Playlist
Show Playlist
Hide Playlist
IgA Vasculitis (Henoch-Schönlein)
-
Slides Vasculitis.pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
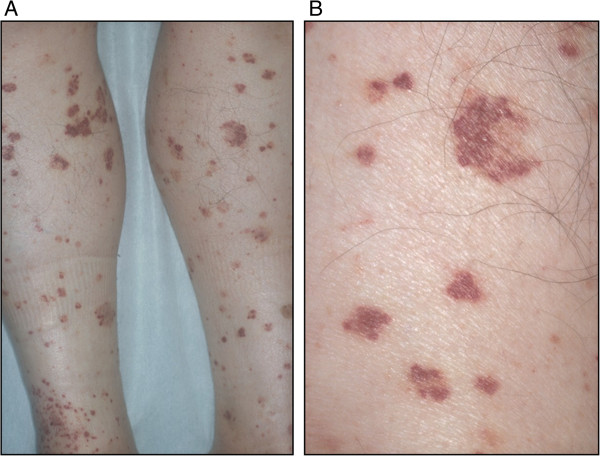
00:00 I think based on the process of elimination, I'm thinking we got a winner here, but let's take a look back at the case, get some blood work and see if IgA vasculitis, which we haven't even talked about yet, is going to be our diagnosis. Alright, so 14-year-old girl. Just to refresh your memory, we already learned that IgA vasculitis, previously known as Henoch-Schönlein purpura is an immune-mediated small vessel vasculitis that unlike the ANCA-associated vasculitis is going to have significant immune complex deposition in tissues. So, let's talk about the specific features of this case that go along with this diagnosis. So her age of being 14 is the classic age point for Henoch-Schönlein purpura IgA vasculitis. As you can see, most common ages are between 3 and 15 years of age. Interestingly enough, it's often preceded by a strep throat infection and this may be due to some sort of molecular mimicry type picture so the time course of days to weeks of prior strep infection would be consistent with this diagnosis as well. When looking at the systems that are involved, we have skin involvement, we have GI involvement, we have arthralgias, in fact about 65% of patients with IgA vasculitis will have an arthritis or arthralgia, more of the arthralgias without as much evidence of a sinovitis on exam. And importantly some things that are absent may also help us out here. She doesn't have any ocular symptoms, she doesn't have any cardiopulmonary symptoms, she doesn't have any constitutional symptoms and that turns out to be significant. Cardiopulmonary stuff without pulmonary symptoms were certainly weaning away from a lot of those ANCA-associated vasculitides as well. Back to the physical exam, the absence of any oropharyngeal lesions like red lips or strawberry tongue is going to lead us away from something like Kawasaki's and thinking back to our large vessel vasculitides the absence of any systemic blood pressure discrepancies, there's no carotid bruit, that's going to stir us away from Takayasu's for example. She is diffusely tender to moderate palpation on exam and has guaiac positivity. We're certainly concerned about either submucosal edema of the intestines or perhaps hemorrhage or ischemia and then as I mentioned an oligoarticular arthralgias would be consistent with this diagnosis as well. Lastly, on the skin exam, if you do a biopsy you're probably going to find a leukocytoclastic vasculitis particularly in the dependent areas down the lower legs and feet. Alright, so let's review the labs here. We have mild anemia, very nonspecific; a leukocytosis, same thing. Creatinine looks okay but she does have 1+ protein, 1+ RBCs so it does look like there is at least mild renal involvement. There are no casts that we're seeing and the creatinine is okay. So, there wouldn't be any really compelling reason to get a kidney biopsy at this point, but if you did you might see this in about a third of patients with IgA vasculitis, you might find mild to severe crescentic glomerulonephritis with this pathognomonic IgA deposition in the mesangium on immunofluorescence. Take note that in this particular glomerulus, it's not particularly hypercellular but it clearly is staining very strong for IgA throughout the mesangium. Lastly, her serum IgA is elevated. That can be a marker of IgA vasculitis, no surprise there. And again, the skin biopsy would be what we've talked about in the past though as an immune complex mediated small vessel vasculitis, you ought to find some IgA actually deposited in your specimen. Alright, there you have it. With a 14-year-old girl presenting with fairly acute onset of symmetric palpable purpura, abdominal pain, and arthralgias in the absence of any constitutional symptoms or cardiopulmonary symptoms and the skin biopsy showing pathognomonic presence of IgA deposits, this is your classic illness script for IgA vasculitis. 04:21 Fortunately, treatment is actually just supportive. It is a self-remitting illness and will get better on its own. Treatment is supportive, you can use, of course you want to provide them hospital care, supportive care, hydration, you can use NSAIDs for any discomfort the patient is experiencing, rarely you would use glucocorticoids only if you have to.
About the Lecture
The lecture IgA Vasculitis (Henoch-Schönlein) by Stephen Holt, MD, MS is from the course Vasculitides.
Included Quiz Questions
Henoch-Schönlein purpura is usually associated with all of the following clinical features except…?
- ...conjunctival injection.
- ...arthralgias.
- ...IgA nephropathy.
- ...abdominal pain.
- ...lower extremity purpura.
Which of the following is the most appropriate treatment for Henoch-Schönlein purpura?
- Supportive care
- Plasmapheresis
- Intravenous immunoglobulin
- Methotrexate
- Cyclophosphamide
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |