Playlist
Show Playlist
Hide Playlist
Immune Response to Tumors: Tumor Antigens and Antitumor Immunity
-
Slides Tumor Immunology.pdf
-
Reference List Immune System.pdf
-
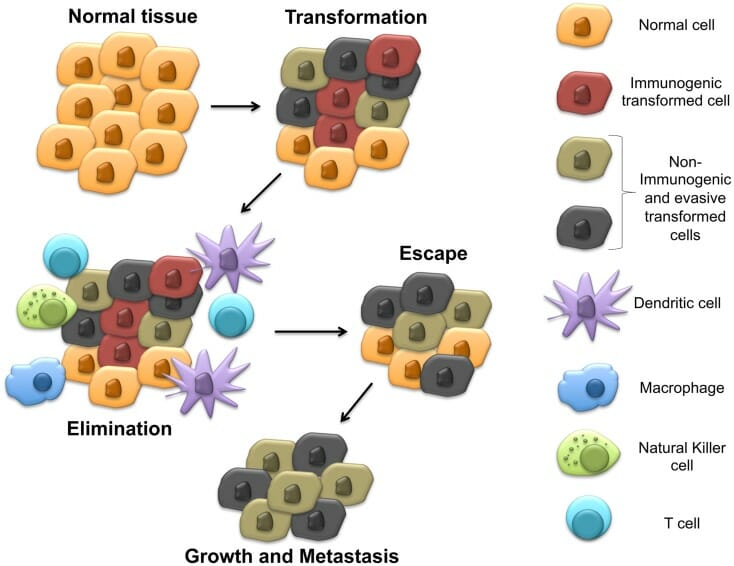
Download Lecture Overview
00:01 So let’s turn now away from tumors of the immune system itself, and ask the question - does the immune system naturally prevent or attack cancers? Well the answer is yes, but perhaps only for certain cancers. 00:20 So what is the evidence that the immune system can actually recognize and attack cancers. 00:26 Well there’s an increased incidence of certain cancers in patients with immunodeficiency, including immunosuppressed transplant patients as we’ve just mentioned. 00:38 The term immunosurveillance is used. This relates to the concept that cells of the immune system patrol around the body looking for cells that have become abnormal through malignant transformation. 00:46 This is part of a broader process called cancer immunoediting, which includes elimination, equilibrium, and escape phases. 00:52 This is part of a broader process called cancer immunoediting, which includes elimination, equilibrium, and escape phases. 01:02 Certainly the immune system can prevent tumors that are linked to oncogenic pathogens. 01:08 And it’s now known that a number of organisms can trigger the development of tumors. 01:14 So for example, the virus HTLV1 (Human T-cell Leukemia Virus-1) as the name suggests, is responsible for inducing T-cell leukemia. 01:26 Epstein-Barr virus can trigger a number of tumors including Burkitt’s lymphoma, nasopharyngeal carcinoma and post-transplant lymphoma. 01:37 The Human Papilloma viruses, particularly types 16 and 18, are responsible for triggering several cancers, including cervical, penile, anal, vulvar, vaginal, and a growing number of head and neck cancers, especially oropharyngeal cancer. Hepatitis B virus and Hepatitis C virus are linked to the development of liver cancer. 02:01 And the bacterium Helicobacter pylori can trigger the development of stomach cancer. 02:07 So it’s quite clear in these kind of situations where infectious agents are linked to the development of a tumor. 02:14 And after all the immune response has developed, has evolved to fight infectious agents. 02:19 One can see a clear potential role for the immune system in this kind of situation. 02:28 The term tumor antigen is used to describe antigens that are associated with tumor cells. 02:35 Remember, tumors are derived from normal cells. 02:42 Tumor-associated antigens are antigens that are present either in or on normal cells. 02:51 And the immune system will normally be tolerant to such antigens, because they’re normal self antigens. 02:59 In contrast, tumor-specific antigens are restricted to tumor cells, and the immune system may well not be tolerant to such antigens; perhaps arising by mutations in a gene that then encodes a different form of a protein to which the individual has not been made immunologically tolerant. 03:24 There are a number of different types of tumor antigen. 03:29 Some of the products have mutated oncogenes or tumor suppressor genes. 03:33 Examples of ongogene products include RAS mutations that are seen in around about 10% of human carcinomas, the p210 product of the Bcr/Abl rearrangements that can occur in chronic myeloid leukemia. 03:49 And mutations of tumor suppressor gene products, such a p53 mutations which are present in around about 50% of human tumors. 04:00 There are also tumor antigens that are unmutated but overexpressed products of oncogenes. 04:07 The HER2/Neu antigen is a good example of this that is seen in breast and other carcinomas. 04:15 Mutated forms of cellular genes that are not themselves actually involved in tumorigenesis, can act as tumor antigens. 04:22 For example, various mutated proteins that are found in melanomas that are recognized by cytotoxic T-lymphocytes. 04:30 And then we also have the products of genes that are silent in most normal tissues. 04:36 For example, the cancer/testis antigens expressed in melanomas and many carcinomas. 04:41 These antigens are normally expressed mainly in the testis and placenta, but can get expressed in tumor cells. 04:49 Tumor antigens can also be normal non-oncogenic proteins that are overexpressed in tumor cells. 04:56 For example, tyrosinase, gp100, and the MART antigens that are found in melanomas and are normally expressed in melanocytes. 05:07 They can be the products of oncogenic viruses. 05:10 For example, the papilloma virus E6 and E7 proteins that are associated with cervical carcinomas. 05:17 EBNA-1 protein of Epstein-Barr virus, present in EBV-associated lymphomas and in nasopharyngeal carcinoma. 05:27 Oncofetal antigens, such as the carcinoembryonic antigen that’s present in many tumors, and also expressed in liver and other tissues during inflammation. 05:39 And another example of an oncofetal antigen is alphafetoprotein. 05:45 Glycolipids and glycoproteins can also act as tumor antigens. 05:49 For example, the GM2 and GD2 antigens on melanomas. 05:56 And then finally, differentiation antigens that are normally present in the tissue of origin. 06:01 For example, the prostate specific antigen (PSA) present in prostate carcinomas. 06:07 And another example here would be CD20 on B-cell lymphomas. 06:12 Anti-tumor immunity is essentially the same kinds of responses that we see against infectious agents. 06:19 So antibody together with complement, the antibody can bind to tumor antigens present on the surface of the tumor cell, activate complement. 06:30 And the membrane attack complex can destroy the tumor cell. 06:34 Antibody dependant cellular cytotoxicity (ADCC), again an antibody against a tumor antigen expressed on the surface of the tumor cell can be recognized by cells that are capable of mediating ADCC. 06:51 We call such cells, killer cells; really they can be any cell in the immune system that has an Fc receptor and also is able to fuse toxic molecules. 07:00 And specific immune cells that express Fc receptors, particularly NK cells, macrophages, and neutrophils, can carry out this function of ADCC. 07:11 There can be direct natural killer cell cytotoxicity, where the killer activating receptors on the surface of natural killer cells recognize ligands on the surface of the tumor cell. 07:26 And finally there can be cytotoxic T-cells which recognize tumor-derived peptides presented by MHC Class I molecules. 07:36 It’s very clear that immune system cells are naturally present within tumors. 07:41 We can find T-cells, natural killer cells, macrophages, also regulatory T-cells and myeloid derived suppressor cells within tumors. 07:56 So T-cells, natural killer cells and macrophages potentially could mediate a beneficial anti-tumor response. 08:04 One of the problems is that very often, these other cell types, such as regulatory T-cells and myeloid derived suppressor cells actually dampen down the anti-tumor response. 08:18 As will be discussed in more detail shortly, In recent years, our understanding of tumor immunity has led to breakthrough therapies called immune checkpoint inhibitors. 08:29 Tumors often evade immune destruction by expressing molecules like PD-L1 or by influencing T cells to express inhibitory receptors like PD-1 and CTLA-4. 08:42 Drugs that block these immune checkpoints have shown remarkable success in treating multiple cancer types including melanoma, lung cancer, and many others.
About the Lecture
The lecture Immune Response to Tumors: Tumor Antigens and Antitumor Immunity by Peter Delves, PhD is from the course Tumor Immunology. It contains the following chapters:
- The Immune Response to Tumors
- Tumor Antigens
- Anti-Tumor Immunity
Included Quiz Questions
Which of the following are the most common types of effector cells in antibody-dependent cellular cytotoxicity?
- Natural killer cells
- Erythrocytes
- B lymphocytes
- T lymphocytes
- Plasma cells
Which type of cancer is INCORRECTLY matched to the associated pathogen?
- Lung cancer - human papillomavirus 16
- Gastric cancer - Helicobacter pylori
- Liver cancer - hepatitis B virus
- Burkitt's Lymphoma - Epstein–Barr virus
- T-cell leukemia - human T-cell lymphotropic virus type 1
Which of the following tumor antigens are products of mutated oncogenes?
- BCR/ABL rearrangement in chronic myeloid leukemia
- Tyrosinase in melanoma
- gp100 in melanoma
- HER2 in breast cancer
- Papillomavirus proteins in cervical cancer
Which of the following immune cells originate from the myeloid lineage and possess strong immunosuppressive activities?
- Myeloid-derived suppressor cells
- T cells
- Natural killer cells
- Macrophages
- Neutrophils
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
very nice and descriptive information regarding the tumor immunology, it has helped a lot