Playlist
Show Playlist
Hide Playlist
Hypothyroidism in Children
-
Slides Thyroiddisorders Pediatrics.pdf
-
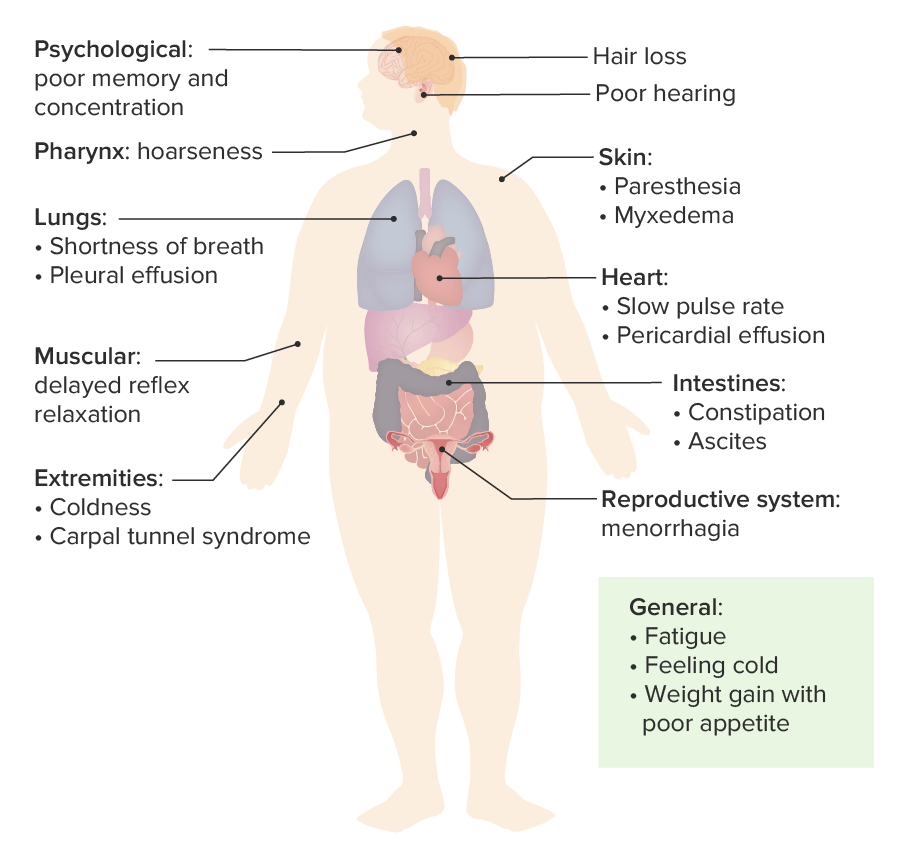
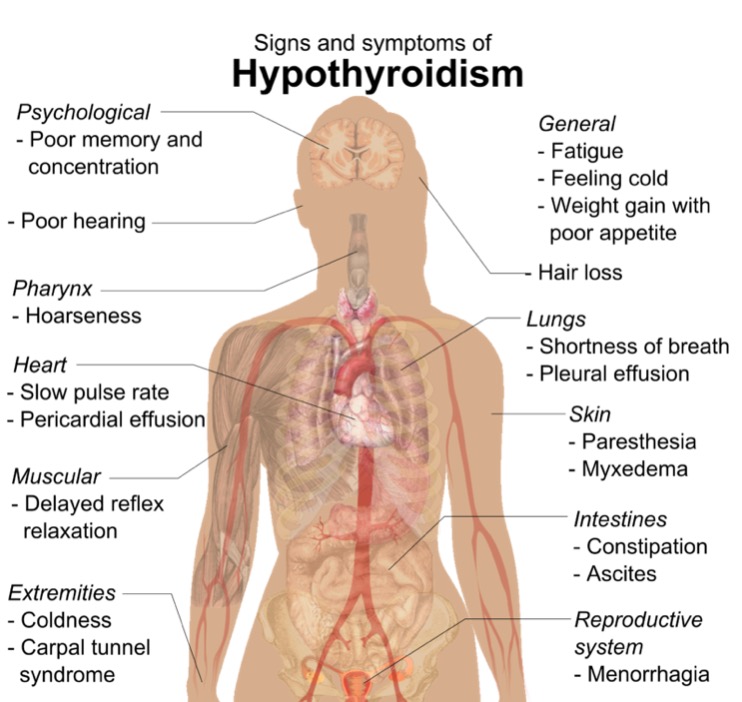
Download Lecture Overview
00:02 Let's switch gears and go to hypothyroidism, when we have not enough thyroid hormone. 00:08 Primary hypothyroidism, an inability of the actual thyroid gland to make enough thyroid is more common. 00:16 Secondary, with the stimulus, the TSH is not high enough, but the thyroid hormone is essentially normal, is rare in children. 00:26 So, probably the most common encounter where we see patients with hypothyroidism in pediatrics, is in the perinatal period, when we see patients with congenital hypothyroidism. 00:38 Because this is so common, this is on the newborn screen across the United States. 00:45 It's on the newborn screen, because rapid intervention can have a profound effect in the long term outcome of these patients. 00:52 This occurs in about 1 in 3,000 babies. 00:55 And mostly, it's a primary disease, with an absent or malformed thyroid, that's about 85% of cases. 01:04 Thyroid hormone synthesis problem takes up the other 15%. 01:10 Alternatively, patients may have an acquired hypothyroidism. 01:16 They were born with adequate thyroid hormone, but later in life stop making it adequately. 01:23 This is actually fairly common, and more common than the congenital hypothyroidism, but there are many different causes. 01:31 So if we're looking for one cause, maybe congenital hypothyroidism is the most common. 01:36 So, what... how do patients with congenital hypothyroidism present? Well, at first there it's asymptomatic, and they're usually picked up on the newborn screen. 01:48 If for some reason a newborn screen wasn't done, or was misinterpreted, or the lab result was lost, patients will usually develop failure to thrive. 01:59 Remember, thyroid hormone is the growth hormone for that first year of life. 02:03 Patients may develop feeding problems, prolonged juandice is common, and in your differential for a jaundice baby is hypothyroidism. 02:14 Additionally, patients will get large fotanelles, the large fotanelle is concerning for hypothyroidism. 02:21 Patients may get constipated. 02:23 Remember, this is essentially the opposite of hyperthyroidism, where they get diarrhea. 02:28 They had develop coarse facies. 02:31 Coarse facies means large units such as large ears, large nose, large eyes, large chin. 02:38 They may develop macroglossia or a large tongue, as you can see in this patient here. 02:44 They develop an umbilical hernia. 02:47 Now remember, umbilical hernias are extremely common, In general, 10-20% of babies have umbilical hernias. 02:55 What is the real killer here is the developmental delay, these patients can have profound loss of ability to have normal cognitive function when they grow up. 03:06 And intervention can prevent that loss of IQ points. 03:10 It's incredibly important to intervene quickly, these patients because of the CNS toxicity will also have hypotonia. 03:18 Notice the bold things I wrote here, these are the things that are probably most likely to be on your test. 03:23 These infants develop, Failure to thrive, prolonged jaundice, a large fotanelle, and then umbilical hernia. 03:30 Those are the things we're gonna pick up early, that are really tell us we're worried about hypothyroidism in this child, maybe we should go, check with that newborn screen really show. 03:38 Later on in life with acquired hypothyroidism, patients are gonna have symptoms that are more or less the opposite of the hyperthyroid patient. 03:47 They may have fatigue, decreased activity, cold intolerance, constipation, they'll have dry skin, and the unique one is hair loss. 03:58 On exam, you may find a goiter, and again, remember how to do that exam. 04:04 You will show a slowing of linear growth. 04:07 These patients may have a delay, and when their teeth come in. 04:11 You'll notice coarse features on their face and we discussed what those were earlier. 04:16 You will notice they have slowed mental activity and slowed physical activity. 04:22 And puberty is quietly frequently delayed in acquired hypothyroidism if the problem happens prior to puberty. 04:31 So how are we gonna test for hypothyroidism if we suspect it? Let's look at how these labs come out in various types of hypothyroidism. 04:40 So when a patient who has primary hypothyroidism, the thyroid gland just isn't working. 04:46 However, the signals going to that thyroid are, a patient will have a low total and low free T4 and the high TSH. 04:55 There is no negative feedback going on, we may also detect antibodies against the thyroid in patients with autoimmune disease. 05:03 In a patient with secondary hypothyroidism, the problem is really the lack of TSH or the inadequate over responsive TSH. 05:15 So the total T4 and free T4 would be down, the TSH maybe low or maybe even just low normal when it should be high in the phase of a low Free T4. 05:29 Sick euthyroid syndrome is when a patient has an abnormal thyroid labs, but they are in fact euthyroid, that is to say they're not yet having a problem with their T4. 05:45 So these patients may have a slightly low or normal T4 that's total but their free T4 is normal and their TSH is normal. 05:54 These patients may also have low T3 or a high reverse T3. 05:59 If a patient had thyroid binding globulin deficiency or TBG deficiency, that's when we would see that low total T4, but a normal free T4 and a normal TSH. 06:12 The patient isn't truly hypothyroidism. 06:14 This, we can also test for actual TBG levels and those would abviously be decreased. 06:22 So in addition to checking labs, we probably wanna image that thyroid gland. 06:26 The way we would start is by ultrasound, it tells the size structure and tells us whether there's a presence of nodules. 06:34 We can use it to check for nodules or goiter. 06:37 Remember, autoimmune thyroiditis has a typical pattern of goiter and micronodules, and the ultrasound may give us a clue into that. 06:47 Also, we can do a thyroid nuclear scan, which should show poor activity of the thyroid, but the mainstaying test, mainstay test is the ultrasound. 06:57 If we're going to treat hypothyroidism, we're gonna start with levothyroxine, which is essentially oral T4. 07:04 We dose this once daily, generally 30 minutes before food, so that we can promote absorption. 07:12 That's about all I have for you for hyper and hypothyroidism. 07:18 Thanks for your attention.
About the Lecture
The lecture Hypothyroidism in Children by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Hypothyroidism: Pathology
- Clinical Presentation
- Diagnosis & Management
Included Quiz Questions
Which of the following is NOT a clinical sign of congenital hypothyroidism?
- Tachycardia
- Large fontanelles
- Macroglossia
- Coarse facies
- Constipation
A 20-week-old child is brought to the clinic by his parents indicating he is not feeding well. The infant has a history of neonatal jaundice and delayed developmental milestones. On examination, he appears weak and hypotonic. Which of the following is the next best step?
- Test for serum thyroid hormone and TSH levels.
- The child must be admitted to the pediatric ward.
- Reassure the parents.
- Start Ryle’ s tube feeding.
- Request a urinalysis.
You request thyroid function labs for a child with suspected thyroid abnormalities. The following results are received: total T4- decreased, free T4- normal, TSH- normal. Which of the following is the most likely diagnosis?
- TBG deficiency
- Primary hypothyroidism
- Pituitary adenoma
- Secondary hypothyroidism
- Graves' disease
A child with suspected thyroid abnormalities suggested by clinical symptoms and lab values undergoes an ultrasound of the neck. The report indicates micronodules along with thyroid swelling. Which of the following is the most likely diagnosis?
- Autoimmune thyroiditis
- Toxic adenoma
- Multinodular goiter
- Sick euthyroid syndrome
- Thyroid malignancy
A child diagnosed with primary hypothyroidism was treated with oral levothyroxine once daily. What additional advice should be given to the child's caregiver?
- Take the tablet 30 min before food.
- Repeat thyroid scan 3 weeks later.
- In case of palpitations or tremors, increase the dose of the levothyroxine.
- Always take this tablet along with other nutrient supplements.
- Alternate levothyroxine with methimazole for the first three months.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture! Very clear, easy to understand, easy to remember. Thanks!