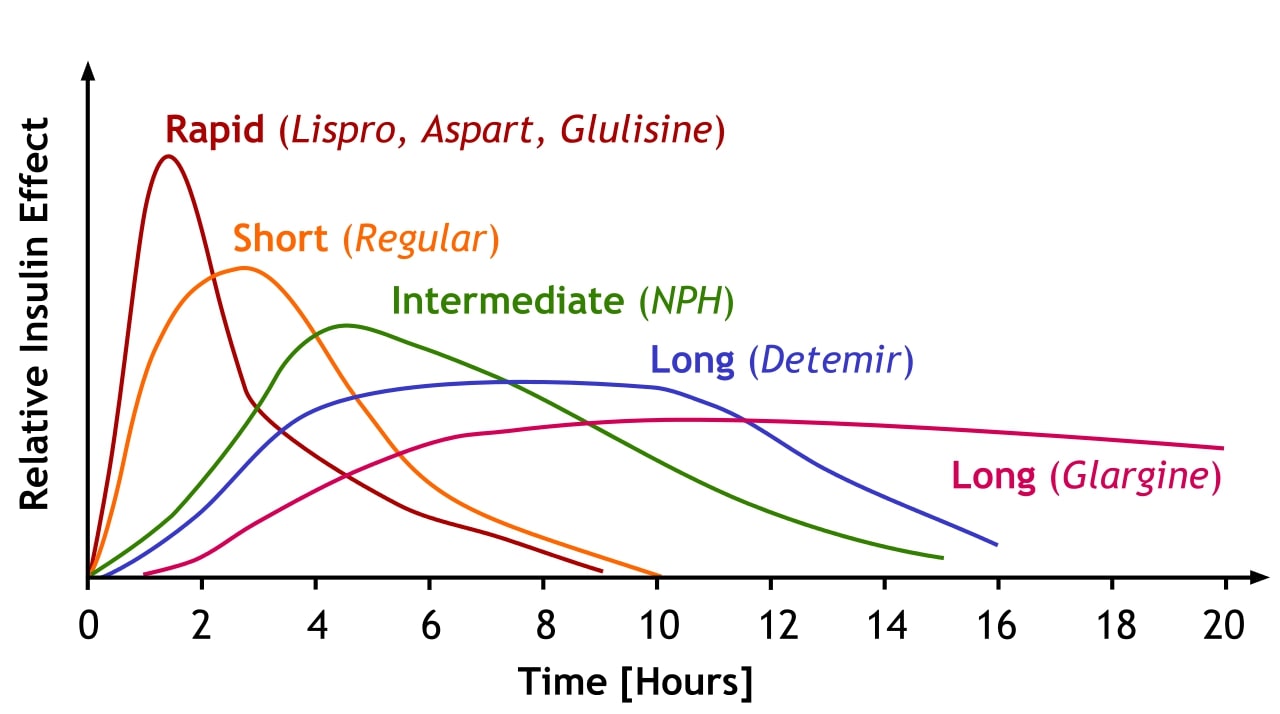
Download Lecture Overview
00:01 Say, the patient is not doing that well and continues to maintain a high A1c despite your best medical therapy. 00:09 So, patients who come in with an HbA1c above 9 can be considered for insulin. 00:15 In my practical experience, most clinicians aren't thinking about using insulin right off the bat unless they come in with an A1c of 11 or more. 00:25 But one thing that’s certainly true is patients who are failing badly and taking two oral anti-diabetes drugs, there's not much point in putting them on a third oral diabetes – anti-diabetes drug. 00:37 At that point, it's time to reconsider therapy and include insulin in that regimen. 00:43 The problem with insulin is there's just a lot of variability. 00:47 How often the patient uses it, their diet, how used they are to checking their home glucose, how involved their health literacy, all of these things factor into the efficacy of insulin. 00:58 It's, frankly, probably easier to take a pill. 01:02 But you can start with something basic, like augmentation of their usual therapy with basal insulin. 01:08 There is the dose, 0.3 units per kilogram per day. 01:12 That's – this is really where you want it. 01:15 If you haven’t initiated doing home glucose monitoring, you're going to want to initiate home glucose monitoring and warning the patient about hypoglycemic symptoms and how to react because, of course, it’s one of the downsides of insulin treatment. 01:26 It is a nice opportunity, in my opinion, to check on lifestyle because you can follow along and you notice when they go – when the patient goes high with their glucose readings at home and when they go low and what happened. 01:37 Oh, that’s the day I exercised. 01:39 That’s the day I forgot to eat. 01:41 Or when it's high, oh, that was a big party I went to and I kind of went nuts and ate whatever I wanted and that's why glucose was 450. 01:48 So, it can give you some insights into how to counsel patients about because lifestyle never leaves just because the patient goes through diabetes education classes and meets with an educator or a (inaudible) or whatever. 02:02 It's never quite over. 02:04 You have to keep up that lifestyle. 02:06 And importantly, once you initiate insulin treatment, don't let go of whatever foundational drug they were taking, whether it be metformin or a GLP-1 agonist. 02:14 It can help mitigate against the weight gain you're going to experience with insulin. 02:19 But sulfonylureas, once you start prandial insulin, there’s not much point in using sulfonylureas anymore. 02:24 Get them off because they might promote hypoglycemia and weight gain. 02:27 And hypoglycemia is a serious risk. 02:29 So, really monitor it closely. 02:31 Keep these levels in mind. 02:32 Goal glucose levels for fasting patients, 90 to 130 mg/dL; for postprandial, less than 180 mg/dL. 02:42 Okay. 02:43 So with that, happy to give you that overview on diabetes care. 02:50 I think the keys are, get the diagnosis right. 02:52 And usually requires a couple of readings to do so. 02:55 Make sure they get their screening on a routine basis for their eyes and for their feet as well as for kidney disease, with the microalbumin and creatinine ratio. 03:03 And you should have some very satisfied and healthy patients. 03:06 Thanks.
About the Lecture
The lecture Type 2 Diabetes: Insulin Treatment by Charles Vega, MD is from the course Chronic Care.
Included Quiz Questions
Which of the following is the most appropriate pharmacotherapy for a diabetic patient with HbA1c of 9.5% and failure of 2 oral anti-DM drugs?
- Addition of basal insulin
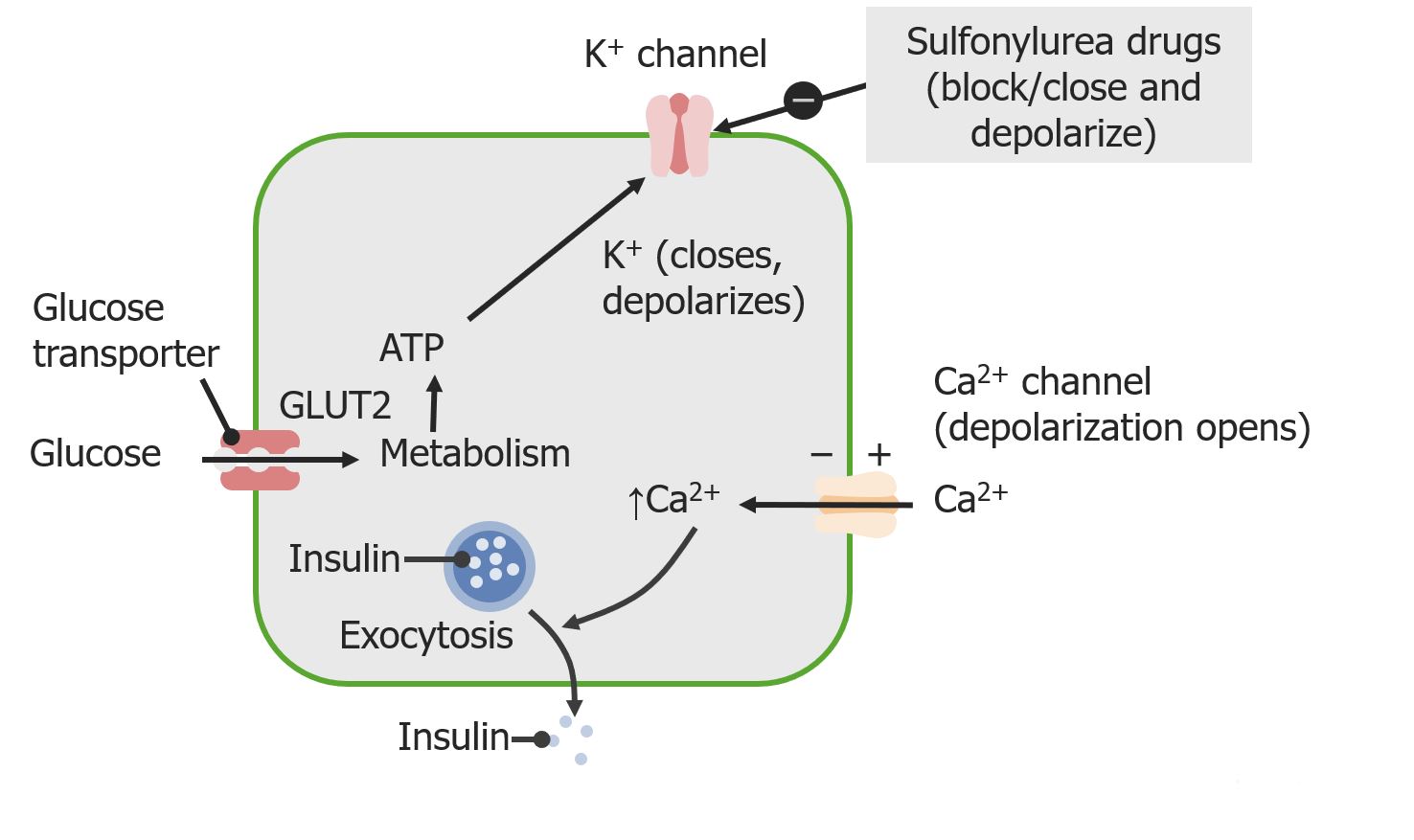
- Addition of a sulfonylureas
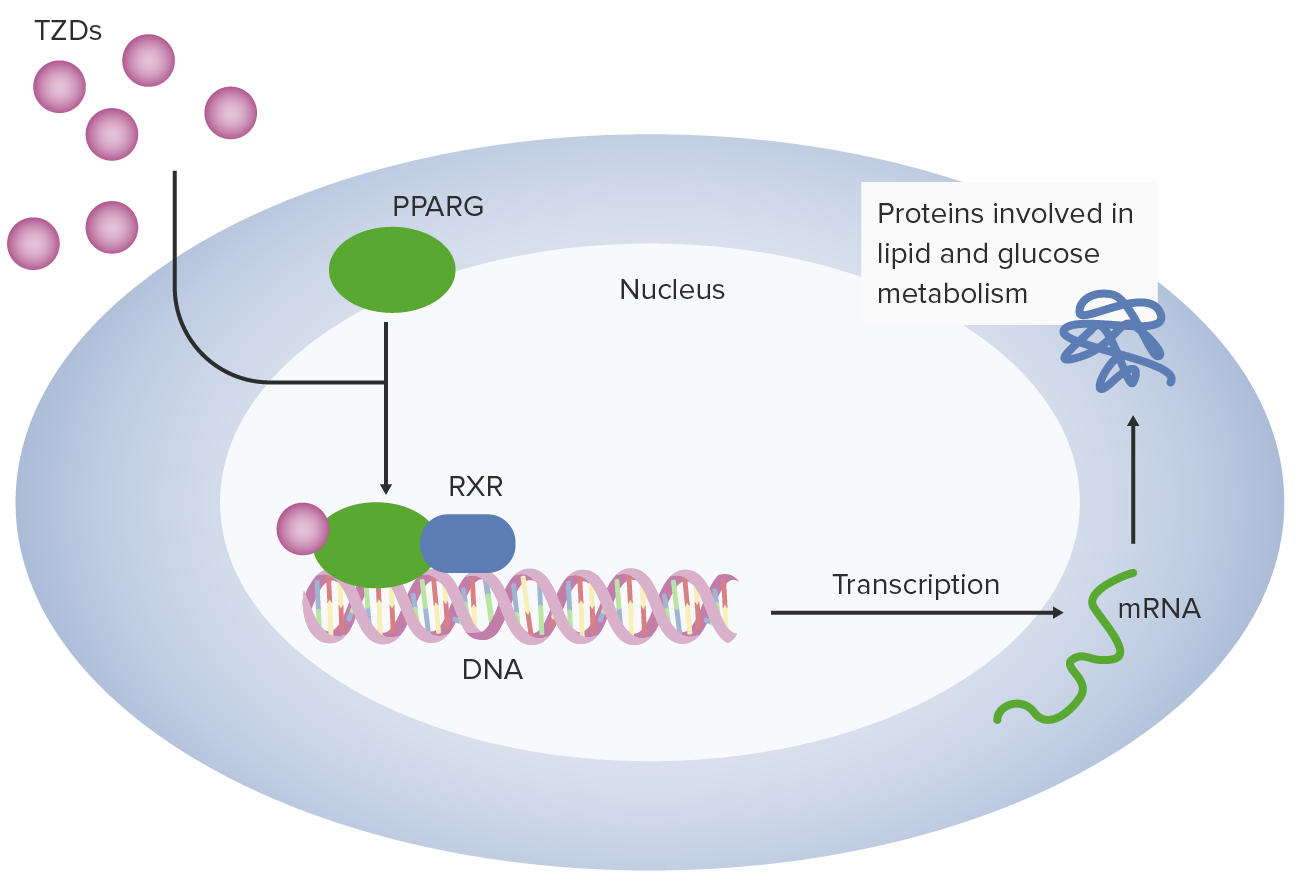
- Addition of a thiazolidinedione
- Replacement of metformin with a sulfonylureas
- Replacement of metformin with a thiazolidinedione
Which of the following A1C values is most appropriate in most adults with type 2 diabetes?
- ≤ 7.0 percent
- ≤ 7.5 percent
- ≤ 6.5 percent
- ≤ 6.0 percent
- ≤ 5.5 percent
Which of the following is the most appropriate starting dose of basal insulin like NPH, detemir, or glargine?
- 0.3 units/kg/day
- 3 units/day
- 3 units/kg/day
- 1 unit/kg/day
- 1 unit/day
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very detailed and covered all vital areas example Do and tx modalaties