Playlist
Show Playlist
Hide Playlist
Hyperlipidemia: Diagnosis and Management
-
Slides Hyperlipidemia ChronicCare.pdf
-
Download Lecture Overview
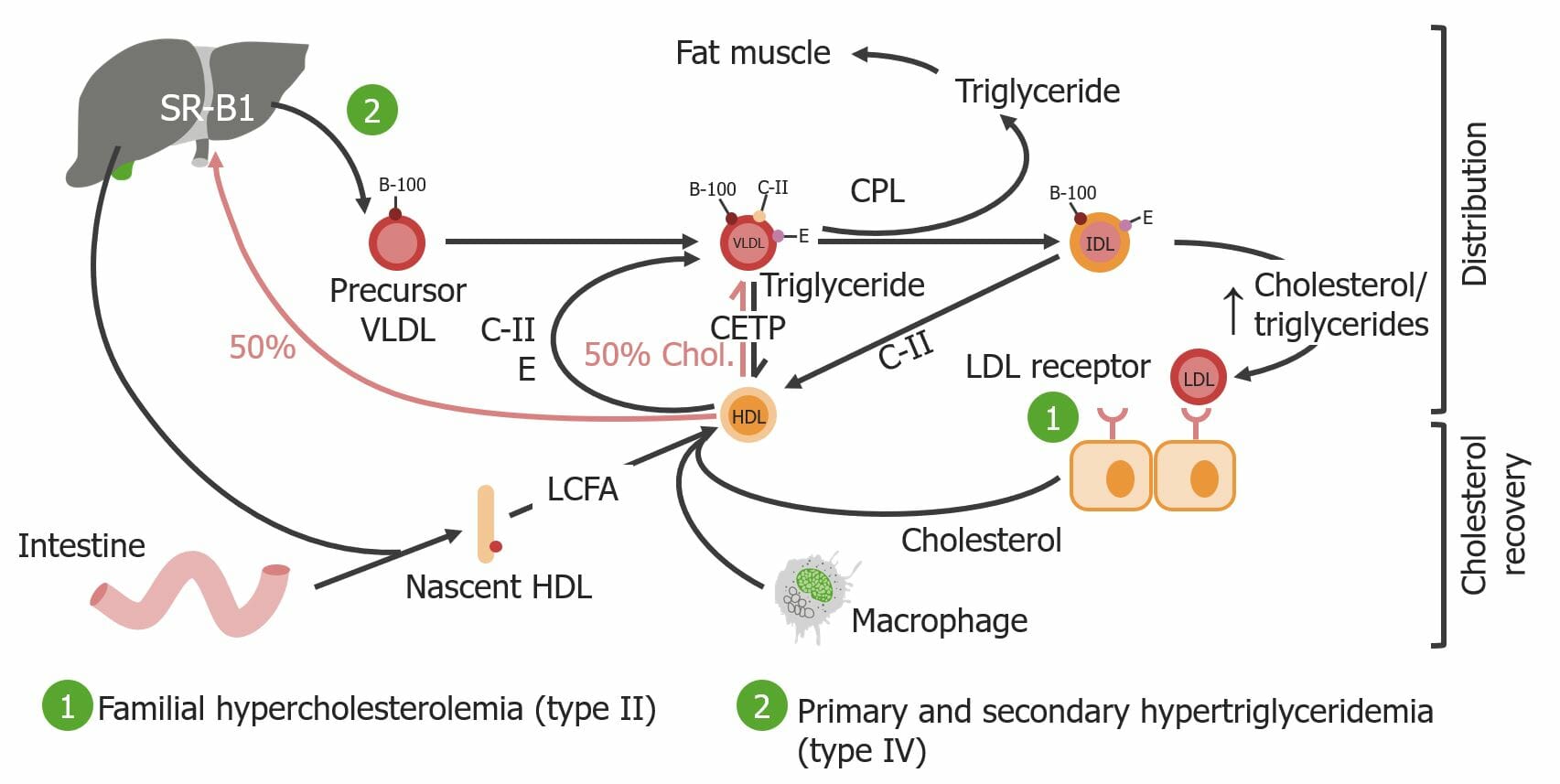
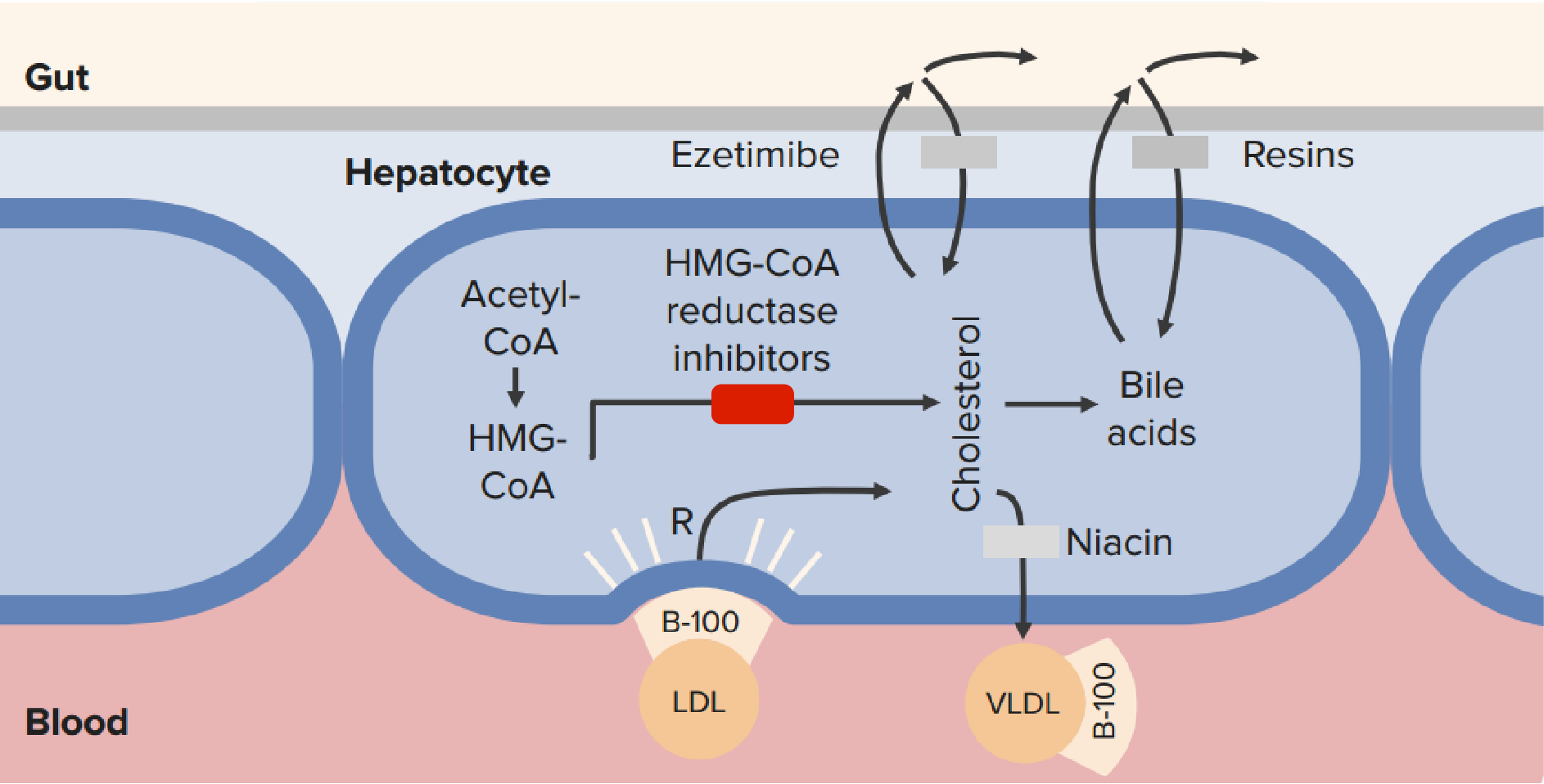
00:01 All right, everybody. 00:02 Grab your favorite fatty salty snack and let's talk about hyperlipidemia. 00:08 All right. 00:08 So, first, let's consider screening for lipid disorders and we’ll start with a case. 00:13 We have a 25-year-old man in for a health maintenance examination. 00:17 He has a body mass index of 31 kg/m². 00:21 That’s obesity. 00:22 And otherwise, his exam is completely normal. 00:26 So, what should you recommend to him regarding evaluating serum lipids. 00:30 No exam until he is at least 35 years old? No exam until he’s at least 50 years old? Evaluation now with a basic lipid panel? Or do you want to evaluate now with a lipid panel including lipoprotein(a) and apolipoprotein-B? What do you think? Current guidelines from our US Preventive Services Task Force would say evaluate now with a basic lipid panel. 00:53 Let’s go over some of those guidelines. 00:55 So, recommended is that men between 20 and 35 years of age and women 20 to 45 years of age get screened with a basic lipid panel if there is increased risk of coronary heart disease, if there's any risk factor present. 01:09 What are those risk factors? How about obesity? This patient has that. 01:12 So, check. He is in the pool. 01:15 Smoking. 01:16 Family or personal history of coronary heart disease. 01:19 Diabetes, of course. 01:20 And hypertension. 01:22 So, those are all risk factors. 01:24 What else does USPSTF say? Well, when you're 35 years old and male, you should be routinely checked. 01:32 For women above 45 years of age, they should be routinely checked as well for serum lipids. 01:38 How often they should be checked is unclear. 01:40 And that's kind of nice because in my clinical practice I have patients who are borderline who I want to check on an annual basis. 01:47 I have patients who clearly have low cholesterol levels thanks to their lifestyle and their genes and, therefore, I don't need to screen them very often at all, maybe every five years or so. 01:59 But, yeah, the right interval for screening is not evidence-based. 02:04 And so, it really comes up to you as a patient. 02:08 They also found that there was insufficient evidence to recommend for/against screening for lipids among children and adolescents. 02:16 Now, that's interesting, but it contrasts with recommendation from the American Academy of Pediatrics, which says, all children should be screened around the age of 9 and 10. 02:27 I split the difference and I'll certainly target overweight and obese children. 02:32 I’ll recommend them for screening lipids as well as thinking about glucose levels for those children as well. 02:39 So, what do you do with the results? Well, currently, the American Heart Association has gone to a more holistic approach to the evaluation of lipids. 02:48 It's not based just on number values anymore. 02:50 In fact, it incorporates multiple facets of a person's sociodemographic and disease profile to create a score, a 10-year risk for cardiovascular disease. 03:01 So, what I recommend – and I actually like this approach. 03:04 Being a family physician and a holistic practitioner myself, it's not only the current recommendations. 03:10 I think it actually is a little bit more evidence-based and it allows me to really more aggressively treat patients with lipids and, therefore, prevent more heart attacks and strokes. 03:22 What are the components of this risk calculator? Which you can download for free and use it on – I use mine on my phone. 03:29 So, it's demographics, age, sex and race. 03:32 Then there are measurements of cholesterol. 03:34 So, you need a baseline cholesterol to put that information into the calculator. 03:38 You have to state whether the patient has hypertension, whether it’s treated, if they have diabetes, their smoking status and the systolic blood pressure. 03:45 It takes about a minute at most to put the information in and get a 10-year predictive cardiovascular risk. 03:53 Linked to that is another site that tells you, based on the information given, here's what's recommended in terms of statin therapy. 04:05 Everybody who has some elevation of cholesterol or cardiovascular risk factors that I mentioned earlier should be thinking about low-fat diet and exercise. 04:16 It’s associated with about a 15% reduction in LDL with lifestyle changes as well as an 18% reduction in triglycerides. 04:26 It also increases HDL by about 14% maximum. 04:30 So, lifestyle definitely has a role. 04:34 And in terms of statin therapy, if you want to broadly compare high-intensity statins – and that’s something along the lines of atorvastatin, rosuvastatin at a higher dose. 04:44 They can be expected to reduce LDL cholesterol by a maximum of about 50% with high-intensity statins. 04:51 Moderate intensity statins, which may include those two drugs at a lower dose or drugs like pravastatin or simvastatin at the highest dose, 30% reduction. 05:01 And then lower intensity statins can be expected to reduce LDL by a maximum of about 20%. 05:09 So, where are these drugs applied? High-intensity – and this is where I think – if you’re going to get questions on these guidelines, this is where they’re going to come from. 05:16 High intensity statins are employed, anybody with a history of cardiovascular disease. 05:22 That’s prior stroke, prior revascularization procedure. 05:26 That is truly where statins do their best work and the best evidence is in – not in primary prevention of cardiovascular disease, secondary prevention – preventing that next episode from happening. 05:37 So, they should absolutely be on a high intensity statin unless they have a severe contraindication. 05:42 Those with really high LDL levels, which may indicate some type of familial hypercholesterolemia, and then those patients who fit in this broad category, they have diabetes, they have a moderate LDL increase at least, and they've got a increased ten-year cardiovascular risk above 7.5%. 06:01 I can tell you from lots of patients who fit these criteria that most patients with diabetes will qualify for high-intensity statins based on those criteria right there. 06:11 Moderate intensity statins is for patients who can't tolerate a high intensity statin. 06:16 That makes sense. 06:17 And also those diabetes patients, the rare ones, who tend to be a lot younger because you don't see that many heart attacks in 32-year-olds, those are the ones who may just take a moderate intensity statin versus a high-intensity. 06:30 And low intensity statin, those are patients who kind of fit on the borderline with some mild increase in their ten-year cardiovascular risk, but they don't have diabetes and they don't have prior cardiovascular disease. 06:45 That’s how it breaks down. 06:48 A few notes on lipid management. 06:50 It’s no longer necessary to routinely monitor transaminase levels. 06:54 If patients develop symptoms, feeling fatigue and certainly feeling myalgias, it’s a good idea to check transaminase levels when they’re on statin therapy, but routine evaluation is no longer necessary. 07:09 And patients can continue taking their statin all the way up till when their liver enzymes rise to three times above the normal limit. 07:19 At that point, it’s time to make a change. 07:22 Also, it’s not as necessary to routinely monitor lipid levels. 07:26 If you have a patient who is on the highest dose rosuvastatin or atorvastatin, there's not much else you can do if their LDL doesn't fall into the old goals. 07:35 However, for patient adherence, it can be useful to check lipid levels, and just ask, are you taking your statin because I see despite intensive therapy, your LDL is 140, that doesn't compute for most patients. 07:47 Then you find out, lo and behold, they only take it once a week. 07:50 I hear that regularly. 07:52 And, of course, reassess that cardiovascular risk every four to six years because they may change from needing a low or moderate intensity up to a higher intensity statin. 08:03 Now, there are a new class of drugs that have been out in the market for a couple years. 08:07 These proprotein convertase – and I can't pronounce it. 08:11 I call them the pesky nine inhibitors for familial hypercholesterolemia. 08:16 Now, these drugs are now being promoted beyond familial hypercholesterolemia. 08:21 They have been associated with a reduction in cardiovascular death and they are stronger in terms of LDL reduction. 08:27 We’re talking 70, up to 80% reduction, severe falls in the total LDL cholesterol, beyond what you can get with a statin alone. 08:39 And so, therefore, these drugs will become promoted for the prevention of cardiovascular disease in a broader population, but they are significantly more expensive. 08:49 It’s something to consider. 08:52 What about patients who can't tolerate a statin? The most common reason patients can't tolerate statins is myalgia. 08:58 Remember that myalgias with statin tends to affect the larger muscle groups. 09:02 It just feels like a dull ache. 09:04 It often happens after initiation of treatment or increase in dose, but it can emerge at any time during treatment. 09:12 And so, there's some simple rules, though. 09:15 You want these drugs, which really do make an impact on cardiovascular disease, onboard as much as possible. 09:22 So, here's what I would recommend. 09:23 First, change the statin. 09:25 Just simply changing the statin to a different type. 09:27 So, they were on atorva, now they take rosuva. 09:30 They were on simva, now they take prava. 09:33 So, changing your statin works in about a third of the time. 09:37 Changing the class of statin, moving from that high intensity to a lower intensity statin can be helpful. 09:43 Then we’re talking about lowering the dose of statin. 09:46 Now, you're making some compromises. 09:48 If they really need to be on high intensity, not everybody can tolerate that, but at least keep them on something. 09:53 Something is always better than nothing. 09:55 And at the end of day, if it takes every other day dosing of the statin, that’s still better than nothing. 10:01 That’s still better than – especially with a history of cardiovascular disease. 10:07 And in those patients who really can't tolerate a statin in any way, shape or form, who have a history of cardiovascular events, that's where I think those pesky nine inhibitors can make a difference.
About the Lecture
The lecture Hyperlipidemia: Diagnosis and Management by Charles Vega, MD is from the course Chronic Care.
Included Quiz Questions
Which of the following is the most appropriate first step for the management of a patient who has developed myopathy (other than rhabdomyolysis) on high-dose atorvastatin?
- Try switching to rosuvastatin
- Decreasing the dose of atorvastatin
- Switching to simvastatin and rosuvastatin simultaneously once symptoms resolve off statins
- Discontinuing statin therapy
- Treating with glucocorticoids
A 24-year-old woman presents for a routine visit. She feels well and has no history of a serious illness. She has a BMI of 22 kg/m2, blood pressure of 120/74 mmHg, and a heart rate of 78/min. What are the USPSTF recommendations for lipid screening in this patient?
- No screening is required.
- Total cholesterol and triglyceride
- Total cholesterol
- Total cholesterol, triglyceride, high-density lipoprotein, and low-density lipoprotein
- Low-density lipoprotein
Which of the following patients is least likely to require lipid screening?
- A 38-year-old female with a BMI of 22 and a blood pressure of 125/75 who has no history of a serious illness
- A 21-year-old woman with a BMI of 21 and normal vital signs whose father had myocardial ischemia at the age of 55
- A 38-year-old man with a BMI of 23 and a blood pressure of 155/75
- A 32-year-old man with a BMI of 27 who has a 4-pack-year smoking history
- A 42-year-old woman with a BMI of 27 who has polycystic ovarian syndrome and a HbA1c of 6.8
Which of the following lipid-lowering medications is most appropriate for secondary prevention of cardiovascular disease?
- Atorvastatin
- Simvastatin
- Pravastatin
- Lovastatin
- Fluvastatin
Which of the following is the most important indication for monitoring patients on high-intensity statin therapy for secondary prevention of cardiovascular disease?
- Evaluation of compliance with therapy
- Evaluation of drug efficacy and Screening for adverse effects
- Evaluation of drug efficacy
- Screening for adverse effects
- None of the options provided are correct.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |