Playlist
Show Playlist
Hide Playlist
Hyperaldosteronism
-
Slides Hyper-Hypo-Aldosteronism EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
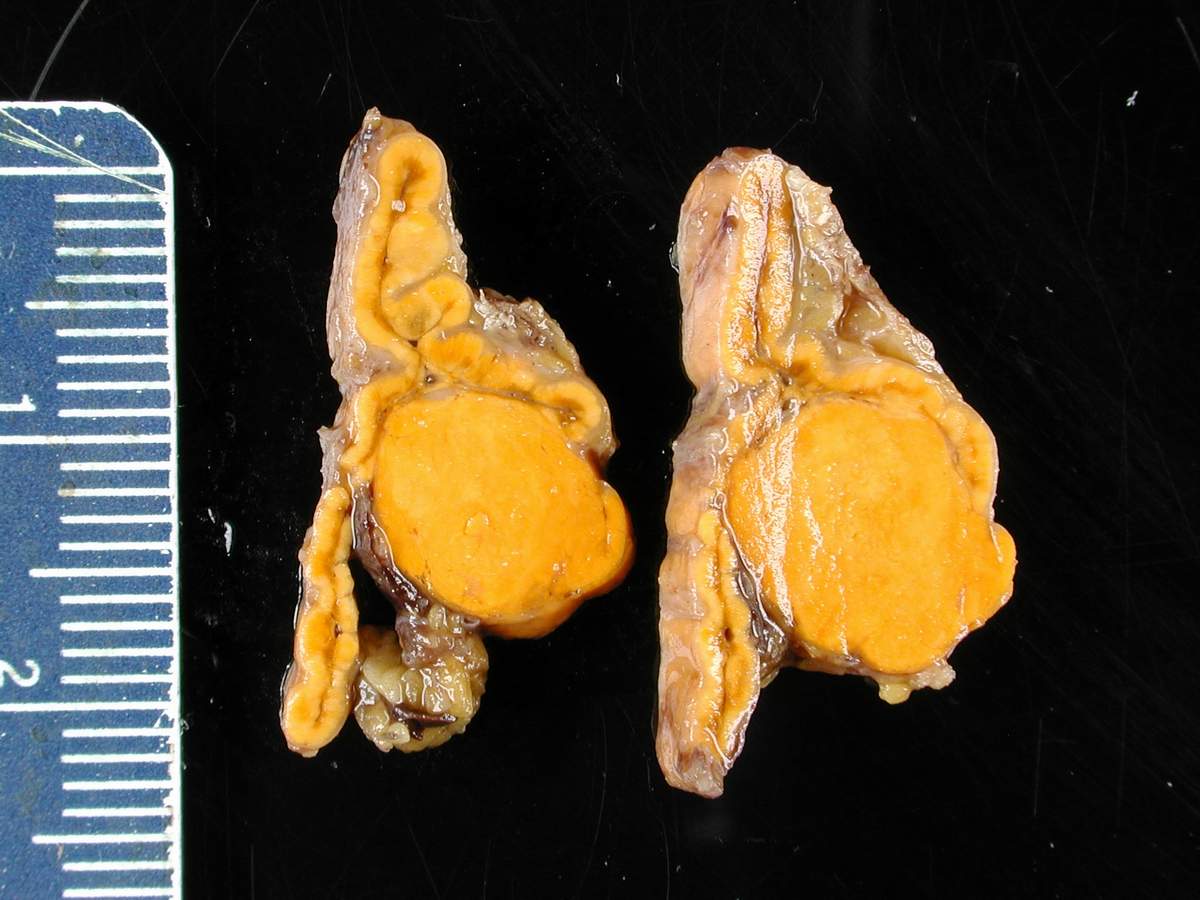
00:01 What’s adrenal gland pathology? Our focus here will be aldosterone, hyper and hypo. 00:06 I highly recommend that you go back and review your physio because I will go through this rather quickly, expect you to know the basic functioning of aldosterone so that we can walk through the path effectively. 00:18 Our topic here is hyperaldosteronism. 00:21 Before we begin, you automatically start thinking about what’s going on with your patient. 00:27 There’s going to be increased reabsorption of sodium, doesn’t matter if it’s primary or secondary. 00:33 In addition, there’s increased reabsorption of water, thus you’ll have increase in blood pressure. 00:38 Next, what does aldosterone do with potassium? It gets rid of it, you secrete it. 00:44 If there’s too much aldosterone, either primary or secondary, your patient is suffering from hypokalemia, your potassium level will be less than 3.5. 00:53 Next, what do you do with hydrogen? Or what does aldosterone do with hydrogen? It secretes it, it gets rid of it. 01:01 If you get rid of hydrogen, your PH is going to increase, your patient is in a state of alkalosis. 01:09 What is primary and secondary? Well, primary hyperaldosteronism will be a specific tumour in the zona glomerulosa that is only producing aldosterone… welcome to Conn’s syndrome. 01:25 What is it going to do to your blood pressure? It is going to increase it. 01:30 Now, be careful, this blood pressure that you’re increasing, obviously called hypertension, is it primary or secondary, do you remember? Secondary. 01:43 In the United States, a very common cause of secondary hypertension is primary hyperaldosteronism. 01:50 Interesting, isn’t it? Do not ever forget that. 01:58 Bilateral adrenal hyperplasia, what’s happening here? Well, here, you might have increased production of aldosterone by your adrenal cortex, specifically the zona glomerulosa. 02:15 If you were to find increased levels of aldosterone primarily, what is its feedback mechanism? Do not focus upon ACTH clinically, you are going to be focusing upon plasma renin activity, PRA. 02:30 Therefore, if there’s increased aldosterone primarily causing secondary hypertension, there will be a decrease in rennin. 02:38 Is that clear? You’ll have increased reabsorption of sodium as mentioned above 145, you’ll have a decrease in potassium level plasma less than 3.5 and because you’re getting rid of hydrogen, your patient is in a state of metabolic alkalosis. 02:57 What about secondary, how does secondary work? All secondary would mean is that, let’s say that your patient has some type of renal artery stenosis. 03:09 What do you mean some type? If I give you a 67 year old male in which, upon physical examination, you hear renal bruits. 03:20 Well, that would be atherosclerosis of the renal artery, correct? Resulting in renal artery stenosis, what then happens? Decreased profusion through the afferent arteriole. 03:33 What is then elevated here? Renin, what’s next? Aldosterone, ah, welcome to secondary hyperaldosteronism. 03:42 It wasn’t primary; the inciting event was decreased profusion to the kidney. 03:50 What else may then cause it? Take a look at the examples here. 03:53 CHF, congestive heart failure, you will then find increase amounts of fluid in your interstitium. 04:00 There will be a decreased profusion through the afferent arterial, you’d be increasing your renin and therefore causing secondary hyperaldosteronism. 04:11 Remember, in congestive heart failure, it’s a vicious cycle, especially if there is right sided heart failure, what does your patient look like? Peripheral edema. 04:23 This relationship is completely the opposite of primary. 04:27 Please locate the relationship between renin and aldosterone in primary. 04:33 Increased aldosterone, decreased renin in primary; in secondary, increased renin, increased aldosterone… secondary hyperaldosteronism. 04:43 What kind of hypertension is this? Secondary hypertension. 04:49 You see as to how language becomes really important for you in medicine, right? So, both primary and secondary hyperaldosteronism is causing what kind of hypertension? Secondary hypertension. 05:03 That must be understood. 05:06 Edema, hypertension, low potassium and alkalosis, the major factor here or sign that you did not see in primary hyperaldosteronism was the edema caused by congestive heart failure caused by cirrhosis caused by nephrotic syndrome, right? In those conditions, don’t you find edema, decreased profusion through the afferent arterial, out comes renin and secondary hyperaldosteronism. 05:39 Let’s screen for primary hyperaldosteronism. 05:44 Plasma aldosterone concentration, PAC, you want to memorize greater than 15 nanograms, you do that on your own time, but you know that it’s already elevated. 05:55 Concept first then memorization. 05:59 In primary hyperaldosteronism causing secondary hypertension, where is my lesion? Is it throughout the cortex of the adrenal or only in the zona glomerulosa? That’s a very important question because that gives you two different diagnoses. 06:17 Where is the adenoma located here? Good, only in the zona glomerulosa. 06:23 Give me the diagnosis, if I put the adenoma… not me, but if pathology puts an adenoma in the adrenal cortex as a whole, that gives you Cushing’s, right? That gives you Cushing’s… simple questions makes you think, that’s what the exam is all about, not about memorization. 06:43 So, here, we have an increase in aldosterone and a decrease in renin, take a look at the ratio here. 06:51 Obviously, your plasma aldosterone concentration is much higher than the plasma renin activity, that ratio will be increased. 07:03 Confirmation of diagnosis, how do you confirm primary hyperaldosteronism? Non-suppressed 24 hour urine aldosterone after oral salt loading or non-suppressed plasma aldosterone concentration after IV saline infusion. 07:22 Be smart about how do you use your test. 07:25 Shouldn’t you be suppressing aldosterone if you inject your patient with fluid? Yes. 07:31 What if it doesn’t happen or what if you give oral salt then what should you be doing to your aldosterone? Obviously suppressing it. 07:42 Doesn’t this sound an awful lot like oral glucose tolerance test? And we had done this for acromegaly. 07:51 If you missed that concept, make sure you go back and take a look at OGTT and acromegaly. 07:56 Here, we have oral salt and aldosterone confirmation. 08:01 In unclear cases, adrenal vein sampling can help distinguish unilateral from bilateral sources of excess aldosterone. 08:10 Do not forget that. 08:12 Adrenal vein sampling may help you distinguish between uni and bilateral… an important slide for screening, confirmation. 08:24 If you take a look at this picture of aldosterone, haha, by that I mean, you can’t tell by looking at this picture per se that it’s aldosterone. 08:35 But, you can definitely tell by looking at this picture that, my goodness, there is an adenoma in the adrenal. 08:42 So, what are you looking for? You will be given more information. 08:48 Maybe there’s secondary hypertension, maybe there is decreased potassium and alkalosis without any effect of Cushing. 08:54 So, therefore, this is Conn. 08:58 If you find a adenoma such as this and your patient has moon facies, buffalo hump, trunk obesity then that would be Cushing, clear? Things are becoming really interesting for you, aren’t they? Primary hyperaldosteronism… surgery for unilateral source adenoma, use of aldosterone antagonists… welcome to your spironolactone or eplerenone. 09:26 Remember that these are drugs or they’re potassium sparing drugs, aren’t they? If you antagonize your aldosterone receptors, obviously you’re going to hold on to your potassium, but here, we’re using for purposes because you want to block the effects of the excess aldosterone for bilateral sources, hyperplasia; unilateral surgery bilateral antagonists.
About the Lecture
The lecture Hyperaldosteronism by Carlo Raj, MD is from the course Adrenal Gland Disorders.
Included Quiz Questions
What is NOT associated with primary hyperaldosteronism?
- Hyponatremia
- Hypertension
- Metabolic alkalosis
- Hypokalemia
- Decreased renin
What is NOT a cause of primary hyperaldosteronism?
- Renal ischemia
- Conn syndrome
- Aldosterone producing adenoma
- Bilateral adrenal hyperplasia
- Adrenal carcinoma
What is the difference in the presentation between primary and secondary hyperaldosteronism?
- Edema
- Secondary hypertension
- Hypokalemia
- Alkalosis
- Hypernatremia
What is a screening test for primary hyperaldosteronism?
- Plasma aldosterone concentration over 15 ng/dL
- Non-suppressed 8-hour urine aldosterone after salt loading
- Non-suppressed plasma aldosterone concentration after diuretic loading
- Suppressed plasma renin activity over 20 ng/dL
- Non-suppressed plasma aldosterone concentration after beta-blocker loading
What is the preferred treatment for a unilateral adenoma causing primary hyperaldosteronism?
- Surgery
- Spironolactone
- Eplerenone
- Megestrol
- Methotrexate
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |