Playlist
Show Playlist
Hide Playlist
Human Immunodeficiency Virus (HIV) – Retroviruses
-
02-43 Retrovirus DLM.pdf
-
Download Lecture Overview
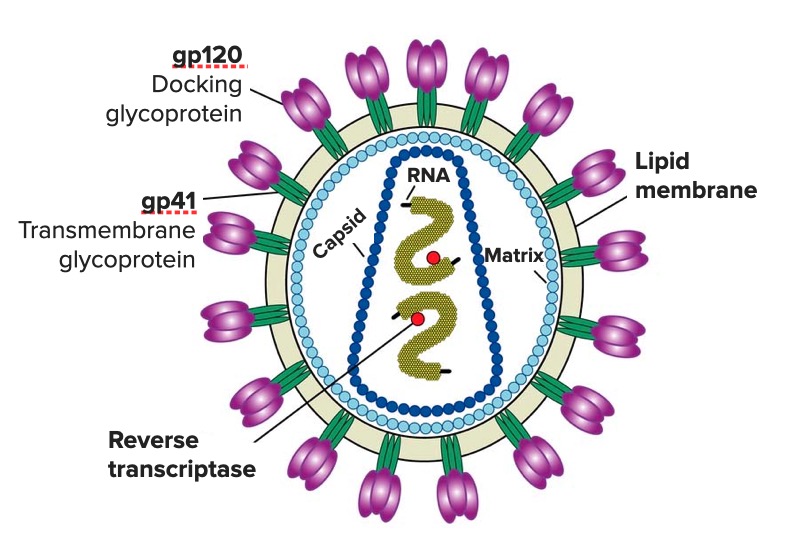
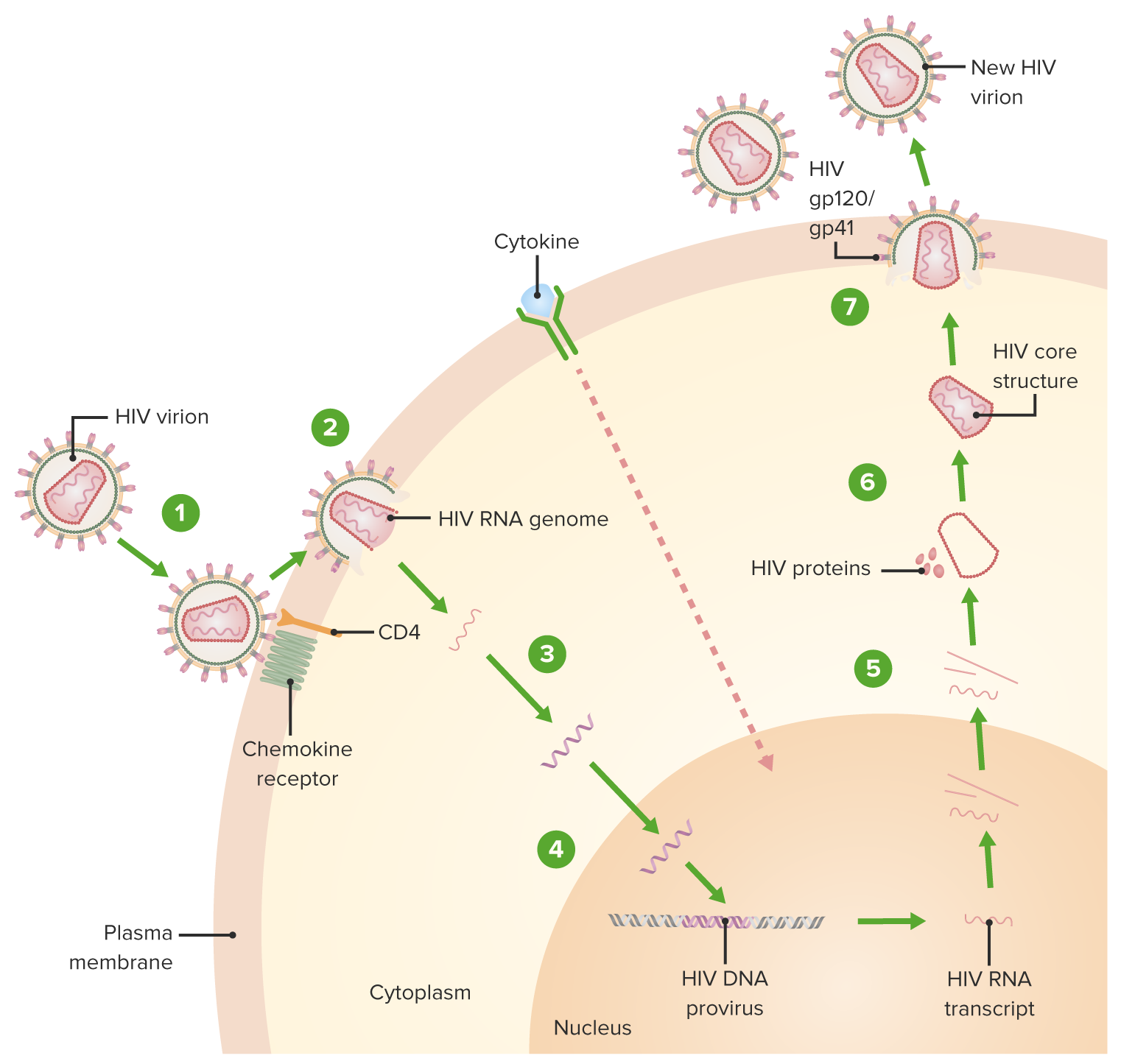
00:01 So, let's walk ourselves through the lifecycle of the human immunodeficiency virus as it is the best example for retroviral life. 00:11 We start at the top with the attachment process in which the virus, through its envelope proteins, binds to specific receptors, in this case, CD4 and other cell differentiating markers, chemokine receptors, and coreceptors on the surface of the CD4 T lymphocyte. 00:30 The attachment is the first part, and then, almost like drawing oneself in through a tow rope by doing waterskiing, the fusion process occurs. It brings the virus in to a further and firm attachment, allowing the envelope of HIV to merge with the cell membrane of the CD4 T lymphocyte. 00:50 Macrophages and dendritic cells are also infected once inside the host cytoplasm. 00:55 The RNA genome of the virus undergoes reverse transcription by means of its reverse transcriptase, synthesizing first a hybrid RNA slash DNA and then a double stranded complementary DNA, also known as cDNA or pro viral DNA in quiescent or non dividing T lymphocytes. 01:15 The HIV complementary or cDNA may remain in the cytoplasm in a linear episode of form. 01:22 However, in dividing T lymphocytes, the cDNA circular rises enters the nucleus and then integrates into the host genome. 01:31 After integration, the pro virus MAI may either stay as latent infection in a pro viral state lasting for months, years, perhaps even decades. 01:40 Or it may be suddenly it may become productive transcribing and expressing its own genome which has the potential to produce new virus that transcribed HIV, RNA that exits the nucleus and can synthesize HIV proteins and the virion cores along with the P24 Capsid. 01:59 And these are assembled into a nascent virion. 02:04 The virion then or core virion, exits the cell with lipid bilayer from the host membrane that is studded with viral glycoproteins gp41 and gp120. 02:17 Productive infection with as just described with this extensive viral budding leads to the death of the infected cell HIV usually enters through the anal genital mucosa or tonsils or tissue. 02:30 The viral envelope protein GP-120 binds to the CD4 molecule and dendritic cells to enter the macrophage, GP-120 must bind to the chemokine receptors CCR five as well as CD4 The HIV infected cells, then fuse with CD4 T lymphocytes spreading the infection. 02:51 So, it's a very complicated structure. 02:54 Something like this probably occurs in many other viruses. 02:57 We happen to know so much because HIV has been a target of extreme scrutiny with research to discover, not only how it does what it does, which is so severe, but also how to try and prevent it. And that's the difficult step. 03:11 So, transmission of HIV. 03:14 Probably quite well known to you, but it is blood and body fluids. So blood, semen, vaginal fluid, if there's bleeding involved, transfer from mother to baby. 03:24 The whole 9 yards, unfortunately, it's quite contagious if the patient has a high viral load, meaning a high number of HIV viruses, which are currently circulating in the bloodstream. 03:37 So, let's look at the pathogenesis. 03:39 And again, keep in mind that the principal problem is that HIV targets the CD4 T lymphocyte, which is the helper T lymphocyte. 03:48 This is the one, in a way, responsible for controlling, suppressing, directing, activating the entire rest of the adaptive immune system, humoral immunity included. 04:01 So, your target cells are the T lymphocytes, and their interaction with the dendritic cells, the macrophages, which initially present HIV to the target. 04:11 As one of the downstream effects, the production of pro-inflammatory cytokines, such as interleukin-2 is reduced, is prevented because the T lymphocyte, the CD4 T lymphocyte, is now being targeted and unable to interact constructively with its partner in crime, the CD8 T lymphocyte, which is a cell or a cytotoxic T lymphocyte. 04:35 This means that patients with HIV infection are susceptible to additional viruses, not just HIV. 04:42 Similarly, the inhibition of release of interferon gamma, another pro-inflammatory cytokine, compromises macrophage activation, and there goes yet another phagocytic part of the immune system. 04:57 So patients are now susceptible to both fungi and bacteria. 05:00 As we said before, it's very difficult for us in medical science to counteract HIV infection. 05:07 But in addition, there are human factors as well. 05:10 For example, the virus replicates itself within an immune cell, so you can't just knock out the immune cell or else we'll accomplish with the virus has been trying to do in the first place. 05:21 In addition, there are known to be immunologic reservoirs or sequestra where the virus can replicate, and we can't get access to it even with very active antiretroviral therapy. 05:34 Plus, the virus can go latent in many of the CD4 T lymphocytes, and that allows it to be quiet and evade immune detection until later in the lifecycle of the virus. 05:46 And then finally, as I've mentioned already, the virus itself has multiple changes in its antigen expression via mutations, so it's a shifting target. 05:55 So, HIV is incredibly complex and, of course, incredibly challenging for scientists and healthcare providers to try and get a sense of and try and get on top of. 06:07 Let's look now at the clinical course of HIV, and it's best shown by this graph. 06:14 In the green line will be the number of CD4-positive T lymphocytes, the target of HIV infection. 06:22 The red line, then, is the viral load, which is the number of HIV RNA copies expressed per milliliter in blood. 06:29 If one then starts at the beginning of infection and primary infection at around 1 to 2 weeks after exposure, there is an initial precipitous drop in the number of CD4 cells, at the same time as the number of HIV RNA genome particles increases exponentially. 06:51 And that is seen in the shaded green bar in which acute HIV infection is occurring. 06:57 Patients during this time may experience what's called acute retrovirus syndrome or acute HIV syndrome. 07:04 And this is very much like a nonspecific, but very severe flu-like illness. 07:10 So, fever, malaise, myalgias, arthralgias. 07:14 Many times there is an erythematous maculopapular rash. 07:18 Many times, there is a leukopenia, so a low white blood cell count. 07:23 One might not yet see, though, a lymphopenia, because until the number of CD4 lymphocytes drops to a significant amount by maybe 6 weeks in, there may not be a discernible change in the number of lymphocytes circulating in the periphery. 07:39 In addition, thrombocytopenia, hepatitis, generalized lymphadenopathy, the whole body's immune system has gone wild as its principal modifier has been targeted. 07:50 After this acute process, typically lasting up to about 9 weeks after initial infection, there's a stabilization. So, the number of CD4 cells starts to increase under production by the body, and at the same time, the HIV virus starts to go latent to avoid immune detection. 08:10 And one can go months to years, in fact, frequently, many years before there's a reactivation, if you will. 08:18 So, the period of latency or clinical latency can last for quite some time, and during this time, the patient may be completely asymptomatic. 08:26 At the worst, they may have some fatigue, or just a general sense of not well-being. 08:32 But after a certain point, activation occurs, and what triggers that point is yet unclear to medical science. 08:40 It may be a combination of physiologic stressors, it may be just finally a time when production of CD4 lymphocytes finally is unable to keep up with that slow, gradual destruction of lymphocytes. 08:52 At any point, the number of CD4 cells finally drops below a critical level. 08:56 The patient now is at risk for opportunistic infections, and they can be anything which we'll cover shortly. 09:02 And at the same time, the viral load, the number of HIV RNA copies, skyrockets, as you see as the red line just shoots straight upwards. 09:11 After a certain point, death occurs, not from HIV, but from an opportunistic infection, which is completely unable to manage in the absence of an immune response.
About the Lecture
The lecture Human Immunodeficiency Virus (HIV) – Retroviruses by Sean Elliott, MD is from the course Viruses.
Included Quiz Questions
Which of the following serve as primary target cells for the human immunodeficiency virus? Select all that apply)
- Helper T cells
- Cytotoxic T cells
- Natural Killer T Cells
- Macrophages
- Dendritic cells
During the course of infection by the human immunodeficiency virus, which of the following is formed initially as a result of action of reverse transcriptase?
- RNA-DNA hybrid
- Complementary dsDNA (cDNA)
- Messenger RNA (mRNA)
- Double-stranded viral DNA (dsDNA)
Inhibition of the release of which of the following pro-inflammatory cytokines compromises macrophage activation, rendering the individual infected by human immunodeficiency virus susceptible to fungal and/or bacterial infections?
- Interferon-gamma
- Interleukin-2
- Interleukin-1
- Tumor necrosis factor-alpha
- Monocyte inflammatory protein
The typical duration of acute human immunodeficiency virus syndrome after initial infection is...?
- ...up to 6 weeks.
- ...up to 10 weeks.
- ...up to 3 weeks.
- ...up to 12 weeks.
- ...up to 15 weeks.
The assembly of the nucleocapsids along with two genome copies of the human immunodeficiency virus takes place within the...?
- ...cytoplasm.
- ...nucleus.
- ...endoplasmic reticulum.
- ...Golgi bodies.
- ...mitochondria.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |