Playlist
Show Playlist
Hide Playlist
Hormonal Regulators: PTH and Vitamin D – Bone and Calcium Medications
-
Slides Hormonal Regulators PTH Vitamin D Bone Calcium Medications.pdf
-
Reference List Pharmacology.pdf
-
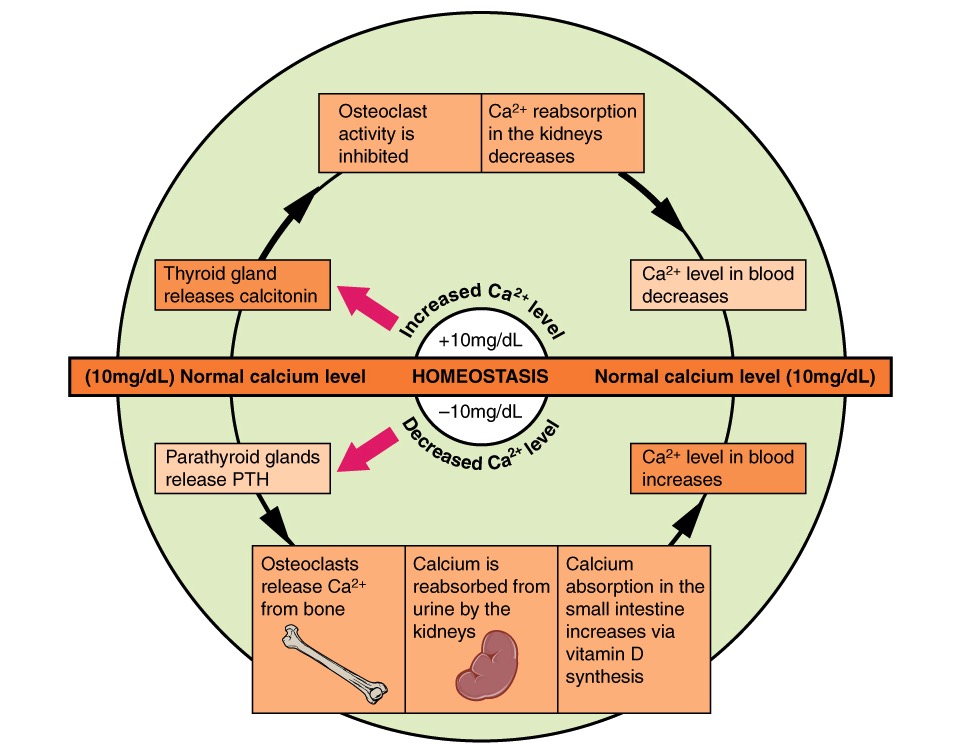
Download Lecture Overview
00:01 Welcome to Pharmacology by Lecturio. I'm Dr. Shukla, and today we're going to cover bone and calcium pharmacology. Now when we talk about bone and calcium pharmacology, we have to understand some of the regulators of bone mineral homeostasis. Homeostasis is essentially a big word that means keeping things the same. Now the bone is constantly rebuilding itself and all of these modulators can have an effect on the way the bone rebuilds itself. 00:30 Because bone is mostly made out of calcium, anything that happens that affects the way that the bones are metabolized will affect your serum calcium levels. Now let's focus on PTH, which is parathyroid hormone and vitamin D. 00:46 Now remember that a drop in free calcium levels will stimulate parathyroid hormone release from the parathyroid glands. Any active metabolites of vitamin D play a secondary role in inhibiting the secretion of parathyroid hormone. So that's important to remember when we're giving drugs. 01:07 For example, in different organs, you can have different activities of both parathyroid and vitamin D. In the intestine, parathyroid hormone will indirectly increase calcium and phosphate absorption. Now it'll also increase, do this by increasing vitamin D metabolites. Now active vitamin D metabolites themselves increase calcium and phosphate absorption in the gut. In the kidney, the parathyroid hormone will cause decreased calcium excretion. Now that makes sense because you want to maintain calcium levels in the body when you have parathyroid hormone. However, your parathyroid hormone will also increase phosphate excretion. So your phosphate levels will go down because of kidney excretion with parathyroid hormone. In terms of active vitamin D metabolites, you get an increased reabsorption of calcium and phosphate, but usually there's a net increase in urinary calcium due to the effects in the GI tract and bone. The activity of parathyroid hormone in the bone is complicated. First of all, there's a difference between continuous high doses of parathyroid hormone and intermittent dosing of parathyroid hormone. So for example, in the bone, calcium and phosphate reabsorption is increased by continuous high concentrations of parathyroid hormone. Meanwhile, intermittent dosing decreases, resorption increases bone formation. So there's a completely opposite effect depending on how the parathyroid is administered. In terms of vitamin D metabolites, there's a direct effect on the bone. 02:46 It increases calcium and phosphate reabsorption from the bone and there's an indirect effect as well that first promotes mineralization by increasing the availability of calcium and phosphate. So it's a complicated mechanism in the bone. The net effect on serum levels of these two hormones is as such. With parathyroid hormone, serum calcium levels are increased and serum phosphate levels are decreased. With vitamin D metabolites, serum calcium and phosphate are both increased. So this is an important distinction between the two hormones and you need to understand that both in clinical practice and on your exams. I want to reiterate a point. 03:31 At continuous high doses of parathyroid, which are seen in hyperparathyroidism, the net effect is increased bone resorption, hypercalcemia, and hypophosphatemia. 03:42 At low intermittent doses of PTH, there is a net increase in bone formation. 03:47 This is why teriparatide, a recombinant truncated version of PTH, is used in osteoporosis. 03:55 Let's talk about vitamin D. So vitamin D, as you probably are well aware, is used in the treatment of rickets, osteoporosis, and osteomalacia, which is defective bone mineralization primarily due to vitamin D deficiency. 04:08 It is also given to patients with chronic kidney disease, malabsorption syndromes, and vitamin D deficiency, which is common, with more than 40% of adults in the USA being deficient in vitamin D. 04:22 Different women are typically given supplements. 04:25 It promotes calcium absorption from the gut, so you increase the amount of calcium being pulled out of food. 04:31 It also promotes bone resorption, which means that it maintains serum calcium levels, and it also promotes bone remodeling. 04:40 The image shows the deformed risk of a vitamin D deficient child with rickets who recovered after treatment. 04:47 The bone deformation is due to growth plate enlargement and bone softening from defective mineralization caused by vitamin D deficiency. 04:55 What are the extraskeletal benefits of vitamin D? It's become a very popular supplement, and part of that is based on real science. 05:03 Supplemental vitamin D is given to pregnant women because it is needed not only for fetal skeletal development, but also for organ maturation and immune function. 05:12 There's no benefit to very high levels of vitamin D or what we call super normal levels, but correcting low levels reduce fracture risk. 05:21 So giving more vitamin D in a person with normal vitamin D levels and normal bones will not make them super strong. 05:30 Now cancer risk may be worsened in patients who have low levels of vitamin D, but there's no good research to support supplementation in patients with normal levels. 05:40 So you're not going to reduce cancer risk in patients who have normal vitamin D levels. 05:45 And autoimmune disease can be made worse with low levels, which isn't surprising, but it's not prevented or treated with supplements if the patient has normal levels. 05:56 So if a patient has a normal vitamin D level, using vitamin D supplements really isn't going to benefit patients. 06:04 The following diseases are worsened by low levels but are not helped with supplements in patients with normal vitamin D levels. 06:12 Diabetes, depression, cognitive decline, pregnancy and preeclampsia, patients who have weight loss, inflammatory and bowel disease, multiple sclerosis, asthma, infections, HIV, and stroke and cardiovascular disease and hypertension. 06:34 So this is something that occupies the internet but not the thoughtful minds of careful doctors.
About the Lecture
The lecture Hormonal Regulators: PTH and Vitamin D – Bone and Calcium Medications by Pravin Shukle, MD is from the course Endocrine Pharmacology.
Included Quiz Questions
What is correct regarding the net effect of parathyroid hormone (PTH) and 1,25(OH)2VitD (an active vitamin D metabolite) on serum calcium and phosphate levels?
- 1,25(OH)2VitD increases both calcium and phosphate.
- 1,25(OH)2VitD increases calcium but decreases phosphate.
- PTH increases both phosphate and calcium.
- PTH increases phosphate but decreases calcium.
- PTH and 1,25(OH)VitD have a similar effect on calcium and phosphate.
What is the benefit of vitamin D supplementation in vitamin D-deficient individuals?
- Reduced fracture risk
- Improves glycemic control
- Treats depression
- Improves symptoms of multiple sclerosis
- Treats HIV
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very clear lecture. I was able to understand and relate the subject in a matter of hours. I recommend this lecture to third and fourth year medical students from Uruguay