Playlist
Show Playlist
Hide Playlist
Hypertension: Etiology (Neural Blood Pressure Control Mechanisms)
-
Slides 06 VascularMedicine advanced.pdf
-
Reference List Vascular Medicine.pdf
-
Download Lecture Overview
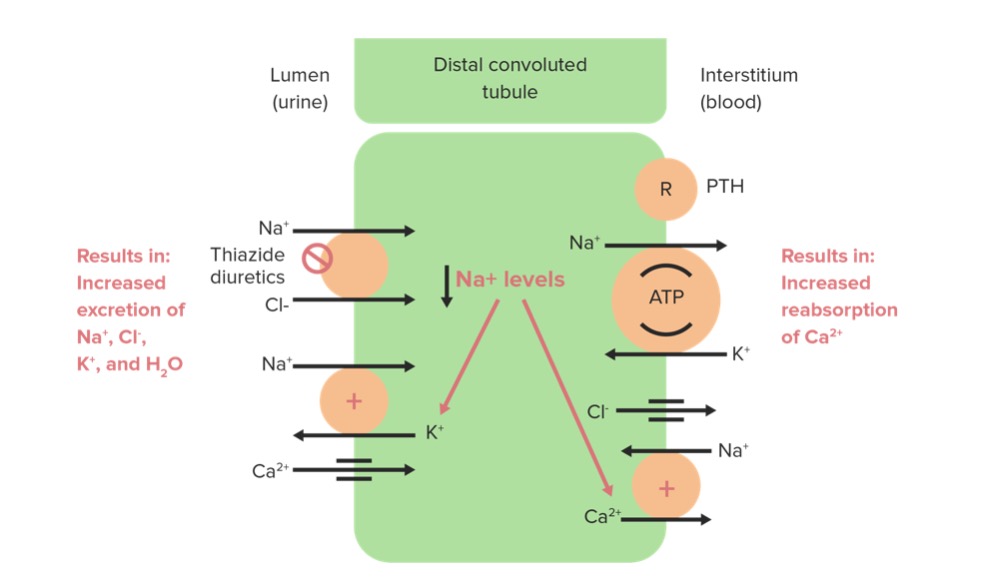
00:01 So we’re going to talk about the causes, the underlying abnormal physiology that leads to hypertension. The so-called etiology. 00:12 In order to do this, we need to get some understanding as to how the body controls blood pressure. 00:18 Obviously, blood pressure control is critical because you want a nice, smooth blood pressure and a smooth distribution of the blood to all of the cells of the body. So this is a very tightly-controlled and regulated system. 00:33 There are two mechanisms that are involved in the control of blood pressure. There is a neural – that is a central nervous system set of mechanisms. And there is a hormonal system. We’re going to talk first about the neural mechanisms. 00:49 The neural mechanisms are centred in the brain. Not surprising! The brain controls all kinds of our activities. As you know, it has ways of controlling our digestion, our blood pressure, our sleeping and waking and so forth. 01:04 So what we see in the brain that is part of the control system for blood pressure? First of all, there is the autonomic nervous system with the sympathetic nervous system playing a major role in blood-pressure control. 01:22 The sympathetic nervous system is the part of the nervous system that controls the release of adrenaline or noradrenaline from nerve endings throughout the body. And remember when you release this hormone, it causes vasoconstriction – that is contraction in the smooth muscle in the arterioles and that increases peripheral vascular resistance. 01:46 So a major determinant of peripheral resistance and therefore blood pressure is the sympathetic nervous system. 01:56 Another factor that is widely spread throughout the arterial system are so-called baroreceptors. 02:02 These are pressure-sensitive cells that send signals to the brain to say what the blood pressure is. Is the blood pressure too low? Is the blood pressure too high? Or is the blood pressure just right? I think of them sort of like thermostats in our house when we set the temperature that we want the room to be. Well the baroreceptors are part of that thermostat system but they’re not measuring heat. They’re measuring pressure. 02:31 And there is a hormone that is released from the pituitary gland in the brain that decreases the release of fluid by the kidney: the so-called antidiuretic hormone, often abbreviated ADH. 02:48 This is a hormone that developed evolutionarily over many, many millions of years. And it protects animals who live on land from dehydration or if there’s a hemorrhage. So if you lose volume in your circulatory system either because you’re dehydrated or because you’re bleeding, the body has all kinds of mechanisms to preserve fluid in the vascular system. And one of them is to say, “Kidneys! Stop making urine. We want to hold onto the fluid.” And that’s organized by the pituitary. 03:22 Now you can imagine the thermostat in the brain that’s receiving signals from the baroreceptors is also going to be helping to control the release of antidiuretic hormone. 03:32 That’s just one factor by the way in the neural-mechanism system. And we’re going to look at some others right now. 03:42 This diagram seems to be a little bit complicated but let’s work our way through it here and you can see. 03:49 This is for control of arterial blood pressure. We already talked about cardiac output and heart rate. If you push up the cardiac output against no change in resistance, you’re going to increase the blood pressure. But the major control of blood pressure is not so much in terms of changing cardiac output. It’s in changing, as I’ve said before, peripheral vascular resistance. And you see, over on the right of the diagram, sympathetic nervous activity is often the major factor controlling the arterial wall constriction or dilation that increases or decreases peripheral vascular resistance. 04:25 The other component of the autonomic nervous system – the vagus or parasympathetic part – also has some vasodilating effects but the major control of the arterioles is with the sympathetic rather than the parasympathetic part of the autonomic nervous system. 04:42 And then of course blood volume and salt and water retention are all involved in controlling the amount of volume in the cardiovascular system and therefore contribute to the pressure in the system. 04:59 Think of it this way: suppose we have a certain volume of blood that’s circulating and we suddenly double it. What’s going to happen in the system if the system doesn’t enlarge in any way? Blood pressure is going to go up because, suddenly, there’s twice as much volume travelling in a system that hasn’t changed in size. 05:16 The kidney plays a major, major role in blood pressure control and you see that down at the bottom there of the diagram. That’s a little cartoon of the kidney. 05:26 The kidney has a number of hormones and we’re going to talk about this more in detail on subsequent slides. But a number of hormones can be released by the kidney that have effects on blood pressure. The most important one is the renin that we talked about when I mentioned the Goldblatt kidney in the last lecture. When there’s an abnormal flow into the kidney, the kidney responds to this by releasing a hormone called renin. 05:54 Renin gets into the circulation, goes through a series of chemical reactions. That produces a substance called angiotensin II. And angiotensin II causes marked vasoconstriction of the arterioles. 06:07 In other words, increased peripheral vascular resistance. Renin also goes to the adrenal glands and causes the adrenal glands to release a hormone called aldosterone. And aldosterone feeds back to the kidney and says, “Hold on to sodium! Hold on to sodium!” At the same time, antidiuretic hormones being released by the pituitary and that says, “Hold on to water!” So the kidney’s getting a signal from a hormone from the adrenal glands and a signal from a hormone from the pituitary gland that say, “Hold on to salt and water!” And you can see that in the diagram: a little red arrow there to the left says: salt and water is retained. That increases blood volume. That increases venous return. And that may help to increase blood pressure. 06:55 And all of this system was set up to help animals survive in periods of dehydration or when there’s blood loss. Unfortunately, sometimes in this system the thermostat is not set right and, in those patients, the system is working even when the blood pressure is normal and, consequently, peripheral resistance goes up and, consequently, blood pressure goes up and those patients are hypertensive. 07:21 We mentioned again that this is just further demonstration of the central nervous system: neural mechanisms for blood-pressure control. Just to review it again: the autonomic nervous system, sympathetic and parasympathetic. Parasympathetic can dilate the blood vessels a little and slow the heart rate and therefore decrease cardiac output and decrease blood pressure. But the major control factor is in the sympathetic system which causes vasoconstriction in the arterioles and increased peripheral vascular resistance. And you see all of that listed on the slide. 08:04 And you can see that the control of blood pressure relates partly to control of cardiac output. But it’s mostly related to peripheral vascular resistance which is mostly under the control of the sympathetic nervous system. 08:22 The baroreceptors are scattered throughout. You can see in this little diagram they’re particularly common in the aorta and in the carotid arteries. Interestingly enough, there are other receptors – chemoreceptors, chemical receptors – that are located with the baroreceptors and they monitor oxygen in the blood, carbon dioxide in the blood and hydrogen ions, or acidity, in the blood. And so the body is also regulating all of those and often part of the regulation there relates to increasing the respiratory rate – increasing how much, how fast you’re breathing and also regulating how much hydrogen ion – how much acid – the kidneys are putting out. 09:03 So the body has very intricate and very, very finely-tuned mechanisms for regulating the internal environment. As we talked about in the very first lecture, the homeostasis: maintaining a smooth internal environment, normal blood pressure, normal oxygen, normal carbon dioxide, normal acidity. And of course we’re talking here mostly about blood pressure regulation and how that goes wrong in some people either genetically – they have an abnormal thermostat for regulating the blood pressure in the central nervous system and they regulate it too high – or many of the secondary factors that can lead to high blood pressure. And we’re going to talk about those as we go along.
About the Lecture
The lecture Hypertension: Etiology (Neural Blood Pressure Control Mechanisms) by Joseph Alpert, MD is from the course Arterial Diseases.
Included Quiz Questions
Patients with uncontrolled chronic hypertension are least likely to develop which of the following conditions?
- Adrenal insufficiency.
- Congestive heart failure.
- Chronic renal failure.
- Stroke.
Which of the following functions is performed by adrenaline in blood pressure control?
- Vasoconstriction.
- Bradycardia.
- Vasodilation.
- Increased vascular permeability.
- Reduced vascular permeability.
Baroreceptors are cells that regulate?
- Pressure.
- Temperature.
- Oxygen density.
- Carbon dioxide density.
- Osmolality of blood.
Antidiuretic hormone controls blood pressure mainly through its effect on which of the following organs?
- Kidney.
- Heart.
- Pituitary gland.
- Endothelium of blood vessels.
- Adrenal gland.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |