Playlist
Show Playlist
Hide Playlist
Hyperthyroidism in Children
-
Slides Thyroiddisorders Pediatrics.pdf
-
Download Lecture Overview
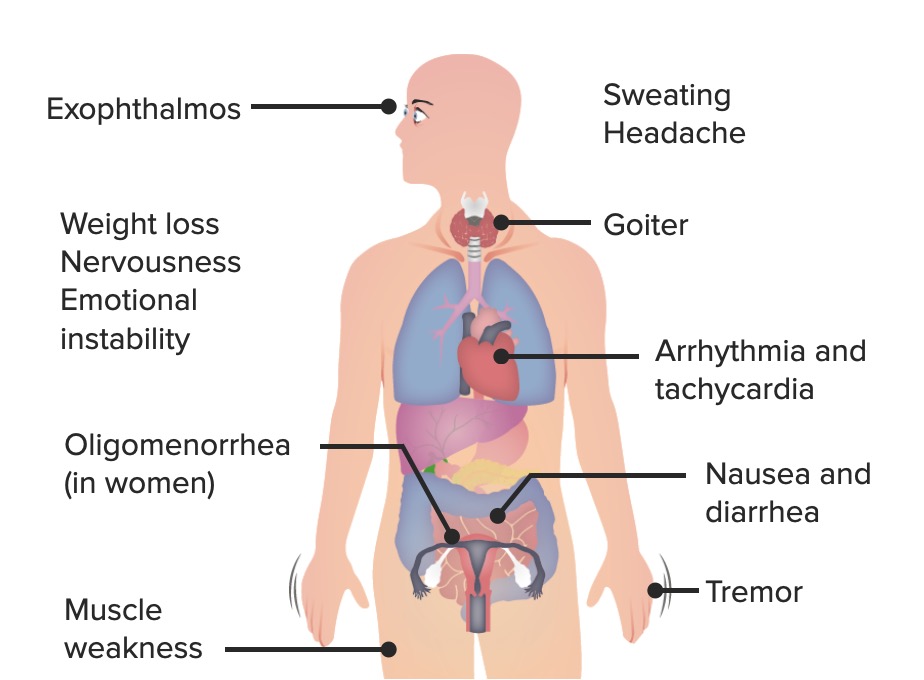
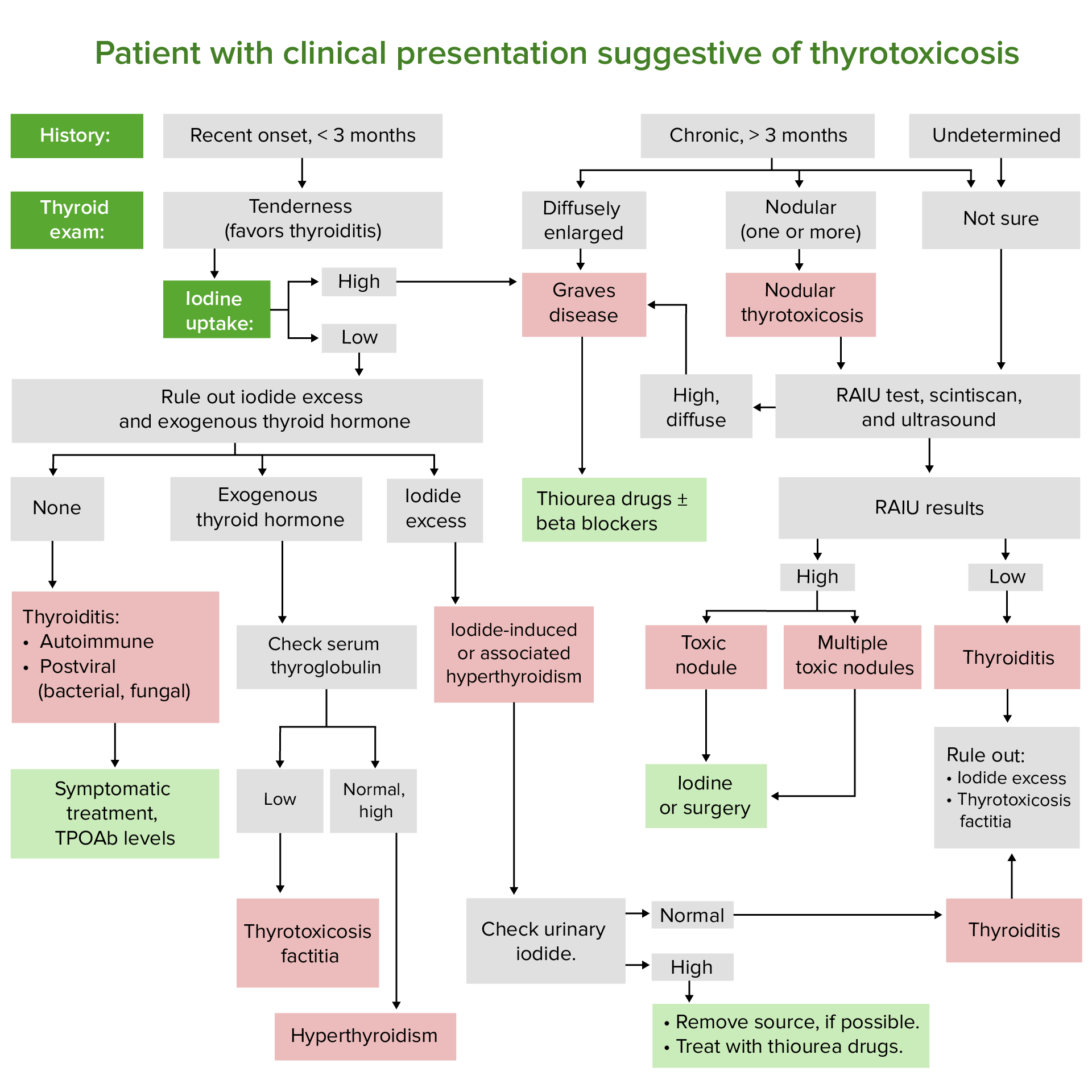
00:01 In this lecture we're going to talk about hypothyroidism and hyperthyroidism in children. 00:07 Let's start with hyperthyroidism. 00:10 So there are many causes of hyperthyroidism in children. 00:15 By far, the most common is the autoimmune disease, Grave's disease. 00:19 Where patient's are having antibodies directed against their thyroid that are causing the thyroid to spit out too much thyroid hormone. 00:27 Also, patients might have Hashimoto's Thyroiditis, and in the early phases, they can have a toxic effect where there is an excessive excretion called Hashitoxicosis, certainly that could be causing hyperthyroidism in children as well. 00:43 Subacute thyroiditis is seen, it's usually cause by viruses and usually it's a more mild malingering sort of condition. 00:52 The toxic nodule is possible, we sometimes see this in patients where there is one nodule that just secreting quiet a bit of thyroid hormone. 01:01 Multinodular goiter is possible in children, we see that more commonly in people with certain conditions such as McCune-Albright. 01:10 Certain drugs can cause hyperthyroidism, of course we think of things like excessive iodine or excessive thyroid hormone medication. 01:20 Very rarely a patient can have a TSH producing adenoma, which cause a secondary hyperthyroidism in a child. 01:29 After radiation therapy for thyrotoxicosis, patients can be transiently hyperthyroid. 01:35 And very rarely, patients can have a selective pituitary thyroid resistance, so when that feedback loop, the pituitary doesn't respond to specifically T3, and does there's an excessive production of TSH, which is then stimulating the thyroid hormone to make more thyroid. 01:55 So let's focus however on Grave's disease, which is our most common cause of this condition. 02:01 Grave's disease is an autoimmune attack of the TSH receptors on thyroid follicular cells. 02:08 It can be associated with other autoimmune diseases such as myasthenia gravis, diabetes, or Addison's disease. 02:17 It's more common in girls than it is in boys, and there is a familial disposition. 02:23 In other words, if it runs in the family the child is at risk for it too. 02:28 So the symptoms of hyperthyroidism as you expect, include anxiety and restlessness. 02:34 They include an increased appetite. 02:37 These patients will have sweating, diarrhea, and perhaps some weight loss. 02:42 There maybe a rapid growth in height, especially in that first year of life when thyroid hormone is one of the premier factors in how children grow rather than growth hormone. 02:54 Patients typically will have tremor and tachycardia as a side effect. 02:59 And on exam you may feel a goiter. 03:02 Remember the best way to palpate a thyroid gland is from behind with both fingers over the thyroid and then ask the patient to swallow. 03:13 So, on exam we will see exopthalmos sometimes but that's really is more common in adults. 03:21 However, if you see bilateral exopthalmos, that's likely to be hyperthyroidism. 03:29 Remember, this condition can be permanent, so we want to correct the condition before we encounter the exopthalmos. 03:36 Also remember unilateral exophthalmos is unlikely to be thyroid disease, but it's more likely to be a mass or a tumor such as seen in neurofibromatosis. 03:48 Symptoms and severe cases of hyperthyroidism include behavioral problems, psychosis, and also patients can have a thyrotoxic crisis which is essentially being so ramped up that their vital signs are abnormally affected and they may develop shock. 04:08 So hyperthyroidism, to understand it and to diagnose, we should understand the basics of the thyroid gland. 04:14 Remember, the pituitary makes thyroid stimulating hormone, which then convinces the thyroid to start making free T4. 04:24 The T4 then goes up and inhibits the pituitary in a negative feedback loop to prevent excessive thyroid production. 04:33 So when we suspect thyroid and hyperthyroidism, we're going to check both a TSH and a free T4, or more commonly, we'll just check a TSH first. 04:46 If that's low, then we'll reflexively check a T4, and if that's high, we've sense the diagnosis. 04:53 The total T4 includes both the bioactive component of T4 called the free T4 and the T4 that's bound and is not bioactive. 05:06 You may see the phrase, free T4 by dialysis or free T4. 05:13 And that's the best way to measure what is free T4. 05:16 The dialysis were first how they do the test in the lab, it has nothing to do whether the patient is on dialysis. 05:24 So, if you suspect hyperthyroidism, we're going to get that TSH and we're gonna get a T4. 05:30 We can also get a free T3 and under certain circumstances that maybe beneficial. 05:36 Imaging, if we suspect hyperthyroidism and we think it's the thyroid gland itself we'll wanna image that thyroid gland. 05:44 We can use a radionuclide scan to look for activity of the gland using radioactive iodine. 05:51 Increased uptake for, occurs in hyperthyroidism from Grave's. 05:58 Decreased uptake for destruction-mediated hyperthyroidism is seen such as radiation or thyroiditis. 06:06 And a hot nodule will show up specifically toxic nodular disease, so the scan can really be helpful in distinguishing the cause. 06:15 Typically, in patients with hyperthyroidism we're gonna manage some of their symptoms with betablockers, and this is a high yield fact for your exam. 06:23 The beta blockers will block a lot of the symptomalogic response of being hyperthyroid. 06:29 So if a patient is profoundly hyperthyroid, we start off with beta blockers while we then proceed to figure out what's going on and how to manage this condition more thoroughly. 06:39 We can also use thionamides as a way to control their hyperthyroidism. 06:44 Specifically, methimazole is generally our first line agent. 06:48 Outisde of the United States, some people use carbimazole, but that is not accepted in the United States by the FDA at this time. 06:55 We treat to normalize the T4 and the TSH, so we're gonna continue get titers and find the place where this child should be. 07:05 In about 30% of patients will go into remission using methimazole. 07:11 Iodine has a fast onset of action and is really used for the thyroid storm. 07:19 We're gonna use that to basically prepare for the patient to go to surgery, we want that patient to be iodine-replete, when they go to surgery to prevent the thyroid storm. 07:33 Radioactive iodine, this is another way to treat hyperthyroidism. 07:39 It goes directly to the thyroid, and it essentially irradiates the gland and the area where there's excessive production. 07:47 This is useful for Grave's disease, and also for a toxic nodule. 07:51 However, the side effect ironically can be hyperthyroidism, and a thyroiditis 2 to 3 weeks later. 08:00 They also can get hypothyroidism 2 to 4 months later, and they may require a second dose. 08:08 And for all these reasons, this is not our first line agent for management of this condition. 08:13 Some patients will have a surgical excision for their hyperthyroidism. 08:18 This is generally indicated with a toxic nodule, and in other selected cases of Grave's disease that were having a hard time controlling, where conservative treatment it doesn't seem to be working. 08:32 The reason we like to limit our surgical excisions, is that a large resection can result in a lifelong hypothyroidism and need for taking synthetic thyroid hormone for the rest of their lives. 08:46 Again, before we have the surgery, we're going to give iodine and make the patient euthyroid so as to prevent a post-operative thyroid storm.
About the Lecture
The lecture Hyperthyroidism in Children by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Hyperthyroidism: Pathology
- Clinical Presentation
- Diagnosis
- Management
Included Quiz Questions
What is the etiology of Graves' disease?
- Autoimmune attack on the TSH receptors present on thyroid follicular cells
- Autoimmune attack of the parafollicular cells
- Destruction of the TSH receptors on the parafollicular cells as a consequence of thyroiditis
- Autoimmune injury to the pituitary resulting in decreased TSH
- Hyperplasia of the thyroid follicular cells resulting in increased hormone production.
Which of the following is the first-line agent for hyperthyroidism in children in the US?
- Methimazole
- Carbimazole
- Radiation therapy
- Iodine
- Methotrexate
Which of the following is NOT seen in children with hyperthyroidism?
- Weight gain
- Sweating
- Restlessness
- Rapid growth in height
- Increased appetite
Which of the following is NOT true regarding hyperthyroidism in children?
- Exophthalmos occurs as commonly as in adults.
- Severe hyperthyroidism presents with behavioral problems, psychosis and thyrotoxic crisis.
- The TSH is low while free T4 is high.
- Radionuclide scanning can be used to know the functional status of the gland.
- Graves' disease is more common in girls as compared to boys.
A child is brought to the clinic with symptoms of hyperthyroidism. On radionuclide scan, there is decreased uptake of I¹²⁵. What is the most likely diagnosis?
- Thyroiditis
- Graves' disease
- Toxic nodular goiter
- Thyroid carcinoma
- Toxic adenoma
A 10-year-old child is brought into the clinic with complaints of severe sweating, diarrhea, and visible tremors of his hands. On physical examination, there is a 2 x 2 cm nodule in the left lobe of the thyroid gland. His vital signs are normal except for his heart rate which is 130 beats per minute. What is the first drug that should be given to this patient?
- A beta-blocker
- Methimazole
- Carbimazole
- Iodine
- Radioactive iodine
Which of the following statements is TRUE regarding the management of hyperthyroidism?
- The main goal of treatment is to normalize T4 and TSH levels.
- Thionamides result in a 100 percent remission.
- Beta-blockers regulate the thyroid hormone levels by inhibiting excessive production.
- Iodine is used as the first-line agent due to its fast onset of action.
- Methimazole is the most common agent used to prevent postoperative thyroid storm.
Which of the following is a complication of radioactive iodine?
- It can cause thyroiditis 2-3 weeks later.
- It may require more than 6 doses to achieve the desired result.
- It can only be used in Graves' disease.
- It can result in hypothyroidism 2-4 weeks later.
- It targets any glandular tissue in the body indiscriminately.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture: comprehensive, clear, easy to remember. Contains all the necessary information for the primary care provider. Thanks!
Simple and high-yield explanation to a commonly encountered topic in both pediatrics and internal medicine.